Method Article
Gastroscope-assisted Trans-Trocar Gastrostomy and Abdominal Exploration
In This Article
Summary
Here, we introduce a novel technique of gastrostomy, which integrates laparoscopic and gastroscopic techniques, offering a streamlined approach with reduced invasiveness, expedited recovery, and the capacity for abdominal exploration while minimizing the risk of adjacent organ injury.
Abstract
Advanced endoscopic technologies have revolutionized gastrointestinal surgical procedures, transitioning from open or laparoscopic methods to endoscopic interventions. Gastrostomy is a classic clinical technique for patients with swallowing impediments due to obstructions in the cardiac or esophageal regions and has evolved significantly with the establishment of percutaneous endoscopic gastrostomy (PEG). While PEG offers reduced trauma and swift recovery, it falls short of exploratory capabilities and risks damaging adjacent organs. Therefore, we developed an innovative approach-gastroscope-assisted trans-Trocar gastrostomy (GTTG), which not only takes full play to the advantages of PEG with less trauma and faster postoperative recovery but also takes into account the advantages of laparoscopic gastrostomy with a good exploration of the abdominal cavity. This technique is characterized by ease of operation, minimal trauma (including short operation time and no redundant incision), rapid recovery, the ability to explore the abdominal cavity, and avoidance of injury to adjacent organs, which is quite worthy of widespread promotion in clinical settings.
Introduction
Gastrostomy is the cornerstone of enteral nutrition for patients with organic or functional obstruction of the cardiac orifice or other organs1. Percutaneous endoscopic gastrostomy (PEG) was first performed in 1979, and it is now a widely accepted and practiced approach2. A PEG tube not only functions as a conduit for the administration of liquid nutritional supplements directly into the stomach but also holds utility in the realms of gastric decompression and the management of gastric volvulus, which offers a multifaceted approach to gastrointestinal care3. PEG is a minimally invasive approach compared with traditional open gastrostomy. Currently, two typical access types for PEGs have emerged, Pull-PEG and Push-PEG. Pull-PEG is the standard procedure used to help patients whose gastroscopic access to the stomach is difficult due to obstruction or stenosis. In Push-PEG, primary gastropexy is performed under disphanoscopy followed by the direct introduction of a balloon-fixed tube4. Although PEG is considered a safe procedure, several complications can occur, including bumper syndrome, bleeding, and tube dislodgement. Several studies have focused on finding solutions to these complications, but only a few have succeeded5.
Another disadvantage of traditional PEG is that, compared to traditional open or laparoscopic gastrostomy, peritoneal exploration is unreliable during PEG. Moreover, bleeding could not be completely avoided because the vessels on the surface of the stomach were invisible when performing Pull-PEG or Push-PEG, and the greater omentum was sometimes attached or damaged6. To address these shortcomings, we propose a hybrid approach that combines endoscopic and laparoscopic techniques and offers a clinically viable and widely applicable method.
Protocol
Ethical approval for the surgical procedure was granted by the ethics board at the First Affiliated Hospital, Sun Yat-Sen University. A 65-year-old male patient, presenting with a one-month history of dysphagia and a diagnosis of esophageal carcinoma with extensive lymph node metastases, was deemed a candidate for systemic therapy following multidisciplinary team discussions. Given the tumor-induced obstruction, gastrostomy was planned to facilitate enteral nutrition, and the patient provided informed consent before the procedure.
1. Surgical procedures
- Place the patient in a supine position after general anesthesia post-tracheal intubation.
- Use a povidone-iodine solution for routine disinfection.
NOTE: The chief surgeon and an assistant are located on the left side of the patient. - Make a 1 cm incision at the predetermined site. The site is located 2 cm right to the left midclavicular line and 2-4 cm below the costal arch, which is the position for gastrostomy (Figure 1).
- Insert a 12 mm Trocar and inject CO2 gas to maintain an abdominal pressure of 12 mmHg.
- Introduce a gastroscope into the abdominal cavity through the Trocar and explore the abdominal cavity.
- Find the non-vascular zone of the anterior wall of the stomach for further gastrostomy.
- Utilize rat tooth forceps to clamp the selected site and exteriorize it using the gastroscope and the trocar.
- Fix the gastric well with a cured clamp to prevent retraction into the abdominal cavity.
- Anchor the gastric well to the abdominal wall with four interrupted sutures using 2-0 absorbable sutures.
- Execute a purse-string suture on the gastric wall with 2-0 absorbable sutures.
- Open the stomach well using an electrotome, and insert a balloon-type gastrostomy tube into the gastric cavity.
- Instill ~20 mL of normal saline (NS) into the balloon to secure the tube and tie up the tube again with the 2-0 absorbable sutures.
- Administer 20-50 mL of NS into the tube to test its patency.
- Fix the tube on the abdominal wall with 2-0 absorbable sutures.
- Close the incision around the tube with interrupted sutures using 2-0 absorbable sutures (Figure 2).
2. Postoperative procedures
- Send the patient back to the ward safely after resuscitation.
- Administer 500 mL of glucose saline through the gastrostomy tube one day after the operation to maintain tubal patency.
- Administer 250-500 mL of enteral nutrient solution through the gastrostomy tube 2 days after the operation.
- Increase the volume of enteral nutrient to 1,500-2,000 mL per day gradually.
Results
The operation was completed within 50 min, with minimal intraoperative bleeding of <5 mL. Enteral nutrition was initiated one day postoperatively, with a gradual increase in volume. By the 4th day, no additional parenteral nutrition was required. The patient and his family members were trained to perform enteral nutrition via a tube s for home care after discharge. Systemic antitumor therapy was commenced 3 days after the operation, and the patient was discharged 4 days later (Table 1). During the subsequent treatments, the patient returned to the hospital for tube maintenance and resolution of issues related to home care.

Figure 1: Trocar placement. The site of the trocar is chosen with the location being 2 cm right to the left midclavicular line and 2-4 cm below the costal arch, which is the position for the gastrostomy. Please click here to view a larger version of this figure.
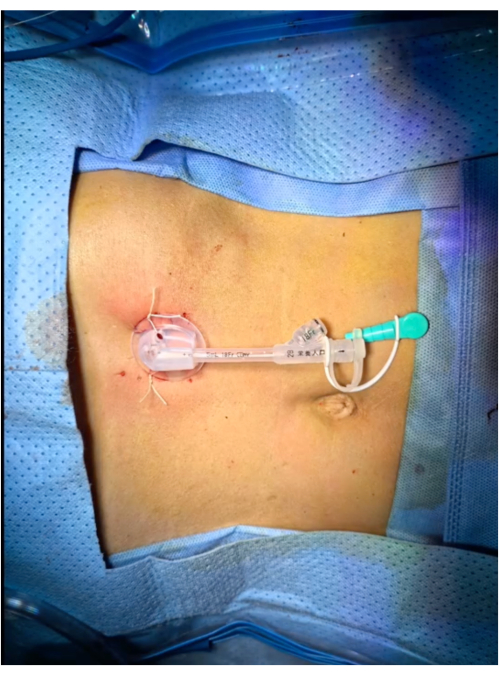
Figure 2: Postoperation abdominal well display. The gastrostomy tube is the only visible object on the abdominal wall, with no other wounds detected. Please click here to view a larger version of this figure.
| Operation time (min) | 50 |
| Intraoperative blood loss (mL) | Less than 5 mL |
| First postoperative tube usage (days) | 1 |
| First posteroperative total enternal nutrition (days) | 4 |
| Systemic anti-tumor therapy after operation (days) | 3 |
| Postoperative hospital stay (days) | 4 |
| Postoperative complications (yes/no) | No |
Table 1: Surgical outcomes.
Discussion
Gastrostomy is a classic therapy for patients without the ability to undergo it because of the organic or functional obstruction of the digestive tract above the cardia. With the development of medicine, laparotomy and laparoscopy have gradually been replaced by PEG, which was first performed in 19797. However, in cases of severe obstruction, endoscopy access may be impeded, prompting the development of Push-PEG and radiologic gastrostomy (RG) to address these challenges8,9. Recently, PEG or RG has been widely applied in most cases. However, the pursuit of minimally invasive procedures has sometimes overlooked the necessary explorations, potentially leading to further downstream obstruction and enteral feeding failure. Traditional surgical approaches offer partial solutions but are limited by the constraints of small incisions. To overcome the exploratory limitations of PEG, we combined the laparoscopic and endoscopic techniques. The gastroscope, inserted into the Trocar, facilitates abdominal cavity investigation, with the Trocar incision serving as the gastrostomy site, and maximizing the utility of a single incision.
In some cases, PEG or RG may accidentally damage adjacent organs such as the liver, greater omentum, and colon, because of the operating field of view of the stomach cavity. The altered anatomical structure is a potential reason and it is believed that laxity of the colonic mesentery in elderly patients makes iatrogenic perforation of the bowels more commonly10. Moreover, bleeding due to injury around the arteries and veins is a common complication during or after PEG and RG11. Our gastroscope-assisted trans-Trocar gastrostomy can directly identify the avascular area of the stomach and capture the stomach wall insertion site under direct vision, thereby mitigating the complications mentioned above.
However, certain PEG complications, such as peristomal infection and tube fractures, persist. Lotti et al. reported a novel technique, laparoscopic tabularized continent gastrostomy to avoid applying the foreign body12. However, the complexity and extended operative and recovery times have hindered their widespread clinical adoption. Nevertheless, this concept is both intriguing and encouraging. To reduce the risk of peristomal infection, tightly closing the incision is critical. The lower the exposure of gastric juices eroding the surrounding skin, the lower the risk of peristomal infection.
In conclusion, we report a novel approach to gastrostomy, gastroscope-assisted trans-Trocar gastrostomy, which combines laparoscopic and endoscopic techniques. GTTG has the advantages of easy operation, minimal trauma (including short operation time and no redundant incision), rapid recovery, exploration capabilities, and avoidance of injury to adjacent organs, which warrants its broader clinical implementation, especially in patients who lack pathological results or have anatomic variation.
Disclosures
The authors have no conflicts of interest to disclose.
Acknowledgements
This work was supported by grants from Guangdong Basic and Applied Basic Research Foundation (2021A1515110759) and the Natural Science Foundation of Guangdong Province of China (2023A1515011197).
Materials
| Name | Company | Catalog Number | Comments |
| 2-0 absorbable suture | Ethicon | VCP345H | |
| Curved forceps | |||
| Electric knife pen | Xinhai Hexing Science and technology (dalian) co.,LTD | ||
| Gastroscope | Olympics | GIF-H290Z | |
| Percutaneous gastroscopy kit | CREATE MEDIC | PEG18 | |
| Rat tooth forceps | Micro-Tech(Nanjing) | MTN-GF-23 | |
| Scissors | |||
| Trocar | Surgaid Medical | 12mm | |
| Vessel forceps |
References
- Garne, E., et al. Gastrostomy and congenital anomalies: A European population-based study. BMJ Paediatr Open. 6 (1), e001526 (2022).
- Ponsky, J. L. Percutaneous endoscopic gastrostomy: After 40 years. Gastrointest Endosc. 93 (5), 1086-1087 (2021).
- Lord, L. M. Enteral access devices: Types, function, care, and challenges. Nutr Clin Pract. 33 (1), 16-38 (2018).
- Kucha, P., et al. To push or to pull? A clinical audit on the efficacy and safety of the pull and push percutaneous endoscopic gastrostomy techniques in oncological patients. United European Gastroenterol J. 11 (10), 951-959 (2023).
- Boeykens, K., Duysburgh, I. Prevention and management of major complications in percutaneous endoscopic gastrostomy. BMJ Open Gastroenterol. 8 (1), e000628 (2021).
- Boeykens, K., Duysburgh, I., Verlinden, W. Prevention and management of minor complications in percutaneous endoscopic gastrostomy. BMJ Open Gastroenterol. 9 (1), e000975 (2022).
- Gauderer, M. W., Ponsky, J. L., Izant, R. J. Gastrostomy without laparotomy: A percutaneous endoscopic technique. J Pediatr Surg. 15 (6), 872-875 (1980).
- Laasch, H. U., Martin, D. F. Radiologic gastrostomy. Endoscopy. 39 (3), 247-255 (2007).
- Kim, R., et al. Percutaneous radiologic gastrostomy with single gastropexy: Outcomes in 636 patients. Eur Radiol. 31 (9), 6531-6538 (2021).
- Ahmad, J., Thomson, S., Mcfall, B., Scoffield, J., Taylor, M. Colonic injury following percutaneous endoscopic-guided gastrostomy insertion. BMJ Case Rep. 2010, 1-5 (2010).
- Rahnemai-Azar, A. A., Rahnemaiazar, A. A., Naghshizadian, R., Kurtz, A., Farkas, D. T. Percutaneous endoscopic gastrostomy: Indications, technique, complications and management. World J Gastroenterol. 20 (24), 7739-7751 (2014).
- Lotti, M., Carrara, G., Lovece, A., Giulii Capponi, M. Laparoscopic tubularized continent gastrostomy: An alternative to tube gastrostomies. Updates Surg. 72 (3), 901-905 (2020).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved