Method Article
Modified Laparoscopic Inguinal Lymphadenectomy Using an Abdominal Subcutaneous Approach
* These authors contributed equally
In This Article
Summary
The efficacy of laparoscopic inguinal lymph node dissection is comparable to that of open surgery. It also significantly decreases the incidence of complications. In this study, a modified laparoscopic method was used for inguinal lymph node dissection through the abdominal subcutaneous approach for penile cancer treatment.
Abstract
Inguinal lymph node metastases significantly impact the prognosis of patients with penile cancer. Therefore, timely inguinal lymph node dissection is essential for the comprehensive treatment of penile cancer. Compared with the traditional open inguinal lymphadenectomy, laparoscopic inguinal lymphadenectomy offers similar tumor control with fewer complications. The current techniques for the laparoscopic surgical approach include L-lymphoid clearance sequence and preservation of the great saphenous vein. In this study, a transabdominal subcutaneous anterograde approach was employed to improve laparoscopic inguinal lymph node dissection and conserve the great saphenous vein, resulting in favorable outcomes. Furthermore, only 2 out of 21 patients experienced wound infections, and only 1 exhibited lymphatic leakage from the drainage orifice. These findings indicate that the use of an innovative subcutaneous transperitoneal retrograde approach is safe for abdominal endoscopic common iliac plexus dissection with fewer complications in patients with penile cancer compared with traditional open surgery. Notably, the postoperative survival rate of penile cancer patients is significantly influenced by the presence or absence of inguinal lymph node metastasis and the extent of metastasis. Timely inguinal lymph node dissection is essential since it significantly impacts the treatment of penile cancer. Besides, laparoscopic inguinal lymphadenectomy offers comparable tumor control to open surgery with significantly reduced complications. Notably, standardized approaches for laparoscopic surgery, cleaning procedures, and preservation of the saphenous vein are crucial for inguinal lymph node dissection. The laparoscopic inguinal lymphadenectomy technique can be improved by employing the abdominal subcutaneous anterograde approach. This article provides a comprehensive account of the procedures and technical improvements associated with the modified laparoscopic inguinal lymphadenectomy using the abdominal subcutaneous approach.
Introduction
Penile cancer is a relatively uncommon malignant tumor of the genitourinary system, with squamous cell carcinoma representing about 95% of cases. Penile cancer is mainly spread through the lymphatic system, with the initial site of dissemination being the inguinal lymph nodes1. The superficial and deep inguinal lymph nodes are the main regional sites for the spread of penile cancer, followed by the pelvic lymph nodes, which include the external and internal iliac lymph nodes, with rare metastasis. Besides the grade and stage of the primary tumor, the presence and scope of inguinal lymph node metastasis affect the prognosis of penile cancer2. Therefore, timely radical lymph node dissection is essential for enhancing survival rates.
Timely inguinal lymph node dissection can improve the 5-year survival rate of patients with penile cancer from 30%-40% to 80%-90% after metastasis. The current treatment guidelines for penile cancer recommend inguinal lymphadenectomy, removal of palpable inguinal lymph nodes, or removal of unreachable inguinal lymph nodes. Although open inguinal lymph node dissection is effective, it is significantly associated with a high rate of postoperative incision infection, delayed healing, skin necrosis, lymphedema, lower limb edema, and other complications3,4. Besides, it is unclear whether timely prophylactic inguinal lymph node dissection is beneficial due to many complications caused by inguinal lymph node dissection5.
A previous study has reported that prophylactic inguinal lymph node dissection should be considered for patients with impalpable lymph nodes since 25% of them may harbor micrometastatic disease. Invasive nodal staging is required for patients with clinically node-negative disease (cN0). Invasive lymph node staging can be performed through dynamic sentinel lymph node biopsy or modified inguinal lymphadenectomy for intermediate-risk pT1 and T2-T4 tumors tumors6.
Laparoscopic minimally invasive techniques have been widely used in recent years for inguinal lymph node dissection, resulting in comparable tumor control to open surgery7 and a significant reduction in complications8,9,10. Notably, standardized approaches for laparoscopic surgery, cleaning procedures, and preservation of the great saphenous vein are crucial for inguinal lymph node dissection11,12,13.
The transabdominal subcutaneous anterograde approach can improve laparoscopic inguinal lymph node dissection and preserve the saphenous vein. This manuscript provides a detailed explanation of the procedure and technical advancements associated with the modified laparoscopic transabdominal subcutaneous approach for anterograde inguinal lymph node dissection. The aim is to present an improved surgical approach for reducing the incidence of postoperative complications such as skin necrosis, delayed wound healing, lymphedema, and lower limb edema.
Protocol
This study was approved by the Institutional Review Board of Hainan Provincial People's Hospital, and all participants provided written informed consent.
1. Patient evaluation
- Enroll patients for the study who have received inguinal lymph node dissection for penile cancer between 1994 and 2022 using the following criteria. A total of 21 patients were included, and their clinicopathological and demographic details are shown in Table 1. Ensure the surgeries are conducted by the same surgical team through laparoscopy.
- Use the following inclusion criteria:(1) Confirmed pathological diagnosis of penile cancer; (2) Presence of high-risk local lesion with palpable active lymph nodes in the groin area or no palpable lymph nodes in the groin area but positive dynamic sentinel lymph node biopsy; (3) Medium or low-risk local lesion with palpable active lymph nodes in the groin area. Lymph node metastasis is confirmed by inguinal lymph node excision or fine needle aspiration biopsy.
- Use the following exclusion criteria: (1) Comorbidity of cardiovascular or coagulation disorders with contraindications for surgery; (2) Ulcer infection in the inguinal lymph nodes; (3) Preoperative local radiotherapy in the groin area; (4) Distant metastasis; (5) Preoperative ultrasound evaluation of lower limb blood vessels revealing deep vein diseases such as thrombosis or venous valve insufficiency; (6) Fixed inguinal lymph nodes.
- Perform a biopsy or resection before surgery to confirm the presence of penile cancer for all enrolled patients. Use the 2023 update of the EAU (European Association of Urology)-American Society of Clinical Oncology Collaborative Guideline on Penile Cancer classification to classify the patient6.
- In the present study, 1 out of the 21 patients was classified as stage I, 4 cases as stage IIA, 2 cases as stage IIB, 4 cases as stage IIIB, 2 cases as stage IIIA, and 8 cases as stage IV. Among them, 1 patient had diabetes, and 1 patient had hypertension and a previous cerebral infarction.
- Perform physical and urinary system examinations, electrocardiogram (EKG), chest radiograph, and laboratory testing. Consider unresectable diseases, which include metastases beyond pelvic lymph nodes, and patients with severe systemic diseases such as coagulation dysfunction and severe heart disease who cannot tolerate surgery, as contraindications.
2. Positioning, trocar port placement, and marking of anatomical boundaries
- Positioning
- Prior to surgery, place a double-lumen catheter into the urethra. Administer general anesthesia and position the patient in a supine posture with the head lowered and the hips elevated at an angle of 10°-20°. Flex the knee onto their sides and abduct the hips.
- Placement of the trocar port
- After the disinfection of the surgical site and the placement of a sterile towel, make a longitudinal incision 1 cm below the umbilicus using a scalpel to cut through the skin and subcutaneous tissues, including the Camper's fascia, Scarpa's fascia, confirming the anterior rectus sheath.
- Create a long tunnel along the aponeurosis surface of the external oblique towards the inguinal ligament using the index finger. Utilize a custom-designed balloon for the purpose of dilating and creating subcutaneous space. Retain a 12 mm metal port at this incision to serve as a lens hole.
- Proceed to dissect the right inguinal lymph nodes with an ultrasonic scalpel and insufflate the subcutaneous pneumoperitoneum space with CO2 at 12-15 mmHg to distend the space rapidly. Place a 5 mm port at the midpoint of the umbilicus pubic line and a 10 mm port at the midpoint between the umbilicus and the anterior superior right iliac spine.
- Place a 5 mm port at the midpoint of the left anterior superior iliac spine of the umbilicus. Establish and maintain four puncture holes on both sides. Repeat steps 2.2.3 and clear the lymph nodes in the left inguinal region (Figure 1A,B).
- Delineate the anatomical boundaries for inguinal lymph node dissection, adhere to the following guidelines: position the upper boundary 1 cm above the inguinal ligament, align the inner boundary with the lateral margin of the adductor longus muscle, corresponding to the outer boundary to the medial margin of the sartorius muscle, and locate the inferior boundary at the apex of the femoral triangle. Mark the area for bilateral inguinal clearance (Figure 1C).
3. Surgical procedures
- Identify the inguinal ligament: Locate and dissect the inguinal ligament downward, separating it between the aponeurotic surface of the external oblique and Scarpa's fascia. Locate the position of the inguinal ligament by applying pressure with the help of an assistant, fully dissociate, and expose the inguinal ligament (Figure 2A).
- Search for the root of the saphenous vein: With the help of the assistant, pull the spermatic cord, follow the path along the surface of the inguinal ligament, and subsequently release it downward to locate, confirm, and free the root of the great saphenous vein, where it joins the femoral vein (Figure 2B).
- Establish and expand medial and lateral fossa: Establish and expand the range on the inner and outer sides along the root of the great saphenous vein by adhering closely to the fascia lata of the thigh. The assistant should press on the original markings and ensure that the clearing range on the inner and outer sides is sufficiently large (Figure 2 C,D).
- Dissect the deep lymph nodes: Proceed along the root of the saphenous vein to confirm the location of the femoral vessel. Cut the anterior sheath of the femoral blood vessel, free the root of the great saphenous vein, the femoral vein, the femoral duct, and the surface of the femoral artery. Clean the medial side of the femoral vein and the lymph nodes inside the femoral canal (Cloquet lymph nodes) and collect the cleared deep group lymph nodes for rapid pathological examination. If positive, clear the pelvic lymph nodes (Figure 2 E,F).
- Dissect superficial lymph nodes and preserve the main trunk of the great saphenous vein:
Liberate the great saphenous vein from its root and completely release its entire length, including its five tributaries.- Starting from the root of the great saphenous vein, move downwards and free up the entire great saphenous vein and its five tributaries. First, free up and cut off the superficial iliac circumflex vein and internal pudendal vein. Clean the superficial lymph nodes in the Camper fascial gap of the skin, identify, free up, and ligate the superficial epigastric vein, the saphenous vein on the medial side of the thigh, and saphenous vein on the lateral side of the thigh while preserving the main trunk of the great saphenous vein.
- Identify, free, and ligate the superficial veins of the abdominal wall, medial thigh, and lateral thigh while preserving the main trunk of the great saphenous vein.
- In case of large lymphatic vessels, postpone cauterization to minimize postoperative lymphatic leakage. Divide the cleansed superficial group of lymph nodes into two sections, using the great saphenous vein as a boundary, and extract each section into separate specimen bags (Figure 2G-I).
- Postoperative treatment: Treat the wound to achieve complete hemostasis and place a negative pressure drainage ball at the lowest point of the incision to facilitate fluid suction through negative pressure. Apply appropriate pressure and dressings to the inguinal area. Administer medication to prevent infection and ease pain during the patient's hospital stay.
Results
The mean age of the included patients was 55 years (range: 31-79 years). The urinary catheter was removed between the 7th and 8th day after surgery. The average length of hospital stay after surgery was 14 days. Post-operation, 3 patients experienced necrosis of external genitalia wounds, and 4 patients had lymphatic leakage. Lymphatic leakage was successfully resolved through continued drainage, resulting in a prolonged average stay. All participants underwent laparoscopic groin lymph node dissection. The specific surgical details and results are presented in Table 2. The average duration of unilateral laparoscopic and bilateral surgeries was 146 min (90-180 min) and 182 min (115-220 min), respectively. Unilateral and bilateral surgeries resulted in an average blood loss of 10 mL (5.0-20 mL) and 22 mL (5.0-100 mL), respectively.
In this statistical analysis, due to the limited number of cases, some patients with combined lymphatic leaks and incision infections were also included in the study cohort, leading to an imbalance in the average hospital stay. For instance, in Table 2, among patients who underwent bilateral lymph node dissection, the shortest hospital stay was 6 days, while the hospital stays for patients with postoperative lymphatic leaks and incision infections were 18 days, 17 days, and 22 days, respectively. This extended the average hospital stay and led to an imbalance in the data.
An average of 12 (2-39) nodes were removed during lymph node dissection (Figure 3C). Histological analysis verified the presence of positive inguinal lymph nodes in 7 patients. Of 21 cases, 14 were classified as well-differentiated squamous cell carcinomas (Figure 3A,B), 3 as moderately differentiated (Figure 3D), 1 as verrucous carcinoma, and 1 as keratinizing squamous cell carcinoma.

Figure 1: Trocar placement and marking of anatomical limits. (A) Intraoperative trocar placement. (B) Postoperative trocar placement. (C) Marking of anatomical limits. Upper bound to 1 cm above the inguinal ligament, inner bound to the lateral margin of adductor longus muscle, outer bound to the medial margin of sartorius, and inferior bound to the apex of the femoral triangle. Please click here to view a larger version of this figure.
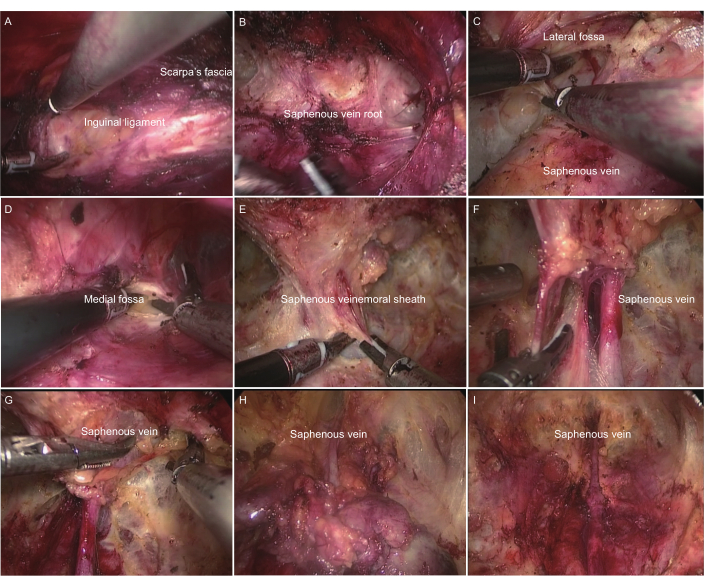
Figure 2: Procedure of modified transabdominal inguinal lymph node dissection. (A) Identifying the inguinal ligament. (B) Identifying the saphenous vein root. (C) Establishing and expanding lateral fossa. (D) Establishing and expanding medial fossa. (E) Cutting the femoral sheath. (F) Dissecting deep lymph nodes: saphenous vein and femoral artery vein. (G) Dissecting superficial lymph nodes: the root of the saphenous vein. (H) Dissecting superficial lymph nodes: the distal end of the saphenous vein. (I) General appearance after inguinal lymph node dissection. Please click here to view a larger version of this figure.
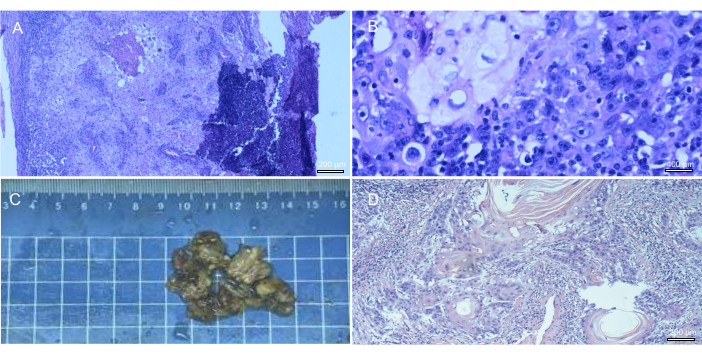
Figure 3: Inguinal lymph nodes excised during surgery, with subsequent pathological classification. (A-B) Metastatic well-differentiated squamous cell carcinoma in the right inguinal lymph node. (C) Left inguinal lymph node excised during surgery. (D) Metastatic moderately to well-differentiated squamous cell carcinoma in the left inguinal lymph node. Please click here to view a larger version of this figure.
| Variable | Value |
| Age, median (range), yr | 55 (31,79) |
| EAU stage | |
| I | 1(4.76%) |
| IIA | 4(19.05%) |
| IIB | 2(9.52%) |
| IIIA | 3(14.29%) |
| IIIB | 6(28.57%) |
| IV | 12(57.14%) |
| Squamous cell carcinoma | |
| Well-differentiated | 12 (57.14%) |
| Moderately differentiated | 7 (33.3%) |
| Keratinizing | 1(4.76%) |
| Complicated with diabetes | 1(4.76%) |
| Complicated with hypertension | 2(0.08%) |
Table 1: Demographic and clinicopathologic data of 21 patients.
| Variable | Value |
| Operative time, median (range), min | |
| Unilateral | 146(90-180) |
| Bilateral | 182(115-220) |
| Operative blood loss, median (range), mL | |
| Unilateral | 10(5-20) |
| Bilateral | 22(5-100) |
| Node count, median (range) | |
| Inguinal | 12(2,39) |
| Pelvic | 0.00 |
| Patients with positive node | 7(33.3%) |
| Duration of drain, median (range) day | |
| Unilateral | 28(7.0,50) |
| Bilateral | 33(7.0,60) |
| Length of stay, median (range), day | |
| Unilateral | 19(8.0,30) |
| Bilateral | 29(13,45) |
| Complications | 3(14.29%) |
| Wound infection | 2(9.52%) |
| Lymphorrhea | 1(476%) |
Table 2: Operative and pathologic data of 21 patients.
Discussion
The continuous development and improvement of lymph node dissection has improved penile cancer treatment. In this study, the surgical approach was modified to achieve the sequence of superficial and deep lymph node dissection and the preservation of the great saphenous vein, which yielded positive results.
Selection of surgical approach
The best choice between the subcutaneous approach through the lower limb femoral triangle and the subcutaneous abdominal approach for laparoscopic inguinal lymphadenectomy is controversial. Although the subcutaneous approach is technically simpler, it is associated with greater trauma and is less convenient for deep lymph node dissection. The abdominal subcutaneous approach has been widely accepted in recent years due to advancements in surgical techniques. Clinical studies have indicated that this method is associated with reduced incisions and decreased risk of postoperative complications, such as lower limb lymphedema. Additionally, the subcutaneous approach allows for a more comprehensive dissection of pelvic lymph nodes11.
Researchers performed an anterograde dissection of inguinal lymph nodes using the abdominal subcutaneous approach in 2011. The puncture points were identified as the lower margin of the navel, the midpoint between the umbilicus and pubic symphysis, and the medial side of the anterior superior iliac spine14. Yuan et al.11 also assessed the therapeutic efficacy and postoperative complications of laparoscopic inguinal lymph node dissection.
Improvement of lymph node dissection sequence in shallow and deep groups and preservation technique of saphenous vein trunk
For the identification of anatomical landmarks, the surgeon must be well-acquainted with the anterior rectus sheath, external oblique aponeurosis, fascia lata, inguinal ligament, and the origin of the great saphenous vein. These landmarks provide clear anatomical guidance during the procedure and also significantly enhance the efficiency and safety of the operation. Particularly, the identification of the great saphenous vein is crucial for the dissection of both deep and superficial lymph nodes. Lymph node dissection can minimize the potential for venous reflux disorders and decrease the occurrence of postoperative lower limb edema. Catalona et al. showed that the saphenous vein preservation technique in inguinal lymphadenectomy minimizes complications and reduces lymphedema incidence15. Moreover, several studies have demonstrated that preservation of the saphenous vein during inguinal lymph node dissection can effectively decrease the occurrence of postoperative lower limb edema13,16.
The dissection should first address deep lymph nodes, followed by the superficial ones. This strategy improves the flow of the surgery, reduces the risk of injury to the great saphenous vein, and facilitates quicker decision-making for intraoperative frozen pathology analysis. Besides, preservation of the great saphenous vein and its branches decreases the incidence of postoperative lower limb edema and enhances the quality of postoperative recovery.
Conclusion
The results indicated that the modified laparoscopic techniques can safely and effectively achieve penile and inguinal lymph node dissection with acceptable complication rates and a high success rate. This method is simple and suitable for teaching and learning purposes. However, this was a single-center study with a limited number of clinical cases, which may lead to unbalanced results. Therefore, a long-term multi-center study with large samples and long follow-up time is needed to verify these findings.
Disclosures
The authors have no conflicts of interest.
Acknowledgements
None
Materials
| Name | Company | Catalog Number | Comments |
| Laparoscopic system | STORZ | 20172226846 | The system provides high-definition images. |
| Laproscopic trocar | Anhui Aofo Medical Equipment Tech Corporation | 20202020172 | Disposable laproscopic trocar. |
| Negative pressure drainage device | Futababra | 20150003 | This disposable material is suitable for negative pressure suction of patients. |
| Ultrasonic scalpel | Ethicon Endo-Surgery, LLC | V94A5C | It is used in endoscopic surgery to control bleeding and minimize thermal damage during soft tissue incision. |
References
- Sharma, P., Zargar, H., Spiess, P. E. Surgical advances in inguinal lymph node dissection: optimizing treatment outcomes. Urol Clin North Am. 43 (4), 457-468 (2016).
- Leijte, J. A., Kirrander, P., Antonini, N., Windahl, T., Horenblas, S. Recurrence patterns of squamous cell carcinoma of the penis: recommendations for follow-up based on a two-centre analysis of 700 patients. Eur Urol. 54 (1), 161-168 (2008).
- Singh, A., et al. Comparing outcomes of robotic and open inguinal lymph node dissection in patients with carcinoma of the penis. J Urol. 199 (6), 1518-1525 (2018).
- Leone, A., Diorio, G. J., Pettaway, C., Master, V., Spiess, P. E. Contemporary management of patients with penile cancer and lymph node metastasis. Nat Rev Urol. 14 (6), 335-347 (2017).
- Niyogi, D., Noronha, J., Pal, M., Bakshi, G., Prakash, G. Management of clinically node-negative groin in patients with penile cancer. Indian J Urol. 36 (1), 8-15 (2020).
- Brouwer, O. R., et al. European Association of urology-American society of clinical oncology collaborative guideline on penile cancer:2023 Update. Eur Urol. 83 (6), 548-560 (2023).
- Tobias-Machado, M., et al. Can video endoscopic inguinal lymphadenectomy achieve a lower morbidity than open lymph node dissection in penile cancer patients. J Endourol. 22 (8), 1687-1691 (2008).
- Nabavizadeh, R., Master, V. Minimally invasive approaches to the inguinal nodes in cN0 patients. Curr Opin Urol. 29 (2), 165-172 (2019).
- Tobias-Machado, M., et al. Video endoscopic inguinal lymphadenectomy (VEIL): minimally invasive resection of inguinal lymph nodes. Int Braz J Urol. 32 (3), 316-321 (2006).
- Tobias-Machado, M., et al. Video endoscopic inguinal lymphadenectomy: a new minimally invasive procedure for radical management of inguinal nodes in patients with penile squamous cell carcinoma. J Urol. 177 (3), 953-957 (2007).
- Yuan, P., et al. Comparative study of video endoscopic inguinal lymphadenectomy through a hypogastric vs leg subcutaneous approach for penile cancer. J Endourol. 32 (1), 66-72 (2018).
- Chiapparrone, G., et al. Saphenous-sparing laparoscopic inguinal lymphadenectomy. Int Braz J Urol. 44 (3), 645-646 (2018).
- Yuan, J. B., et al. Preservation of the saphenous vein during laparoendoscopic single-site inguinal lymphadenectomy: comparison with the conventional laparoscopic technique. BJU Int. 115 (4), 613-618 (2015).
- Xu, H., et al. Endoscopic inguinal lymphadenectomy with a novel abdominal approach to vulvar cancer: description of technique and surgical outcome. J Minim Invasive Gynecol. 18 (5), 644-650 (2011).
- Catalona, W. J. Modified inguinal lymphadenectomy for carcinoma of the penis with preservation of saphenous veins: technique and preliminary results. J Urol. 140 (2), 306-310 (1988).
- Yao, K., et al. Modified technique of radical inguinal lymphadenectomy for penile carcinoma: morbidity and outcome. J Urol. 184 (2), 546-552 (2010).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved