Method Article
Application of Laparoscopic Ultrasonography in Primary Choledochal Suture during Combined Two-lens Surgery
In This Article
Summary
Here, we develop and present a T-tube and intrabiliary stent-free technique utilizing dual-lens visualization (via laparoscope and choledochoscope) combined with laparoscopic ultrasonography (LUS) to perform primary choledochal suture.
Abstract
Gallstones combined with common bile duct stones are a common clinical disease. The minimally invasive treatments include laparoscopic cholecystectomy + laparoscopic common bile duct exploration (LC+LCBDE) and endoscopic retrograde cholangiopancreatography + laparoscopic cholecystectomy (ERCP+LC). LCBDE can resolve two issues in a single procedure, whereas ERCP+LC requires a two-step approach. As more studies have shown, common bile duct exploration with stone extraction followed by primary closure may lead to faster recovery and improved quality of life for patients.
Anatomical variations in bile ducts and vessels are well-known to be common. Laparoscopic ultrasound (LUS) is instrumental in clarifying the hepatic portal area's anatomical structures, determining biliary duct orientation, identifying spatial relationships between biliary ducts, hepatic arteries, and portal veins, and minimizing the risk of biliary injury.
The procedure is illustrated here through a detailed case description. After administering general anesthesia, a laparoscopic approach was routinely established to inspect the abdominal cavity and assess lesions. Laparoscopic ultrasound was employed to evaluate the gallbladder triangle within the hepatic portal region, including the anatomy of bile ducts and vessels. The gallbladder triangle was dissected, followed by a 5-0 needle incision of the bile duct wall. Choledochoscopy was performed for stone extraction, with confirmation of normal duodenal papillary function. Continuous suturing of the bile duct wall was achieved using 5-0 polydioxanone monofilament suture material. Concurrently, laparoscopic ultrasound verified complete stone clearance and assessed suture integrity.
Introduction
Cholecystolithiasis is a common clinical disease, with approximately 10-20% of patients developing secondary choledocholithiasis1,2. Gallstones combined with common bile duct stones are a frequent clinical condition. Bile duct obstruction may lead to abdominal pain, jaundice, biliary tract infections, and even severe shock. The optimal treatment involves relieving the obstruction and removing the lesions.
The current therapeutic approaches for gallbladder stones with common bile duct stones include open cholecystectomy + open common bile duct exploration (OC+OCBDE), endoscopic retrograde cholangiopancreatography + laparoscopic cholecystectomy (ERCP+LC), laparoscopic cholecystectomy + laparoscopic common bile duct exploration (LC+LCBDE)3,4.
Open surgery is associated with significant trauma and prolonged recovery, typically reserved for cases where minimally invasive techniques are not feasible. ERCP+LC and LC+LCBDE are considered minimally invasive alternatives. However, ERCP+LC requires two separate procedures and carries risks of complications such as bleeding, pancreatitis, duodenal perforation, and impaired Oddi sphincter function. In contrast, LC+LCBDE has been demonstrated as a safe and effective surgical method due to its minimal invasiveness, rapid recovery, shorter hospital stay, and favorable cost-effectiveness5,6,7. Additionally, LCBDE is indicated for patients with ERCP failure, acute cholangitis, acute pancreatitis, or a history of gastrointestinal diversion surgery7.
LCBDE encompasses two primary techniques: primary closure and T-tube drainage. Emerging evidence suggests that primary closure offers advantages over T-tube drainage, including shorter operative and hospitalization durations, as well as reduced postoperative and biliary complications8.
Primary closure of LCBDE can be performed with or without internal stenting. Studies indicate that stent-free primary closure is safe reliable, and avoids potential complications such as stent migration or the need for subsequent stent removal procedures9.
The biliary system exhibits significant anatomical variations10,11, with a reported variation rate of 42.3%12. During laparoscopic surgery, the inability to palpate anatomical structures, combined with tissue edema or visually ambiguous landmarks, increases the risk of bile duct and vascular injuries. Laparoscopic ultrasonography (LUS) addresses these challenges by enabling real-time evaluation of the hepatic portal area, providing dynamic visualization of bile ducts, vasculature, and surrounding tissues, compensating for the lack of tactile feedback, and enhancing surgical safety13,14. While transabdominal ultrasound remains a standard imaging modality for gallstone diagnosis, its accuracy is limited by factors such as abdominal wall thickness, visceral fat, and gastrointestinal gas interference. LUS overcomes these limitations by combining the benefits of conventional ultrasound with high-frequency, high-resolution imaging, direct organ proximity, and real-time intraoperative guidance.
Protocol
This protocol follows the ethical guidelines for human research at Dongguan Tungwah Hospital. The patient has signed the relevant informed consent form.
NOTE: A 78-year-old male patient was admitted with a 3-day history of abdominal pain. CT examination revealed cholecystolithiasis combined with choledocholithiasis, with a common bile duct (CBD) diameter of approximately 10 mm (see Figure 1). The preoperative evaluation showed no surgical contraindications. The instruments and equipment used are detailed in the Table of Materials.
1. Preoperative examination
- Blood tests: Perform liver function tests and kidney function tests, as well as complete blood count, coagulation profile, blood type, and crossmatch.
- Diagnostic imaging and evaluations: Perform electrocardiogram, chest X-ray, cardiovascular assessment, color Doppler ultrasound of the liver and biliary system, and computed tomography (CT) scan of the upper abdomen.
2. Operative procedure
- Perform endotracheal intubation and position the patient supine. Execute routine disinfection using a povidone-iodine solution.
NOTE: General anesthesia was administered according to institutionally approved protocols. - Perform a standard four-port technique of laparoscopic cholecystectomy (see Figure 2).
- Create a 10-mm vertical incision subumbilically, and introduce CO₂ gas using a Veress needle to establish pneumoperitoneum at 12 mmHg.
- Then, place the 10-mm trocar and laparoscope infraumbilically. Under the direct visualization provided by the laparoscope, place a subxiphoid port (10 mm), right midclavicular port (5 mm), and right anterior axillary port (5 mm).
- Surgical steps (see Figure 3 and Figure 4)
NOTE: The surgical procedure is performed by a surgeon with the assistance of an assistant.- Perform laparoscopic exploration of the abdominal cavity by following this sequence: top to bottom, solid organs first, then hollow organs, abdominal cavity first, then pelvic cavity, to systematically assess abdominal lesions (see Figure 3A).
- Use LUS to probe the hepatic portal area, place the laparoscopic probe at the porta hepatis region through the subxiphoid port (10 mm), and move the probe up and down. Distinguish bile ducts and blood vessels via blood flow signals and assess stone distribution (see Figure 3B and Figure 4A,B).
- Elevate the gallbladder fundus with atraumatic forceps (Assistant). Retract and expand Calot's triangle to optimize exposure (Surgeon). Dissect Calot's triangle layer by layer using an electrohook or ultrasonic scalpel (see Figure 3C).
- Use LUS to confirm the CBD location. Straighten a 5-0 round-bodied needle with a needle holder and tie a No.4 silk suture to its tail to prevent accidental loss.
- Grasp the needle midpoint with laparoscopic forceps connected to electrocautery (20 W). Make a 1-cm longitudinal incision on the anterior CBD wall (see Figure 3D).
- Insert the choledochoscope through the subxiphoid port into the CBD. Visualize and retrieve calculi using a stone retrieval basket (see Figure 3E).
- Inspect proximal and distal bile ducts for residual stones. Confirm duodenal papillary sphincter competence. Close the choledochotomy with a 5-0 polydioxanone suture (PDS) using continuous or interrupted sutures (1-2 mm spacing) (see Figure 3F,G).
- Place a sterile gauze pledget on the CBD to detect bile leakage. Complete the gallbladder resection using ultrasonic shears or electrocautery.
- Extract the gallbladder via the subxiphoid port. Conduct laparoscopic ultrasound (LUS) scanning along the extrahepatic bile duct axis in the hepatic hilum. Confirm the absence of residual calculi and ensure patency of biliary anastomosis without stricture (see Figure 3H).
- Insert a drainage tube into the subhepatic epiploic foramen (foramen of Winslow) through the 5-mm right anterior axillary port (see Figure 3I).
3. Postoperative care
- Continuously monitor heart rate, blood pressure, respiratory rate, and body temperature.
- Administer intravenous fluids to maintain hydration, electrolyte balance, and acid-base equilibrium. Administer IV antibiotics and hepatoprotective agents postoperatively.
- Initiate oral water intake 6 h postoperatively. Encourage early bedside mobilization to promote recovery.
- Maintain patency of drainage tubes. Monitor for bile leakage signs (e.g., yellowish drainage, abdominal distension).
Results
The procedure lasted 110 min with an intraoperative blood loss of 10 mL. The drainage tube was removed on postoperative day 4 (POD4), and the patient was discharged uneventfully on POD5. Intraoperative laparoscopic ultrasound (LUS) was employed to clearly delineate the cystic duct, common bile duct, and vascular anatomy and the size, quantity, and precise location of common bile duct stones (see Figure 4), enabling real-time intraoperative guidance. No perioperative complications-including bile leakage, hemorrhage, residual stones, or biliary stricture-were observed. During the 3-year postoperative follow-up, no significant surgery-related complications were identified. All these details are presented in Table 1.

Figure 1: CT images. (A,B) The images show cholecystolithiasis combined with choledocholithiasis. The yellow arrow represents gallbladder and cholecystolithiasis, and the red arrow represents common bile duct and choledocholithiasis. Please click here to view a larger version of this figure.
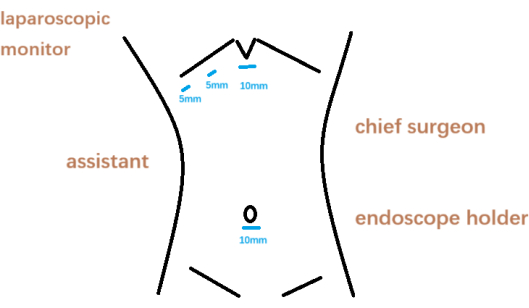
Figure 2: Surgeon position and puncture location. Please click here to view a larger version of this figure.
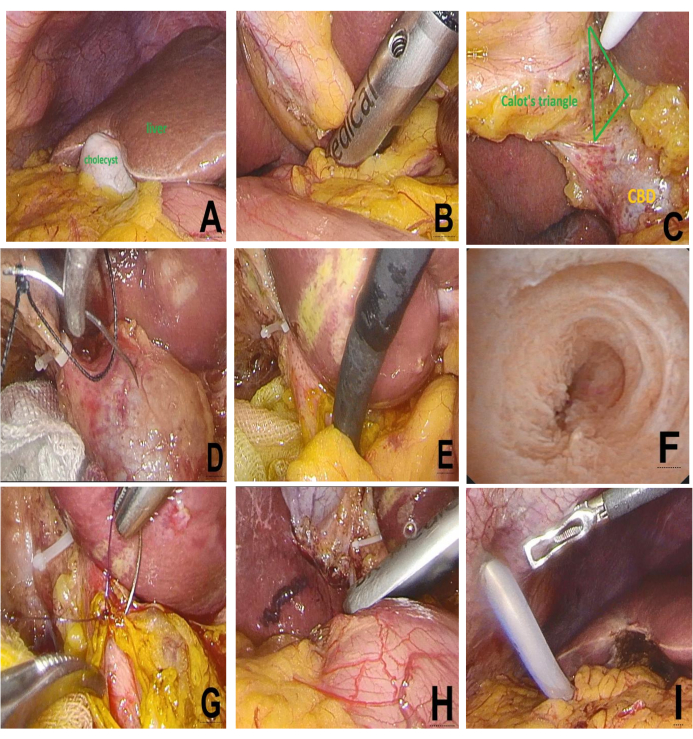
Figure 3: Intraoperative steps of LCBDE: (A) Laparoscopic exploration. (B) LUS evaluation. (C) Calot's triangle dissection. (D) Electrocautery CBD incision. (E) Choledochoscopic stone extraction. (F) Post-lithotomy CBD and papilla. (G) Primary CBD closure. (H) LUS re-evaluation. (I) Drain placement. Please click here to view a larger version of this figure.
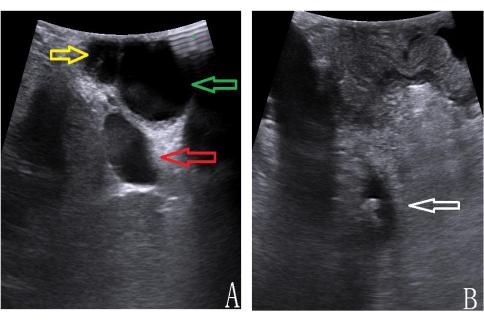
Figure 4: LUS imaging of hepatic portal anatomy. (A) cystic duct [yellow], CBD [green], portal vein [red]). (B) CBD stones [white arrow]. Please click here to view a larger version of this figure.
| Parameters | Results |
| Operative time | 110 min |
| Blood loss | 10 mL |
| Removal time of drainage tube | 4 days |
| Postoperative discharge time | 5 days |
| Bile leakage | No |
| Retained stone | No |
| Biliary stenosis | No |
| Follow-up time | 3 years |
| Recurrence of CBD stones | No |
Table 1: Surgical outcomes.
Discussion
LC+LCBDE and ERCP+LC are the primary minimally invasive approaches for gallbladder stones with common bile duct stones. Compared to ERCP, LCBDE offers advantages in managing larger stones, preserving papillary function, and avoiding staged procedures15,16.
The role of T-tube drainage post-LCBDE remains debated. While justified in cases of biliary hypertension, residual stones, strictures, or acute cholangitis, primary closure is recommended when biliary inflammation is mild, stone clearance is complete, and papillary function is intact17,18. Our center avoids routine biliary stenting to prevent stent migration, additional costs, and secondary removal procedures.
Laparoscopic surgery limits tactile feedback, increasing injury risks in edematous tissues or anatomical variants. Laparoscopic ultrasonography (LUS) overcomes this by providing real-time, high-resolution imaging of bile ducts and vasculature. Unlike transabdominal ultrasound, LUS is unaffected by abdominal wall thickness or bowel gas. Compared to intraoperative cholangiography, LUS is radiation-free and time-efficient, with a reported sensitivity of 96% and specificity of 100%19,20.
In this study, we performed laparoscopic common bile duct exploration (LCBDE) and ensured duct clearance with primary closure of the CBD using laparoscopic choledochoscopy and laparoscopic ultrasound (LUS). LUS was utilized to probe the cholecystic triangle, determine the position of the extrahepatic biliary tract, hepatic artery, and portal vein, and assess the location, size, and number of stones. It also provided intraoperative guidance.
Currently, common methods for incising the common bile duct (CBD) include scissors, blades, and electric hooks. Cutting with scissors or blades is prone to bleeding and requires additional hemostasis, while electric hooks may cause thermal injury to the bile duct wall due to heat conduction. In our approach, a 5-0 electrosurgical needle was used to incise the CBD. This technique minimized damage to the bile duct wall and effectively prevented bleeding. A choledochoscope was then employed to explore the biliary tract and remove stones. If the choledochoscopic examination confirmed no residual stones and normal duodenal papilla function, the CBD was closed with a 5-0 monofilament absorbable suture using continuous or interrupted full-thickness sutures (stitch spacing 1-2 mm, margin 1-2 mm), ensuring uniform tension-free closure. Dry sterile gauze sponges were applied to test for bile leakage. Laparoscopic ultrasound (LUS) was further utilized to assess for residual stones and evaluate the sutured bile duct for strictures. Subhepatic drainage tubes were routinely placed to promptly detect bile leakage and ensure adequate drainage. In the case described here, the drainage tube was removed on postoperative day 4, and the patient was discharged on day 5. No complications, such as bile leakage, hemorrhage, residual stones, or biliary strictures were observed.
However, in the implementation of the operation, it is necessary to grasp the indications strictly so as to maximize patient benefits. We have summarized the clinical experience and relevant literature reports21,22,23. There are 4 indications for primary biliary suture: (i) The biliary tract diameter ≥ 6 mm. A cholangioscope can enter the bile duct, which can not only remove stones but also reduce postoperative bile duct stenosis. (ii) For simple extrahepatic bile duct stones, a primary suture can be performed if stone removal is ensured. However, it is generally difficult to ensure complete stone removal for cases with combined intrahepatic bile duct stones, and primary suture is not recommended. (iii) The duodenal papilla has a good opening and closing function and no biliary stricture. (iv)The common bile duct wall is sutured evenly, accurately, and reliably without bile leakage or stenosis.
However, laparoscopic ultrasound also has its limitations. The probe of laparoscopic ultrasound is usually small in size, making it difficult to comprehensively observe a large area of tissue at one time. Only through the practical experience accumulated in laparoscopic surgical procedures and ultrasonic examination techniques can one truly master laparoscopic ultrasound technology. The laparoscopic ultrasound equipment is relatively expensive, which limits the widespread application of this technology in some resource-limited areas.
In conclusion, the application of LUS combined with a choledochoscope in laparoscopic surgery can ensure the effectiveness and safety of CBD primary closure.
Disclosures
The authors report no conflict of interest.
Acknowledgements
We thank the anaesthesiologists and operating room nurses who assisted with the operation.
Materials
| Name | Company | Catalog Number | Comments |
| Basket catheter | Guangzhou Manya Medical Technology Co., Ltd | WL-F65-115M | |
| Cholangioscope | Olympus | CHF-V | |
| Disposable laparoscopic trocar | Mindray | CW-Z346 | |
| Electrocautery hook | Visionstar | HV300B | |
| Laparoscopic system | KARL STORZ | 26003AA | |
| Laparoscopic ultrasound | BK Medical | 8666-RF | |
| Polydioxanone suture | ETHICON | Z303H | |
| Ultrasonic dissector | ETHICON | ACE+7 |
References
- Marilee-L, F., Robert-L, B., Andrew-J, D. Choledocholithiasis: Evolving standards for diagnosis and management. World J Gastroenterol. 12 (20), 3162-3167 (2006).
- Costi, R., Gnocchi, A., Di Mario, F., Sarli, L. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J. Gastroenterol. 20 (37), 13382-13401 (2014).
- Shojaiefard, A., Esmaeilzadeh, M., Ghafouri, A., Mehrabi, A. Various techniques for the surgical treatment of common bile duct stones: a meta review. Gastroenterol Res Pract. 2009, 840208 (2009).
- Naotaka, F., et al. Evidence-based clinical practice guidelines for cholelithiasis. J Gastroenterol. 58 (9), 801-833 (2023).
- Chen, C. C., et al. The fading role of T-tube in laparoscopic choledochotomy: primary choledochorrhaphy and over pigtail j and endonasobiliary drainage tubes. J Laparoendosc Adv Surg Tech A. 20 (10), 807-811 (2000).
- Zhang, H. W., Chen, Y. J., Wu, C. H., Li, W. D. Laparoscopic common bile duct exploration with primary closure for management of choledocholithiasis: A retrospective analysis and comparison with conventional T-tube drainage. Am Surg. 80 (2), 178-181 (2014).
- Podda, M., et al. Systematic review with meta-analysis of studies comparing primary duct closure and T-tube drainage after laparoscopic common bile duct exploration for choledocholithiasis. Surg Endosc. 30 (3), 845-861 (2016).
- Kurinchi, S. G., Rahul, K. T-tube drainage versus primary closure after laparoscopic common bile duct exploration. Cochrane Database Syst Rev. 21 (6), CD005641 (2013).
- Yan, Y. The safety and efficacy of primary duct closure without endoscopic nasobiliary drainage after laparoscopic common bile duct exploration. Gastrointest Tumors. 7 (4), 117-124 (2020).
- Brent, T. X. Biliary anatomy and variations. Surg Clin North A. 104 (6), 1137-1144 (2024).
- Onofrio, A. C., et al. Vascular and biliary variants in the liver: implications for liver surgery. Radiographics. 28 (2), 359-378 (2008).
- Wu, J. S., Peng, C., Mao, X. -. H., Lv, P. Bile duct injuries associated with laparoscopic and open cholecystectomy: sixteen-year experience. World J Gastroenterol. 13 (16), 2374-2378 (2007).
- Jamal, K. N., et al. Meta-analysis of the diagnostic accuracy of laparoscopic ultrasonography and intraoperative cholangiography in detection of common bile duct stones. Ann R Coll Surg Engl. 98 (4), 244-249 (2016).
- Omer, A., et al. Laparoscopic ultrasonography versus intra-operative cholangiogram for the detection of common bile duct stones during laparoscopic cholecystectomy: a meta-analysis of diagnostic accuracy. Int J Surg. 12 (7), 712-719 (2014).
- Rogers, S. J., et al. Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg. 145 (1), 28-33 (2010).
- Salminen, P., Laine, S., Gullichsen, R. Severe and fatal complications after ERCP: Analysis of 2555 procedures in a single experienced center. Surg Endosc. 22 (9), 1965-1970 (2008).
- Jiang, C., Zhao, X. H., Cheng, S. T-tube use after laparoscopic common bile duct exploration. JSLS. 23 (1), e2018.00077 (2019).
- Xie, W., et al. Is T-tube drainage no longer needed for laparoscopic common bile duct exploration? A retrospective analysis and literature review. Videosurgery. 18 (1), 99-107 (2023).
- Atstupens, K., Mukans, M., Plaudis, H., Pupelis, G. The role of laparoscopic ultrasonography in the evaluation of suspected choledocholithiasis. A single-center experience. Medicina. 56 (5), 246-260 (2020).
- Maple, J. T., et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 71 (1), 1-9 (2010).
- Estellés, V. N., et al. Eleven years of primary closure of common bile duct after choledochotomy for choledocholithiasis. Surg Endosc. 30 (5), 1975-1982 (2016).
- Guan, H., Jiang, G., Mao, X. Primary duct closure combined with transcystic drainage versus T-tube drainage after laparoscopic choledochotomy. ANZ J Surg. 89 (7-8), 885-888 (2019).
- Khaled, Y. S., et al. Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis. Surg Endosc. 27 (11), 4164-4170 (2013).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved