Method Article
Techniques for Lower Trapezius Transfer Using Achilles Allograft in Irreparable Posterosuperior Rotator Cuff Tears
In This Article
Summary
Here, we describe a modified technique for lower trapezius tendon transfer using an Achilles allograft in the treatment of massive posterosuperior rotator cuff tears.
Abstract
The management of irreparable rotator cuff tears presents significant challenges, particularly in active individuals experiencing functional limitations, such as reduced forward elevation and deficits in both external and internal rotation. Traditional latissimus dorsi (LD) tendon transfer has shown effectiveness in reducing pain associated with posterosuperior cuff tears but often yields inconsistent functional outcomes. This is largely due to the LD's primary role as an internal rotator, which limits its capacity to restore normal shoulder biomechanics. To address these limitations, the lower trapezius (LT) tendon transfer, augmented with an Achilles allograft, has emerged as an alternative to enhance external rotation, leveraging the LT's line of pull, which closely resembles that of the infraspinatus muscle.
This protocol outlines a modified surgical technique for LT tendon transfer with Achilles allograft augmentation, detailing patient positioning, tendon harvest, graft preparation, arthroscopic passage, and fixation methods. The protocol emphasizes key anatomical landmarks to minimize neurovascular injury and enhance graft integration. Postoperative care includes a 3 month immobilization period followed by a structured rehabilitation program to facilitate functional recovery.
This procedure is indicated for a specific patient group requiring improved external rotation and is biomechanically advantageous over the LD transfer. Though additional studies are warranted to confirm its efficacy in broader patient populations, early clinical outcomes suggest that LT transfer with Achilles allograft could offer superior biomechanical alignment and improved external rotation.
Introduction
Irreparable rotator cuff tears in active individuals pose significant treatment challenges due to the resulting functional limitations, including diminished forward elevation and deficits in both external and internal rotation1,2,3. While tendon transfers were initially developed to treat permanent nerve injuries, they have since been adapted for the management of irreparable rotator cuff tears4,5.
The latissimus dorsi (LD) tendon transfer is traditionally used for reconstructing posterosuperior rotator cuff tears, providing substantial pain relief. However, functional improvements have been inconsistent6. Since the LD functions as an internal rotator, it does not fully restore the normal force dynamics of the glenohumeral joint7. Even in cases with successful clinical outcomes, limited electromyographic activity of the LD has been observed during shoulder abduction8,9,10.
To address these limitations, the lower trapezius (LT) tendon transfer11 has emerged as an alternative, specifically to enhance external rotation12. The LT muscle's line of pull and force vector more closely mimic those of the infraspinatus tendon10, which is often insufficient or absent in these patients. In 2009, Elhassan et al.13 first described the use of the LT tendon transfer, augmented with an Achilles allograft, for improving external rotation in patients with traumatic brachial plexus injury14. Since then, this technique has gained popularity in treating patients with massive irreparable cuff tears.
This article presents modified techniques for performing LT tendon transfer using an Achilles allograft. This approach offers a reliable method with the potential to improve outcomes in a select group of patients, particularly those requiring enhanced external rotation.
Protocol
This study was approved by the Ethics Committee of our institution and informed consent was obtained from all patients.
1. Patient positioning and surgical preparation (Figure 1)
- Position the patient in the beach chair position with a 40-60° incline.
- Position the patient close to the edge of the bed to optimize access to the medial border of the scapula14.
- Drape a wide surgical field to ensure proper exposure of the shoulder and scapula region.
- Apply an arm holder to provide a distal traction force to open the shoulder joint for better visualization.
2. Harvest the lower trapezius tendon ( Figure 2)
- Make a horizontal incision from the medial border of the scapula to the midpoint of the scapular spine. Use palpation of the scapular spine for accurate guidance. The wound is 5 cm long and 1 cm below the scapular spine.
- Utilize electrocautery to separate the middle trapezius (inserted at the superior surface of the scapular spine) and LT (inserted at the scapular spine dorsum) muscle fibers along the scapular spine directly.
- Halfway along the scapular spine, make a vertical incision downward and flip the soft tissue to reveal the tendon part of the LT.
- Tag both ends of tendon parts of the LT with two #5 nonabsorbable sutures in a Krackow stitch pattern.
- Perform a finger dissection between the LT and infraspinatus from the lateral to the medial part to allow tendon mobilization and to preserve the underlying spinal accessory nerve15.
NOTE: Maintain a distance of approximately 58 mm from the tendon insertion to the spinal accessory nerve to minimize injury risk16. - Control minor bleeding by rinsing with hydrogen peroxide-soaked gauze.
3. Achilles allograft preparation ( Figure 3)
- Select an Achilles tendon allograft without bone for graft preparation.
NOTE: If Achilles allograft is unavailable, consider a semitendinosus autograft as an alternative9,17. - Secure both tendon parts of the allograft using two braided sutures in a Krackow stitch pattern, creating four strands for secure fixation.
- Evaluate the graft for any signs of damage or imperfections before proceeding to ensure optimal strength.
CAUTION: Use gloves and sterile techniques to handle the graft to prevent contamination and infection18,19.
4. Arthroscopic portals preparation ( Figure 4)
- Establish a standard posterior viewing portal to assess the glenohumeral joint.
- Create an anterolateral portal for passing the allograft and a lateral portal for visualization and anchor placement.
- Release the rotator interval to improve mobility and prevent future joint stiffness20.
- Release the supraspinatus and infraspinatus tendons to evaluate the feasibility of a side-to-side repair with the allograft21. Suprascapular nerve release may also be considered22,23.
NOTE: Performing superior capsular reconstruction using the biceps tendon is optional.
5. Graft passage and fixation ( Figure 5)
- Extend a fingertip from the wound in the back into the glenohumeral joint between the infraspinatus fascia and scapular spine to ensure a clear pass way for tendon shuttling (Figure 5A).
- Shuttle one #5 nonabsorbable suture from the anterolateral portal to the open wound in the back, just posterior to the scapular spine (Figure 5B).
- Tie the two braided sutures fixing the Achilles allograft with the #5 nonabsorbable suture just passed through the shoulder joint, and shuttle it inside the joint (Figure 5C,D).
- Insert one lateral row anchor (knotless PEEK suture anchors) at the bicipital grove (Figure 5E) and one lateral row anchor at the greater tuberosity. Maximize the graft coverage of the whole supraspinatus and infraspinatus footprint (Figure 5F)24,25 .
- Repair the Achilles allograft with the remnant infraspinatus (Figure 5G) using two medial row anchors (Ti 5.0) (red dot) (Figure 5H). The two lateral row anchors just inserted (yellow dot) are also shown in Figure 5H. Perform four mattress sutures and tie them at the two medial row sutures.
- Test the graft by internally and externally rotating the arm, confirming excursion and tension along the medial side of the Achilles allograft.
- Securely weave the LT tendon with the Achilles allograft using Pulvertaft sutures at 45° abduction and 45° external rotation, ensuring firm integration26.
6. Postoperative protocol
- Immobilize the patient in a gunslinger brace for 6 weeks at 45° shoulder abduction and neutral rotation to prevent graft tension.
- Initiate passive range of motion exercises 6 weeks after surgery, with precautions against internal rotation and cross-body movements.
- Begin active motion exercises at 12 weeks post surgery, progressively advancing to strengthening exercises by month 4.
7. Preoperative and one-year image follow-up
- Obtain preoperative anteroposterior X-ray and MRI images (Figure 6A-C) for patients receiving lower trapezius transfer using Achilles allograft.
- Obtain one-year anteroposterior X-ray and MRI images follow-up (Figure 6D,E) for patients receiving lower trapezius transfer using Achilles allograft.
Results
The LT tendon transfer with Achilles allograft aims to restore external rotation and improve shoulder function in patients with irreparable rotator cuff tears14,21. Representative outcomes include improvements in external rotation strength, range of motion, and pain relief post surgery, with objective measurements taken during clinical follow-up27,28.
Patients generally demonstrate a significant increase in external rotation range of motion, with an average gain of 30-40° compared to preoperative measurements29,30. Muscle strength is restored to a minimum of muscle power grade 4 and higher31. Postoperative results improved the Disabilities of the Arm, Shoulder, and Hand (DASH) score. Both studies assessed the Subjective Shoulder Value (SSV) and observed an average increase of 25.8%30. Additionally, Valenti and Werthel32 documented a reduction in pain levels on the visual analog scale (VAS), with scores dropping from 7 to 2-a decrease of 5 points32. MRI imaging at the 6-month follow-up typically shows robust graft integrity without significant stretching or degeneration33. The Achilles allograft appears well-integrated with the lower trapezius tendon, maintaining appropriate thickness and signal intensity32,33. Electromyographic analysis may also confirm the recruitment of the LT during external rotation movements, supporting functional transfer34. Compared to traditional latissimus dorsi (LD) transfer35,36, the LT tendon transfer demonstrated more effective improvement in shoulder external rotation and comparable American Shoulder and Elbow Surgeons score, UCLA score, and VAS (Table 1 and Table 2)37.
Suboptimal outcomes, characterized by limited motion gains, inadequate strength, and persistent pain, suggest issues with graft tension or muscle activation. Careful surgical technique, appropriate patient selection, and adherence to postoperative protocols are critical for optimal results. Suboptimal results may require revision or alternative management strategies. Positive results are indicated by a substantial increase in external rotation, improved muscle strength, decreased pain scores, and enhanced functional scores. Well-maintained graft integrity on imaging and effective LT muscle activation confirm the protocol's success.

Figure 1: Patient positioning and surgical preparation. The patient is positioned in the beach chair position with an inclination of 40-60°. Proper exposure is ensured to adequately visualize and explore the medial border of the scapula (arrow) for the surgical procedure. Arrowhead pointing to the scapular spine. Please click here to view a larger version of this figure.

Figure 2: Harvesting of the lower trapezius tendon. A horizontal incision is made from the scapula's medial border to its spine midpoint, guided by palpation. The harvested lower trapezius tendon is secured with two #5 nonabsorbable sutures (arrowhead) in a Krackow stitch pattern. The asterisk indicates the lower trapezius. Please click here to view a larger version of this figure.

Figure 3: Achilles allograft preparation. An Achilles tendon allograft was prepared using two Fiberwire sutures (arrowhead) in a Krackow stitch pattern, creating four strands to ensure secure fixation. Please click here to view a larger version of this figure.

Figure 4: Arthroscopic portal preparation. Establish a standard posterior viewing portal, an anterolateral portal, and a lateral portal. Abbreviations: P = posterior portal; L = lateral portal; AL = anterolateral portal. Please click here to view a larger version of this figure.
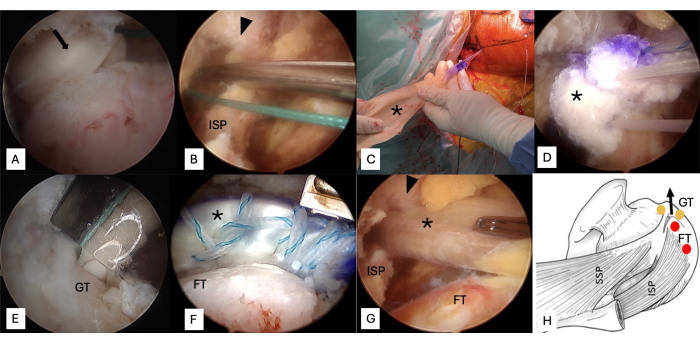
Figure 5: Graft passage and fixation. (A) Perform a finger dissection from the wound in the back into the glenohumeral joint between the infraspinatus fascia and scapular spine. (B) Shuttle one #5 nonabsorbable suture from the anterolateral portal to the open wound in the back, just posterior to the scapular spine. (C, D) Tie the two Fiberwires fixing the Achilles allograft with the #5 nonabsorbable suture and shuttle it inside the joint. (E) Insert one lateral row anchor at the bicipital grove and one at the greater tuberosity. (F) Maximize the graft coverage of the whole footprint. (G) Repair the Achilles allograft with the remnant infraspinatus. (H) Two medial row and two lateral row anchors are used. Arrow, fingertip; Arrowhead, scapular spine; Asterisk, Achilles allograft; Yellow dot, lateral row anchor; Red dot, medial row anchor. Abbreviations: GT = greater tuberosity; FT = supraspinatus footprint; ISP = infraspinatus. Please click here to view a larger version of this figure.
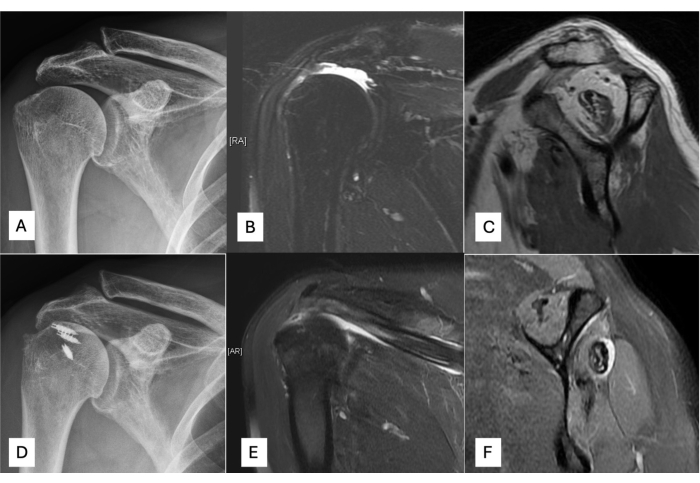
Figure 6: Preoperative and one-year image follow-up for patients with irreparable rotator cuff tears receiving lower trapezius transfer with Achilles allograft. (A) Preoperative anteroposterior view of X-ray. (B) Preoperative coronal view MRI. (C) Preoperative sagittal view MRI. (D) Postoperative anteroposterior view of X-ray. (E) Postoperative coronal view MRI. (F) Postoperative sagittal view MRI. Please click here to view a larger version of this figure.
| Outcome Metric | Modified LT Transfer Preoperative | Modified LT Transfer Postoperative | P Modified LT Transfer Postoperative | Traditional LD Transfer (Literature)34,35 |
| (3 Months) | (6 Months) | |||
| External Rotation (Degrees) | 15 ± 5 | 42 ± 10 | 51 ± 10 | 46 ± 10 |
| ASES Score | 29 ± 5 | 70 ± 5 | 77 ± 5 | 75 ± 5 |
| UCLA Score | 15 ± 3 | 28 ± 2 | 31 ± 2 | 30 ± 2 |
| VAS Pain Score | 8 ± 1 | 3 ± 1 | 2 ± 1 | 2 ± 1 |
Table 1. Pre- and postoperative outcomes. Abbreviations: LT = lower trapezius; LD = latissimus dorsi; ASES = American Shoulder and Elbow Surgeons; VAS = visual analog scale.
| Parameter | Modified LT Transfer | Traditional LD Transfer34,35 |
| External Rotation (Degrees Improved) | +36 (15 to 51) | +31 |
| ASES score (Postoperative) | +48(29 to 77) | +49 |
| UCLA Score (VAS Reduction) | +16 (15 to 31) | +15 |
| VAS Score Improvement | -6 (8 to 2) | -6 |
Table 2: Comparison of Outcomes (Modified LT Transfer vs. LD Transfer). Abbreviations: LT = lower trapezius; LD = latissimus dorsi; ASES = American Shoulder and Elbow Surgeons; VAS = visual analog scale.
Discussion
In this protocol, a few critical steps have been identified to optimize the effectiveness and safety of the lower LT tendon transfer. First, put the patient in the beach chair position with a head holder, fixing the head in slight neck flexion. Positioning the patient near the bed's edge allows optimal access to the medial border of the scapula, facilitating the necessary exposure for precise dissection and secure graft placement. A wide surgical field is draped to ensure complete visibility of the shoulder and scapular regions, minimizing unintended tissue damage and maintaining anatomical orientation throughout.
One key modification in this protocol involves placing the lateral row anchors slightly more anterior than in traditional infraspinatus placements38. Stone et al. achieved an additional 20° gain in external rotation, demonstrating a notable improvement in shoulder function26. During fixation, positioning the shoulder in 45° abduction and 45° external rotation also helps achieve optimal graft orientation and tension, which is essential for postoperative fixation strength14,39.
The Pulvertaft suture for weaving the LT tendon with the Achilles allograft enhances strength at the integration site, increasing the construct's durability. Additionally, releasing the trapezius muscle with an incision from the medial border halfway along the scapular spine requires precision to avoid neurovascular damage. Maintaining a distance of approximately 58 mm from the tendon insertion to the spinal accessory nerve minimizes the risk of nerve injury, which could otherwise impair shoulder function and recovery16.
Our method, though previously unpublished, is straightforward, feasible, and practical, making it an accessible option for improving surgical outcomes. However, we currently lack detailed biomechanical data to validate the procedure fully. This limitation is being addressed through ongoing research to understand better the structural mechanics involved. Together, these critical steps and modifications contribute to a robust protocol, each element essential in enhancing patient outcomes and minimizing procedural complications.
Disclosures
The authors have no financial or competing interests related to this work to disclose. The authors gratefully thank the Taiwan Minister of Science and Technology and Linkou Chang Gung Memorial Hospital for the financial support of this study (Grant: MOST 111-2628-B-182A-016, NSTC112-2628-B-182A-002, CMRPG5K0092, CMRPG3M2032, CMRPG5K021, SMRPG3N0011)
Acknowledgements
The authors gratefully thank the Taiwan Minister of Science and Technology and Linkou Chang Gung Memorial Hospital for the financial support of this study (Grant: MOST 111-2628-B-182A-016, NSTC112-2628-B-182A-002, CMRPG5K0092, CMRPG3M2032, CMRPG5K021, SMRPG3N0011)
Materials
| Name | Company | Catalog Number | Comments |
| Flexigraft; Achilles allograft | LifeNet Health, Virginia Beach, VA | Fresh-frozen grafts, Tendon Length 160-260 mm | |
| Footprint knotless PEEK suture anchors | Smith & Nephew, Andover, MA | 4.5 mm anchor for lateral row fixation | |
| TwinFix Ti suture anchors | Smith & Nephew, Andover, MA | 5.0 mm anchor for medial row fixation | |
| Ultrabraid sutures | Smith & Nephew, Andover, MA | braided sutures |
References
- Oh, J. H., Park, M. S., Rhee, S. M. Treatment strategy for irreparable rotator cuff tears. Clin Orthop Surg. 10 (2), 119-134 (2018).
- Cvetanovich, G. L., Waterman, B. R., Verma, N. N., Romeo, A. A. Management of the irreparable rotator cuff tear. J Am Acad Orthop Surg. 27 (24), 909-917 (2019).
- Neri, B. R., Chan, K. W., Kwon, Y. W. Management of massive and irreparable rotator cuff tears. J Shoulder Elbow Surg. 18 (5), 808-818 (2009).
- Bertelli, J. A. Lengthening of subscapularis and transfer of the lower trapezius in the correction of recurrent internal rotation contracture following obstetric brachial plexus palsy. J Bone Joint Surg Br. 91 (7), 943-948 (2009).
- Wagner, E. R., et al. Novel arthroscopic tendon transfers for posterosuperior rotator cuff tears: Latissimus dorsi and lower trapezius transfers. JBJS Essent Surg Tech. 8 (2), e12 (2018).
- Grimberg, J., Kany, J., Valenti, P., Amaravathi, R., Ramalingam, A. T. Arthroscopic-assisted latissimus dorsi tendon transfer for irreparable posterosuperior cuff tears. Arthroscopy. 31 (4), 599-607.e591 (2015).
- Boileau, P., et al. Isolated loss of active external rotation: A distinct entity and results of l'episcopo tendon transfer. J Shoulder Elbow Surg. 27 (3), 499-509 (2018).
- Ghoraishian, M., Stone, M. A., Elhassan, B., Abboud, J., Namdari, S. Techniques for lower trapezius tendon transfer for the management of irreparable posterosuperior rotator cuff tears. J Orthop. 22, 331-335 (2020).
- Omid, R., et al. Biomechanical comparison between the trapezius transfer and latissimus transfer for irreparable posterosuperior rotator cuff tears. J Shoulder Elbow Surg. 24 (10), 1635-1643 (2015).
- Reddy, A., et al. Biomechanics of lower trapezius and latissimus dorsi transfers in rotator cuff-deficient shoulders. J Shoulder Elbow Surg. 28 (7), 1257-1264 (2019).
- Clouette, J., et al. The lower trapezius transfer: A systematic review of biomechanical data, techniques, and clinical outcomes. J Shoulder Elbow Surg. 29 (7), 1505-1512 (2020).
- Muench, L. N., et al. Biomechanical comparison of lower trapezius and latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears using a dynamic shoulder model. J Shoulder Elbow Surg. 31 (11), 2392-2401 (2022).
- Elhassan, B. Lower trapezius transfer to improve external shoulder rotation in patients with brachial plexus injury. Techniques in Shoulder & Elbow Surgery. 10 (3), 119-123 (2009).
- Elhassan, B. T., Alentorn-Geli, E., Assenmacher, A. T., Wagner, E. R. Arthroscopic-assisted lower trapezius tendon transfer for massive irreparable posterior-superior rotator cuff tears: Surgical technique. Arthrosc Tech. 5 (5), e981-e988 (2016).
- Kierner, A. C., Zelenka, I., Heller, S., Burian, M. Surgical anatomy of the spinal accessory nerve and the trapezius branches of the cervical plexus. Arch Surg. 135 (12), 1428-1431 (2000).
- Omid, R., Cavallero, M. J., Granholm, D., Villacis, D. C., Yi, A. M. Surgical anatomy of the lower trapezius tendon transfer. J Shoulder Elbow Surg. 24 (9), 1353-1358 (2015).
- Almeida, T. B., Pascarelli, L., Bongiovanni, R. R., Tamaoki, M. J., Rodrigues, L. M. Outcomes of lower trapezius transfer with hamstring tendons for irreparable rotator cuff tears. Shoulder Elbow. 15 (4 Suppl), 63-71 (2023).
- Pérez-Prieto, D., et al. Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 24 (9), 2724-2728 (2016).
- Barret, H., et al. Vancomycin soaking to reduce intraoperative contamination by cutibacterium acnes during the latarjet procedure. Am J Sports Med. 52 (11), 2843-2849 (2024).
- Denard, P. J., Lädermann, A., Burkhart, S. S. Prevention and management of stiffness after arthroscopic rotator cuff repair: Systematic review and implications for rotator cuff healing. Arthroscopy. 27 (6), 842-848 (2011).
- Stoll, L. E., Codding, J. L. Lower trapezius tendon transfer for massive irreparable rotator cuff tears. Orthopedic Clinics. 50 (3), 375-382 (2019).
- Gupta, A., Ker, A. M., Maharaj, J. C., Veen, E. J. D., Cutbush, K. All-arthroscopic muscle slide and advancement technique to repair massive retracted posterosuperior rotator cuff tears. Arthrosc Tech. 10 (6), e1439-e1446 (2021).
- Noh, K. -. C., Lang, J., Oh, J. -. U., Kim, Y. -. T., Morya, V. K. Arthroscopic-guided release of supraspinatus and infraspinatus muscles for repair of large-to-massive rotator cuff tear and suprascapular nerve release. Arthrosc Tech. , (2024).
- Baek, C. H., Kim, B. T., Kim, J. G. Arthroscopic-assisted lower trapezius tendon transfer using a fasciae lata autograft in treatment of posterior superior irreparable rotator cuff tears in lateral decubitus position. Arthrosc Tech. 12 (12), e2227-e2237 (2023).
- Wagner, E. R., Elhassan, B. T. Surgical management of massive irreparable posterosuperior rotator cuff tears: Arthroscopic-assisted lower trapezius transfer. Curr Rev Musculoskelet Med. 13 (5), 592-604 (2020).
- Stone, M. A., Kane, L. T., Ho, J. C., Namdari, S. Short-term outcomes of lower trapezius tendon transfer with Achilles allograft for irreparable posterosuperior rotator cuff tears. Arthrosc Sports Med Rehabil. 3 (1), e23-e29 (2021).
- De Marinis, R., et al. Lower trapezius transfer improves clinical outcomes with a rate of complications and reoperations comparable to other surgical alternatives in patients with functionally irreparable rotator cuff tears: A systematic review. Arthroscopy. 40 (3), 950-959 (2024).
- Sanchez-Sotelo, J. Lower trapezius transfer for irreparable posterosuperior rotator cuff tears. Curr Rev Musculoskelet Med. 17 (4), 93-100 (2024).
- Baek, C. H., Lee, D. H., Kim, J. G. Latissimus dorsi transfer vs. Lower trapezius transfer for posterosuperior irreparable rotator cuff tears. J Shoulder Elbow Surg. 31 (9), 1810-1822 (2022).
- Clouette, J., et al. The lower trapezius transfer: A systematic review of biomechanical data, techniques, and clinical outcomes. J Shoulder Elbow Surg. 29 (7), 1505-1512 (2020).
- Elhassan, B. T., Wagner, E. R., Werthel, J. -. D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. 25 (8), 1346-1353 (2016).
- Valenti, P., Werthel, J. D. Lower trapezius transfer with semitendinosus tendon augmentation: Indication, technique, results. Obere Extrem. 13 (4), 261-268 (2018).
- Chopra, A., Wright, M. A., Murthi, A. M. Outcomes after arthroscopically assisted lower trapezius transfer with achilles tendon allograft. J Shoulder Elbow Surg. 33 (2), 321-327 (2024).
- De Mey, K., Cagnie, B., Danneels, L. A., Cools, A. M., Van De Velde, A. Trapezius muscle timing during selected shoulder rehabilitation exercises. J Orthop Sports Phys Ther. 39 (10), 743-752 (2009).
- Grimberg, J., Kany, J. Latissimus dorsi tendon transfer for irreparable postero-superior cuff tears: Current concepts, indications, and recent advances. Curr Rev Musculoskelet Med. 7 (1), 22-32 (2014).
- Wey, A., Dunn, J. C., Kusnezov, N., Waterman, B. R., Kilcoyne, K. G. Improved external rotation with concomitant reverse total shoulder arthroplasty and latissimus dorsi tendon transfer: A systematic review. J Orthop Surg (Hong Kong). 25 (2), 2309499017718398 (2017).
- Ek, E. T., Lording, T., Mcbride, A. P. Arthroscopic-assisted lower trapezius tendon transfer for massive irreparable posterosuperior rotator cuff tears using an Achilles tendon-bone allograft. Arthrosc Tech. 9 (11), e1759-e1766 (2020).
- Wagner, E. R., et al. Novel arthroscopic tendon transfers for posterosuperior rotator cuff tears: Latissimus dorsi and lower trapezius transfers. JBJS Essent Surg Tech. 8 (2), e12 (2018).
- Woodmass, J. M., et al. Arthroscopic lower trapezius tendon transfer provides equivalent outcomes to latissimus dorsi transfer in the treatment of massive posterosuperior rotator cuff tears. JISAKOS. 5 (5), 269-274 (2020).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved