Method Article
Hemodynamic Precision in the Neonatal Intensive Care Unit using Targeted Neonatal Echocardiography
* Wspomniani autorzy wnieśli do projektu równy wkład.
W tym Artykule
Podsumowanie
Presented here is a protocol to perform comprehensive neonatal echocardiography by trained neonatologists in the neonatal intensive care unit. The trained individuals provide longitudinal assessments of heart function, systemic and pulmonary hemodynamics in a consultative role. The manuscript also describes the requirements to become a fully trained neonatal hemodynamics specialist.
Streszczenie
Targeted neonatal echocardiography (TnECHO) refers to the use of comprehensive echocardiographic evaluation and physiologic data to obtain accurate, reliable, and real-time information on developmental hemodynamics in sick newborns. The comprehensive assessment is based on a multiparametric approach that overcomes the reliability issues of individual measurements, allows for earlier recognition of cardiovascular compromise and promotes enhanced diagnostic precision and timely management. TnECHO-driven research has led to an enhanced understanding of the mechanisms of illness and the development of predictive models to identify at-risk populations. This information may then be used to formulate a diagnostic impression and provide individualized guidance for the selection of cardiovascular therapies. TnECHO is based on the expert consultative model in which a neonatologist, with advanced training in neonatal hemodynamics, performs comprehensive and standardized TnECHO assessments. The distinction from point of care ultrasonography (POCUS), which provides limited and brief one-time assessments, is important. Neonatal hemodynamics training is a 1-year structured program designed to optimize image acquisition, measurement analysis, and hemodynamic knowledge (physiology, pharmacotherapy) to support cardiovascular decision-making. Neonatologists with hemodynamic expertise are trained to recognize deviations from normal anatomy and appropriately refer cases of possible structural abnormalities. We provide an outline of neonatal hemodynamics training, the standardized TnECHO imaging protocol, and an example of representative echo findings in a hemodynamically significant patent ductus arteriosus.
Wprowadzenie
Targeted neonatal echocardiography (TnECHO) refers to the bedside use of echocardiography to longitudinally assess myocardial function, systemic and pulmonary blood flow, and intracardiac and extracardiac shunts1. When TnECHO is integrated with clinical findings, it can provide vital information in diagnosis, the guidance of therapeutic interventions, and the dynamic monitoring of response to treatments2. TnECHO is frequently performed by trained neonatologists in response to a specific clinical question with the goal of acquiring hemodynamics information that can complement and provide physiologic insights into the clinical status of the patients, resulting in precise cardiovascular care3. Over the past 10-15 years, TnECHO services have been incorporated in multiple tertiary neonatal intensive care units (NICUs) in Australia, New Zealand, Europe, and North America, especially in the management of complex high-acuity cases4,5,6,7,8. To date, there are eight centers in the USA with trained practitioners providing TnECHO services and a growing number of centers involved in neonatal hemodynamics research. Furthermore, the establishment of the neonatal hemodynamics and TnECHO special interest group (SIG) at the American Society of Echocardiography (ASE) reinforces the academic collaboration with pediatric cardiology and creates a strong political platform for further growth in the field9.
Neonatal hemodynamics training is designed to ensure that individuals who have received the training can achieve high-level imaging and provide comprehensive cardiovascular decision-making. In 2011, training recommendations for TnECHO, endorsed by European and North American professional organizations, were published3. Currently, more than 50 North American neonatologists have completed formal training in TnECHO; of note, more than 50% of hemodynamic clinicians are considered emerging academic leaders in the field, which is an unanticipated but much-needed benefit of formal training. Figure 1 summarizes hemodynamics training and accreditation.
The essential elements of a TnECHO service include access to a dedicated echocardiography machine. This ensures immediate availability for image acquisition and allows longitudinal follow-up (Figure 2 and Figure 3). The database/image archive must include the ability to provide immediate playback without video degradation, standardized reports, and long-term storage as per the recommendations of the Intersocietal Commission for the Accreditation of Echocardiography Laboratories10. A standard TnECHO includes key measurements that allow comprehensive assessments of intricate cardiovascular physiology during the neonatal period. This includes left ventricular (LV) function, right ventricular (RV) function, intracardiac shunt (atrial-level shunt and ductal-level shunt), the hemodynamic effects of patent ductus arteriosus (PDA), right ventricular systolic pressure (RVSp)/pulmonary artery (PA) pressure, systemic and pulmonary blood flow, the presence of pericardial fluid, thrombus, and central line position. Table 1 shows the commonly used echocardiographic terms utilized to acquire some of the data for these measurements. The evaluation may be performed for both symptom- and disease-based indications. Supplementary File 1 and Table 2 outline the comprehensive neonatal echocardiography assessments with recommended measurements, interpretation, and reference ranges for term neonates in the first 7 postnatal days.
The evaluation of LV systolic function is a key component as it assists in the delineation of the etiology and management of hemodynamic instability in critically ill neonates. Quantitative assessment is recommended as qualitative assessment is prone to inter-observer and intra-observer variability11. The calculation of the ejection fraction using a multi-plane method such as Simpson's biplane or the area-length method is superior to M-mode estimations, which may miss regional wall motion abnormalities and is inaccurate in the presence of septal flattening12. LV diastolic dysfunction is an emerging concept in neonatal hemodynamics. However, the data remain limited13.
An assessment of RV function is crucial in neonatal life because the RV is the dominant ventricle in transitional circulation, and many neonatal diseases are associated with right heart pathology. For a similar reason, in the assessment of LV systolic function, subjective assessment should be avoided14. However, due to the RV's unusual shape, highly trabeculated surface, and position wrapped around the LV, the measurement of RV function is more difficult. Despite this, several reliable quantitative parameters have been studied, and normative data have been published15,16. Fractional area change (FAC) and tricuspid annular plane systolic excursion (TAPSE) are two of the recommended quantitative measurements used17.
Intracardiac shunt (atrial and ductal level) is another important aspect of the comprehensive neonatal echocardiography assessment. In most situations, left atrial pressures are higher in comparison to right atrial (RA) pressures, resulting in a left-to-right shunt. However, in the neonatal period, a bidirectional shunt can still be normal. Elevated right-sided filling pressures, especially in association with pulmonary hypertension (PH), should be considered when there is right-to-left shunting at the atrial level, but this should not be used in isolation given that variation in ventricular compliance/pressure may also influence atrial pressure at various points during the cardiac cycle.
An assessment of patent ductus arteriosus (PDA) should include the determination of ductal shunt direction and the measurement of ductal pressure gradients, which are used to assist in treatment decisions. An arch-sidedness evaluation is also important, especially when there is consideration of surgical PDA ligation. PDA shunt direction is reflective of the difference between aortic and PA pressures, as well as the relative resistance of the pulmonary and systemic circulation. One factor used to adjudicate hemodynamic significance is the presence of holodiastolic retrograde flow in the descending thoracic or abdominal aorta18. Hemodynamic significance can be further assessed by quantifying the degree of volume overload by comprehensive measurements19. Scoring systems that assess the surrogate consequences of volume loading on the heart and the systemic hypoperfusion associated with PDA shunt, such as the Iowa PDA score, have been published (Table 3)19,20,21 The Iowa PDA score has been adopted clinically at the University of Iowa to enhance objectivity in determining the hemodynamic significance of a PDA shunt. A score of more than 6 is suggestive of a hemodynamically significant patent ductus arteriosus (hsPDA)19.
In the assessment of pulmonary hemodynamics, the absolute value of RVSp is estimated by the measurement of the tricuspid regurgitant (TR) gradient. Continuous wave Doppler is used to measure the maximal tricuspid regurgitation velocity through the tricuspid valve, referred to as the tricuspid regurgitant peak velocity. An assumed RA pressure of 5 mmHg is typically used for the calculation. The RVSp is then calculated using the simplified Bernoulli equation22:
RVSp = 4 × (tricuspid regurgitant peak velocity [m/s])2 + RA pressure
Occasionally an alternative, the Doppler-derived pressure gradient across a PDA, is used for the calculation of PA (pulmonary artery) pressures23. However, a TR jet is only present in approximately 50% of patients with chronic PH24,25,26. In these situations, measurements such as the end-systolic eccentricity index (sEI), which is a measure of LV circularity, may indicate the relative pressure between the ventricles. This measurement should be interpreted with caution in patients with systemic hypertension as the mild disease may go undetected due to elevated LV end-diastolic pressure. Figure 4 gives an example of an algorithm and comprehensive neonatal echocardiography assessment guidelines for pulmonary hypertension.
For the assessment of LV stroke volume, a pulse Doppler tracing in an apical five-chamber view at the level of the aortic valve is measured to obtain the time-velocity integral (TVI). This is combined with a measurement of aortic annulus diameter in the parasternal long-axis view. A calculation with the following formula is used to estimate LV output27:
LV output (mL/min/kg) = (TVI [cm] × π x [D/2]2 [cm2] × heart rate)/weight.
However, in the presence of a PDA, the LV output measurement is not reflective of systemic blood flow secondary to the shunting at the PDA level3. The diastolic flow to peripheral organs by Doppler interrogation of the celiac artery, superior mesenteric artery, and middle cerebral artery can give an indication of a systemic steal by a PDA but may, alternately, reflect organ resistance, with low or absent diastolic flow seen in the setting of high resistance.
TnECHO can also be utilized to assist in detecting the presence of intracardiac thrombus, pericardial fluid, and its hemodynamic significance, guiding pericardiocentesis, as well as assisting in the placement of peripheral arterial lines, peripherally inserted central catheters, and umbilical venous catheters28. Here, to show the comprehensive approach to obtaining TnECHO and the hemodynamics information, we describe the imaging protocol and the elements of a TnECHO service (Figure 3).
Protokół
This protocol was approved by the institution's human research ethics committee, and written consent was obtained from the patient before the procedure.
1. Preparation
- For image acquisition, use ultrasound systems that include two-dimensional (2D), M-mode, and full Doppler capabilities, as well as simultaneous electrocardiographic tracing display ability.
- Ensure that multi-frequency probes, 5-6 MHz (for infants >2 kg) and 8-12 MHz (for infants <2 kg), are available for use in the appropriate size of infants. Commonly used echocardiographic terms are described in Table 1 with Supplementary File 1, depicting examples of probe placement and the corresponding representative echocardiographic views.
NOTE: The first echocardiography study includes a full morphologic and hemodynamic assessment of cardiac anatomy and physiology using a segmental approach as per the American Society of Echocardiography (ASE) guidelines11.
2. Preparing the patient for echocardiography evaluation
- Follow the institution's specific infection control precaution guidelines for the prevention of infection to the patients.
- Un-swaddle and expose the baby's chest and upper abdominal area, carefully move any leads that may be in the way and pay particular attention to skin integrity.
- Maintain the body temperature of the patient and the neutral thermal environment by the minimal opening of the incubator.
- Ensure continuous cardiorespiratory monitoring during the scan.
3. Probe and image acquisition
- Plug in the echocardiography machine, attach the EKG cord and warm the ultrasound gel to 102 ˚F while waiting for the machine to boot up.
- Ensure a patient identifier such that the imaging is linked to the appropriate patient chart.
- Choose a probe appropriate for the patient size (a 6S-D cardiac sector ultrasound transducer for a patient ≥2 kg; a 12S-D cardiac sector ultrasound transducer for a patient <2 kg).
NOTE: This protocol describes a case using a 12S-D transducer. - Adjust the depth and brightness of the images.
- Click the image store after each step outlined below for the images to be saved.
NOTE: A minimum of 3 cardiac cycles should be obtained.
4. Image acquisition
- Apical views
- Start with the apical four-chamber view. Place the probe on the apex with the position marker (notch) angling toward the left shoulder (see Supplementary File 1). Click 2D to start the first image. Click the up/down button on the interactive touch screen to orientate the apex of the heart at the bottom of the screen.
NOTE: In infants with evolving chronic lung disease, this view is sometimes obtained more laterally and, on some occasions, more medially. The sector width may need to be widened to allow complete visualization of the bilateral ventricular walls by turning the width reset button clockwise. - The image acquired shows the four chambers of the heart. Once the optimal view is obtained, adjust the gain, depth, and grayscale to optimize the image quality. Adjust the depth by turning the depth knob on the console to reach a depth of 3.5 cm to complete the visualization of the atria and ventricles. Click the image store to save the 2D image.
- Click color on the console. Place the color box over the tricuspid valve using the trackball. Adjust the velocity reset to a color scale of 70-80 cm/s.
NOTE: The blue regurgitant jet through the tricuspid valve during systole is evidence of tricuspid regurgitation. - Click cursor, and then use the trackball to place the sample gate over the tricuspid valve. Click CW button to obtain the tricuspid regurgitant peak velocity. Click freeze > image store.
- Click 2D to reset the screen. Click color > simultaneous buttons to activate color Doppler. Use the trackball to place the color box over the pulmonary veins.
- Adjust the velocity and decrease the color Doppler to 50-60 cm/s. Click cursor, place the sample gate over the pulmonary vein and click PW to obtain the pulsed wave. To save, click freeze > image store.
NOTE: A pulmonary venous flow velocity trace recorded by Doppler echocardiography is often described in three components, which are the systolic component (S), followed by the diastolic component (D), and there might be flow reversal during atrial contraction (A) in some cases. - Click 2D to reset the image. Click cursor and place the sample gate at the tips of the open mitral valves. Click PW to obtain the mitral valve E/A. Click freeze > image store.
- Click 2D to reset the screen and then click color > simultaneous to activate the color Doppler. Increase the color box to cover just above the mitral valve to the apex. Perform the settings as in step 4.1.3. Click image store.
- Rotate the probe clockwise to open and visualize the left ventricular outflow tract. Click cursor and place the sample gate at the mitral inflow and outflow junction, and then click PW to obtain the pulsed wave. Click freeze > image store to save the image.
- Click 2D to reset the image with an open left ventricular outflow tract (LVOT). Place the sample gate at the aortic valve and repeat step 4.1.9 for image capture.
NOTE: When performing a measurement of the isovolumetric relaxation time (IVRT), it is optimal to decrease the sweep speed (25-50 mm/s) such that the interval between the end of systole and the beginning of diastole is seen. - To focus on the LVOT, turn the width button to narrow the sector width, place the sample gate over the aortic valve at the level of the hinge points, and repeat step 4.1.9.
NOTE: It may be necessary to rotate clockwise and/or move toward the left hip to optimally align the LVOT; it is essential for accurate measurement of the left ventricular output that the line of insonation is parallel to the LVOT. Tracing the envelope is required for the calculation of the velocity time integral (VTI).
- Start with the apical four-chamber view. Place the probe on the apex with the position marker (notch) angling toward the left shoulder (see Supplementary File 1). Click 2D to start the first image. Click the up/down button on the interactive touch screen to orientate the apex of the heart at the bottom of the screen.
- Tissue doppler imaging from Apical four-chamber view
- Click 2D to reset the image. Click image store to save the 2D image.
- Click the TVI button on the console to activate tissue Doppler imaging. Click image store to save the image apex to base.
- Turn the width button to narrow the sector width to interrogate the septum with a target frame rate of >200 frames/s (fps). Place the sample gate below the mitral valve annulus in the wall of the septum and repeat step 4.1.9.
NOTE: This provides a tissue velocity curve from the valve annulus with positive velocity in systole and negative velocity in diastole. The peak velocity in systole is S', early diastole is E', and late diastole during atrial contraction is A'. For all the tissue Doppler imaging (TDI) myocardial velocities, ensure to align the cursor with the ventricular wall such that the velocity measured is the movement from the ventricular apex to the base of the ventricles. - Click 2D on the interactive touch screen, click Tilt to move the sector to focus on the lateral wall of the left ventricle and maintain the frame rate at >200 fps. Place the sample gate over just below the mitral valve annulus in the wall and repeat step 4.1.9.
- Move the sector to focus on the lateral wall of the RV. Click 2D on the interactive touch screen. Click Tilt, place the sample gate in the lateral wall of the RV and repeat step 4.1.9.
- While still in tissue Doppler mode, click cursor and use the trackball to place the line of insonation at the tricuspid valve annulus, perpendicular to the free wall hinge point of the tricuspid valve. Click the M-mode button on the console for tricuspid annular plane systolic excursion (TAPSE) and repeat step 4.1.9. This is measured either with or without a TDI map.
- Click 2D on the console to reset the image. Transition to the apical two-chamber view by counterclockwise rotation of the probe (approximately 1 o'clock) and click image store for 2D images. Click TVI > image store to obtain TDI images.
- For apical three-chamber LV view, turn the probe counterclockwise (approximately 11 o'clock) and click image store. Click TVI button > image store. Repeat step 4.1.9.
- Turn width button, narrow the sector to the anterior wall and repeat step 4.1.9.
- Apical three-chamber RV view
NOTE: The apical three-chamber RV view is obtained by placing the probe on the left sternal border in the fourth intercostal space with the notch pointing toward the left axilla. Movement along the sternal border may be necessary to adjust the image to show the RV inlet and outflow tracts.- Click the 2D button to reset the image, turn the width button for complete visualization of the RV lateral wall, click image store to save the image, click color. Use the trackball to place the color box over the tricuspid valve. Place the sample gate over the tricuspid valve where the blue jet is observed and repeat step 4.1.4.
- Use the trackball to move the color box over the pulmonary artery. Click cursor and place the sample gate over the pulmonic valve. Click PW and CW to obtain the pulsed and continuous wave Doppler of the right ventricular outflow. Click freeze > image store.
- Parasternal long-axis view
NOTE: For obtaining an optimal parasternal long-axis view , place the probe straight down on the third or fourth intercostal space just to the left of the sternum with the notch pointing toward the right shoulder. Ensure that the probe is rotated anticlockwise or clockwise to obtain the full length of the left ventricle, mitral valve, aortic valve, and right ventricle.- Click 2D and the up/down tab on the interactive control to orient the right ventricle at the top of the screen. Click image store > cursor. Place the line of insonation through the left ventricle at the tips of the mitral valve leaflets, ensuring that the line is perpendicular to the interventricular septum and that the left ventricle is not foreshortened. Click M-mode > freeze > image store.
NOTE: The M-mode tracing shows the biphasic opening and closing of the mitral valve, as well as the dimensions of the interventricular septum, left ventricular cavity, and posterior walls of the right and left ventricles in both systole and diastole. This image is used to calculate the ejection fraction and fractional shortening29. - Click 2D to reset the image. Turn the width button and focus on the aortic valve. Turn the depth knob to adjust the depth (2.5-3 cm) or turn the zoom button on the console to view the aortic annulus. Ensure that both leaflets are visualized such that the diameter is measurable.
- Click cursor and place the line of insonation through the aortic valve annulus and left atrium for left atrium and aortic dimensions (at the hinge points). Click M-mode > freeze > image store.
- Click 2D and angle the probe toward the left shoulder to focus on the pulmonary artery. Click color > simultaneous to obtain an image of the right ventricular outflow tract.
- Place the sample gate over the pulmonic valve at the hinge point and repeat step 4.1.9. Place the sample gate over the tricuspid valve and repeat step 4.1.4.
NOTE: It may be necessary to move slightly toward the left shoulder to elongate the right ventricular cavity. As with the other views of the right ventricle, if there is tricuspid regurgitation, obtain a continuous wave Doppler to calculate the TR.
- Click 2D and the up/down tab on the interactive control to orient the right ventricle at the top of the screen. Click image store > cursor. Place the line of insonation through the left ventricle at the tips of the mitral valve leaflets, ensuring that the line is perpendicular to the interventricular septum and that the left ventricle is not foreshortened. Click M-mode > freeze > image store.
- Parasternal short-axis view
NOTE: Obtain the parasternal short-axis view by placing the probe in a sagittal position in the third or fourth intercostal space just to the left of the sternum with the notch pointing toward the left shoulder and with all three valves opening (aortic, pulmonic, and tricuspid valves). Obtain a 2D image of the right ventricular inflow and outflow.- Activate the color Doppler as in step 4.1.5. Perform the settings of step 4.1.3. Place the sample gate over the tricuspid valve where the blue jet is observed and repeat step 4.1.4. Place the sample gate over the pulmonic valve at the hinge points and repeat step 4.1.9.
- Click freeze to unfreeze the image. Click cursor and place the line of insonation over any regurgitant jet (red coloration) over the pulmonic valve. Click CW and repeat step 4.1.9.
- Click 2D to reset the image. Continue angling the probe toward the left flank until the fish-mouth appearance of the mitral valve is visualized. Place the line of insonation through the mitral valve at the level of the mitral valve leaflets and repeat step 4.4.3. This view is also used to calculate the ejection fraction and fractional shortening.
- Click 2D on the console and reset the image. Continue the 2D sweep (25-50 mm/s) toward the left flank at the apex of the left ventricle; obtain 2D images at the level of the papillary muscles (used to calculate the eccentricity index) and the apex. Click freeze > image store.
- High parasternal view
NOTE: With the infant's head turning toward the left shoulder, place the probe along the upper right border of the sternum with slight clockwise rotation from the sagittal plane and with the marker pointing toward the head.- Activate the color Doppler as in step 4.1.5. Perform the settings of step 4.1.3. Click image store to acquire simultaneous 2D and color images while ensuring that the three proximal branches of the aorta are visible.
- Place the sample gate at the preductal aortic arch, ensuring the line of insonation is parallel to the flow, and then at the postductal arch below the level of the ductus, ensuring the line of insonation is parallel to the flow, and repeat step 4.1.9.
- To obtain the ductal view with a color sweep of PDA, click freeze button twice. Move the probe in an angling motion from the aortic arch toward the pulmonary artery by angling the probe toward the right flank. Click freeze > select all > image store.
- In the presence of a patent ductus arteriosus (PDA), click cursor, place the sample volume at the narrowest point of the PDA, and repeat step 4.1.9.
- Branch pulmonary artery view
NOTE: This view is obtained by placing the probe along the upper 2/3 to the left of the sternum at a 3 o'clock position. The probe marker is directed to the left of the patient. It may be necessary to move toward the head to navigate poor acoustic windows, particularly for patients with apical lung overdistension, such as with chronic ventilation.- Angle the probe toward the patient's head to reveal the branch pulmonary arteries with the same setting of the screen as the aortic arch view. Place the sample volume through the right pulmonary artery (RPA), ensuring the line of insonation is parallel to the flow, and repeat step 4.1.9. If the peak systolic velocity is >1.5 m/s, repeat 4.1.4.
NOTE: This is performed to evaluate for peripheral pulmonic stenosis (PPS). - Repeat the same steps on the left pulmonary artery (LPA).
- Angle the probe toward the patient's head to reveal the branch pulmonary arteries with the same setting of the screen as the aortic arch view. Place the sample volume through the right pulmonary artery (RPA), ensuring the line of insonation is parallel to the flow, and repeat step 4.1.9. If the peak systolic velocity is >1.5 m/s, repeat 4.1.4.
- Pulmonary vein view: crab view
NOTE: This view is obtained by placing the probe in the suprasternal notch, perpendicular to the sagittal plane. With the marker pointing toward the left of the patient, angle the probe toward the patient's head to reveal the pulmonary veins.- Turn the width button clockwise to increase the sector width, then, turn the velocity knob counterclockwise to adjust the color Doppler gain to 30-50 cm/s, click image store to obtain the image. Interrogate each pulmonary vein with color flow Doppler, place the sample gate on the pulmonary vein, and repeat step 4.1.9. Repeat this step until all the pulmonary veins are interrogated.
- Subcostal view
NOTE: The subcostal view is obtained by placing the probe at the epigastrium area of the abdomen. With the probe marker pointing to the left of the infant, angle the probe toward the patient's abdomen. Once visualization of both the right atrium and the left atrium is obtained, ensure that at least 1/3 of the image is of the liver for the optimization of this view.- Click 2D > up/down on the interactive screen. Ensure that the right atrium is oriented at the bottom part of the screen. Turn the width button. Click color > simultaneous. Turn the velocity knob to adjust the color gain to 40-50 cm/s. If the foramen ovale is patent, place the sample gate at the defect and repeat step 4.1.9.
- To visualize the superior vena cava (SVC), turn the probe by clockwise rotation. Click cursor and place the sample volume approximately 1 cm within the SVC, ensuring the line of insonation is parallel to the flow. Click freeze > image store.
- Click up/down on the interactive screen to reorientate the screen so that the heart is positioned on the right side of the screen. Position the probe in the sagittal plane with the notch pointing toward the head of the patient. Angle the probe tilting toward the left of the patient to visualize the IVC and the hepatic vein. Place the sample gate at the hepatic vein and repeat step 4.1.9.
- To view the position of an umbilical vein catheter (UVC) or lower limb peripherally inserted central catheter (PICC), slide the probe up toward the middle of the chest until the catheter is visualized in the image sector. A sweep from the right or left or rotation counterclockwise is necessary to view the course of the catheter. Click image store to obtain the image once the appropriate view of the central catheter has been visualized.
- Transition to the sagittal view of the abdominal aorta by sliding the probe toward the umbilicus in the sub-xiphoid area with the notch pointing toward the head. Adjust the color gain to 70-80 cm/s. Place the sample gate over the celiac artery and repeat step 4.1.9. Repeat the same steps for the superior mesenteric artery (SMA).
Wyniki
The following representative results outline the evaluation of a hemodynamically significant patent ductus arteriosus (hsPDA) as an example of the use of TnECHO in clinical settings. As mentioned earlier, a comprehensive assessment with multiple measurements is performed to adjudicate hemodynamic significance. The Iowa PDA score (Table 3) is one of the scoring systems adopted into clinical use as it assists in quantifying the consequences of volume loading and systemic hypoperfusion associated with PDA shunt.
The assessment consists of apical four-chamber views where pulmonary vein D wave velocity, mitral valve E wave velocity, and IVRT are obtained. Elevated velocities of the mitral valve E wave and pulmonary vein D wave indicate evidence of left heart volume overload, as well as a shortened IVRT. The velocities are documented in centimeters per second (cm/s). The time measurement is documented in milliseconds (ms). Left ventricular outflow is then assessed. An increase in left ventricular output is also suggestive of an increase in left heart volume loading. In the parasternal long axis view, the left atrium/aorta ratio (LA:Ao ratio) is then evaluated. An elevated LA:Ao ratio is indicative of left atrial dilatation, consistent with left heart volume overload. The high parasternal view allows for the assessment of PDA size, directionality, shunt patterns, as well as shunt effects on the blood flow supplying the descending aorta. Systemic hypoperfusion is then assessed by Doppler imaging of the celiac artery, superior mesenteric artery (SMA), and middle cerebral artery (MCA).
The echocardiographic results are then rated using the rating system such as the Iowa PDA score, as illustrated in Table 3. The scoring system then allows for quantitative assessment of the hemodynamic significance of the PDA, with an Iowa PDA score above 6 being suggestive of hemodynamically significant PDA.
The following is a case vignette to illustrate the echocardiography performed using this protocol.
A male premature infant was born at the gestational age of 29 weeks. He received the TnECHO evaluation at 2 days of life for the assessment of the hemodynamic significance of PDA. The measurements of the TnECHO showed the following results in Table 4, which gave the Iowa PDA score of 8, suggestive of hemodynamically significant PDA.
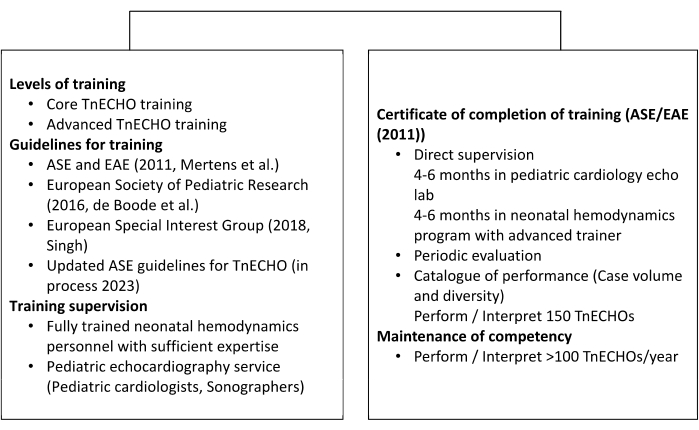
Figure 1: Summary of neonatal hemodynamics training and accreditation. A brief outline of targeted neonatal echocardiography and neonatal hemodynamics training for North America, USA. This figure has been modified from 3 and published with permission. Please click here to view a larger version of this figure.
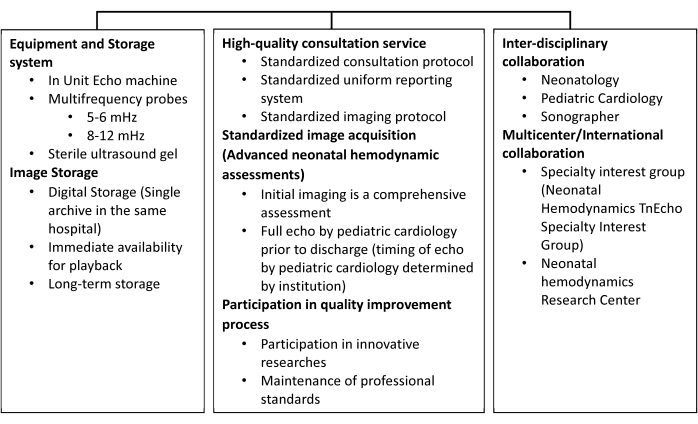
Figure 2: Elements of a neonatal hemodynamics consultation service. An outline detailing the equipment and storage systems and interdisciplinary collaborations of a neonatal hemodynamics service. This figure has been modified from 30 and republished with permission. Please click here to view a larger version of this figure.

Figure 3: Indications for neonatal hemodynamics consultation. An outline of symptom- and disease-based indications. This figure has been modified from 30 and republished with permission. Please click here to view a larger version of this figure.

Figure 4: TnECHO assessment guideline for pulmonary hypertension. An example of an algorithm and TnECHO assessment guideline for pulmonary hypertension. Please click here to view a larger version of this figure.
Table 1: Definitions of commonly used ultrasound modalities/terms. This list provides definitions of the ultrasound modalities described in this protocol. Please click here to download this Table.
Table 2: Standard targeted neonatal echocardiographic assessments with recommended measurements, interpretations, and reference range for term neonates. An outline of targeted neonatal echocardiographic assessments with recommended measurements, interpretations, and reference range. Abbreviations: CW = continuous wave; LA = left atrial; LVOT = left ventricular outflow tract; MV = mitral valve; PW = pulsed wave; RVOT right ventricular outflow tract; 3D = three-dimensional. This figure has been modified from 3 and published with permission. Please click here to download this Table.
Table 3: Echocardiographic markers evaluated to determine the Iowa PDA score. This scoring system assesses the surrogate consequences of volume loading on the heart and systemic hypoperfusion associated with patent ductus arteriosus shunt. Total score = (total points) + (PDA diameter [mm]/weight [kg] at echocardiography). This figure has been modified from 19 and published with permission. Please click here to download this Table.
Table 4: Representative results of a case vignette to illustrate echocardiography performed using the protocol and the Iowa PDA score. With measurements obtained from TnECHO, the measurements are then used to score based on the Iowa PDA score. The results gave an Iowa PDA score of 8, suggestive of hemodynamically significant PDA. Please click here to download this Table.
Supplementary File 1: Standard targeted neonatal echocardiographic measurement with probe placement. This table outlines the targeted neonatal echocardiographic assessments with probe placement, representative echo images, and measured parameters. Abbreviations: LPA = left pulmonary artery; LVO = left ventricular output; PDA = patent ductus arteriosus; RV = right ventricle; VSD = ventricular septal defect. Please click here to download this File.
Dyskusje
TnECHO-guided care has been adopted in many neonatal intensive care units as an adjunct to the clinical assessment of hemodynamic instability in infants by neonatologists4. Accredited training programs have been developed in accordance with the 2011 ASE3 with a focus on a competence-based approach to training. The unique vulnerability of the immature cardiovascular system and the complexity of cardiovascular adaptation during the postnatal transition are key determinants of hemodynamic stability, which highlights the importance of comprehensive and accurate serial TnECHO evaluation7,31.
It is critical to note that the first echocardiography study consists of a full morphologic and hemodynamic assessment of cardiac anatomy and physiology using a segmental approach as per the American Society of Echocardiography (ASE) guidelines. Revision by a pediatric cardiologist should also be performed within 12 h to confirm normal cardiac anatomy. Subsequent echocardiography evaluation then follows a standardized protocol mentioned previously in this article. In addition, the abstraction of clinical (history and examination) information should be systematic to formulate a diagnostic impression and therapeutic recommendation. With recent evidence highlighting the limitations of subjective assessment14, the use of a multiparametric hemodynamic approach allows for quantitative analysis, thus increasing the refinement of clinical decision-making32.
A modified imaging protocol is sometimes necessary in the setting of an acutely decompensating patient (e.g., pre-extracorporeal membrane oxygenation status). In this setting, the most critical images should be quickly obtained (e.g., left and right ventricular outputs, RV and LV function, aortic arch, and PDA and patent foramen ovale [PFO] patency and direction) to facilitate emergent hemodynamic rescue. An existing caveat is to recognize that TnECHO is used as a noninvasive tool to provide additional information on the underlying cardiovascular pathophysiology in infants with hemodynamic instability and in monitoring response to therapy. It is, therefore, important to appreciate that TnECHO is neither a substitute nor equivalent for the evaluation of congenital cardiac defects with an echocardiogram by a qualified pediatric cardiologist. Along the same lines, caution should be taken with the application of cardiac point of care ultrasound (cardiac POCUS), which is a limited one-time assessment indicated for specific indications such as the detection of pericardial tamponade or the assessment of central catheter position.
Over the past few years, technical advances have allowed for rapid growth in the field of neonatal hemodynamics with more sophisticated echocardiographic evaluations such as deformation analysis and blood speckle imaging, which might carry the potential for neonatal use. These ongoing advancements in targeted neonatal echocardiography and neonatal hemodynamics, especially in the understanding of the accuracy, feasibility, reliability, and limitations of the method, can yield significant clinical improvement in the care of our most vulnerable patients in the future7,27.
Ujawnienia
The authors have nothing to disclose and no conflicts of interest.
Podziękowania
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. M.M. is supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R25MD011564.
Resources for the figures, reference values, and training recommendations were adapted from Ruoss et al.30, the TnECHO teaching manual47, the Neonatal Hemodynamics Research Center (NHRC)48, and the Targeted neonatal echocardiography application49.
Materiały
| Name | Company | Catalog Number | Comments |
| DICOM VIEWER EP | GEHealthcare | H45581CC | DICOM Viewer on MediaThis option provides the ability to export DICOM images including a DICOM viewer to storage media (USB, DVD), for easy access to patient images on offline computers. |
| 2D Strain | GEHealthcare | H45561WF | Automated 2D EF Measurement tool based upon 2D-Speckle tracking algorithm. |
| EchoPAC* Software Only v203 | GEHealthcare | H8018PF | |
| EchoPAC* Advanced Bundle Package | GEHealthcare | H8018PG | Advanced QScan provides dedicated parametric imaging applications for quantitative display of regional wall deformation. |
| Multi-Link 3-lead ECG Care cable neonatal DIN, AHA (3.6 m/12 feet) | GEHealthcare | H45571RD | Multi-Link 3-lead ECG Care cable neonatal DIN, AHA (3.6 m/12 feet) Used together with neonatal leads H45571RJ |
| Myocardial Work | H45591AG | Myocardial Work adjusts the AFI (strain) results using the systolic and diastolic blood pressure measured immediately prior to the echo exam. Using the Myocardial Work feature helps achieve a less load dependent strain/ pressure curve and work efficiency index | |
| 12S-D Phased Array Probe | GEHealthcare | H45021RT | |
| 6S-D Phased Array Probe | GEHealthcare | H45021RR | |
| Sterile ultrasound gel | Parker labs | PM-010-0002D | sterile water solubel single packet ultrasound transmission gel |
| Ultrasound gel warmer | Parker Labs | SKU 83-20 | ultrasound gel warmer for single gel package. |
| Wireless USB adapter | H45591HS | Wireless external G type USB adapter with extension cable and hardware for mounting on the rear panel. | |
| Vivid* E90 v203 Console Package | GEHealthcare | H8018EB | Vivid E90 w/OLED monitor v203 Console |
Odniesienia
- Shah, D. M., Kluckow, M. Early functional echocardiogram and inhaled nitric oxide: Usefulness in managing neonates born following extreme preterm premature rupture of membranes (PPROM). Journal of Paediatrics and Child Health. 47 (6), 340-345 (2011).
- El-Khuffash, A., McNamara, P. J. Hemodynamic assessment and monitoring of premature infants. Clinics in Perinatology. 44 (2), 377-393 (2017).
- Mertens, L., et al. Targeted neonatal echocardiography in the neonatal intensive care unit: Practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). Journal of the American Society of Echocardiography. 24 (10), 1057-1078 (2011).
- Papadhima, I., et al. Targeted neonatal echocardiography (TNE) consult service in a large tertiary perinatal center in Canada. Journal of Perinatology. 38 (8), 1039-1045 (2018).
- Sehgal, A., McNamara, P. J. Does point-of-care functional echocardiography enhance cardiovascular care in the NICU. Journal of Perinatology. 28 (11), 729-735 (2008).
- El-Khuffash, A., Herbozo, C., Jain, A., Lapointe, A., McNamara, P. J. Targeted neonatal echocardiography (TnECHO) service in a Canadian neonatal intensive care unit: A 4-year experience. Journal of Perinatology. 33 (9), 687-690 (2013).
- Harabor, A., Soraisham, A. S. Utility of targeted neonatal echocardiography in the management of neonatal illness. Journal of Ultrasound in Medicine. 34 (7), 1259-1263 (2015).
- Evans, N. Echocardiography on neonatal intensive care units in Australia and New Zealand. Journal of Paediatric and Child Health. 36 (2), 169-171 (2000).
- McNamara, P., Lai, W. Growth of neonatal hemodynamics programs and targeted neonatal echocardiography performed by neonatologists. Journal of the American Society of Echocardiography. 33 (10), 15-16 (2020).
- Frommelt, P., et al. Digital imaging, archiving, and structured reporting in pediatric echocardiography: Impact on laboratory efficiency and physician communication. Journal of the American Society of Echocardiography. 21 (8), 935-940 (2008).
- De Geer, L., Oscarsson, A., Engvall, J. Variability in echocardiographic measurements of left ventricular function in septic shock patients. Cardiovasc Ultrasound. 13, 19 (2015).
- Margossian, R., et al. The reproducibility and absolute values of echocardiographic measurements of left ventricular size and function in children are algorithm dependent. Journal of the American Society of Echocardiography. 28 (5), 549-558 (2015).
- Harada, K., Takahashi, Y., Tamura, M., Orino, T., Takada, G. Serial echocardiographic and Doppler evaluation of left ventricular systolic performance and diastolic filling in premature infants. Early Hum Development. 54 (2), 169-180 (1999).
- Smith, A., et al. Accuracy and reliability of qualitative echocardiography assessment of right ventricular size and function in neonates. Echocardiography. 36 (7), 1346-1352 (2019).
- Koestenberger, M., et al. Systolic right ventricular function in preterm and term neonates: Reference values of the tricuspid annular plane systolic excursion (TAPSE) in 258 patients and calculation of Z-score values. Neonatology. 100 (1), 85-92 (2011).
- Jain, A., et al. A comprehensive echocardiographic protocol for assessing neonatal right ventricular dimensions and function in the transitional period: normative data and z scores. Journal of the American Society of Echocardiography. 27 (12), 1293-1304 (2014).
- Koestenberger, M., et al. Right ventricular function in infants, children and adolescents: Reference values of the tricuspid annular plane systolic excursion (TAPSE) in 640 healthy patients and calculation of z score values. Journal of the American Society of Echocardiography. 22 (6), 715-719 (2009).
- Groves, A. M., Kuschel, C. A., Knight, D. B., Skinner, J. R. Does retrograde diastolic flow in the descending aorta signify impaired systemic perfusion in preterm infants. Pediatric Research. 63 (1), 89-94 (2008).
- Rios, D. R., et al. Early role of the atrial-level communication in premature infants with patent ductus arteriosus. Journal of the American Society of Echocardiography. 34 (4), 423-432 (2021).
- de Freitas Martins, F., et al. Relationship of patent ductus arteriosus size to echocardiographic markers of shunt volume. The Journal of Pediatrics. 202, 50-55 (2018).
- Martins, F. F., et al. Relationship of patent ductus arteriosus echocardiographic markers with descending aorta diastolic flow. Journal of Ultrasound in Medicine. 40 (8), 1505-1514 (2021).
- Waggoner, A. D. Quantitative echocardiography. Journal of Diagnostic Medical Sonography. 21 (6), 464-470 (2005).
- Masuyama, T., et al. Continuous-wave Doppler echocardiographic detection of pulmonary regurgitation and its application to noninvasive estimation of pulmonary artery pressure. Circulation. 74 (3), 484-492 (1986).
- Mourani, P. M., Sontag, M. K., Younoszai, A., Ivy, D. D., Abman, S. H. Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics. 121 (2), 317-325 (2008).
- Fisher, M. R., et al. Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. American Journal of Respiratory and Critical Care Medicine. 179 (7), 615-621 (2009).
- Krishnan, U., et al. Evaluation and management of pulmonary hypertension in children with bronchopulmonary dysplasia. The Journal of Pediatrics. 188, 24-34 (2017).
- Huntsman, L. L., et al. Noninvasive Doppler determination of cardiac output in man. Clinical validation. Circulation. 67 (3), 593-602 (1983).
- Weisz, D. E., Poon, W. B., James, A., McNamara, P. J. Low cardiac output secondary to a malpositioned umbilical venous catheter: Value of targeted neonatal echocardiography. AJP Reports. 4 (1), 23-28 (2014).
- Quinones, M. A., et al. A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation. 64 (4), 744-753 (1981).
- Ruoss, J. L., et al. The evolution of neonatal hemodynamics and the role of ASE in cultivating growth within the field. ECHO. 11 (4), 16-19 (2022).
- Bensley, J. G., De Matteo, R., Harding, R., Black, M. J. The effects of preterm birth and its antecedents on the cardiovascular system. Acta Obstetricia et Gynecologica Scandinavica. 95 (6), 652-663 (2016).
- Sehgal, A., Mehta, S., Evans, N., McNamara, P. J. Cardiac sonography by the neonatologist: Clinical usefulness and educational perspective. Journal of Ultrasound in Medicine. 33 (8), 1401-1406 (2014).
- Zecca, E., et al. Left ventricle dimensions in preterm infants during the first month of life. European Journal of Pediatrics. 160 (4), 227-230 (2001).
- Jain, A., et al. Left ventricular function in healthy term neonates during the transitional period. The Journal of Pediatrics. 182, 197-203 (2017).
- Nagasawa, H. Novel regression equations of left ventricular dimensions in infants less than 1 year of age and premature neonates obtained from echocardiographic examination. Cardiology in the Young. 20 (5), 526-531 (2010).
- Skelton, R., Gill, A. B., Parsons, J. M. Reference ranges for cardiac dimensions and blood flow velocity in preterm infants. Heart. 80 (3), 281-285 (1998).
- Kampmann, C., et al. Normal values of M mode echocardiographic measurements of more than 2000 healthy infants and children in central Europe. Heart. 83 (6), 667-672 (2000).
- Overbeek, L. I. H., et al. New reference values for echocardiographic dimensions of healthy Dutch children. European Journal of Echocardiography. 7 (2), 113-121 (2006).
- Riggs, T. W., Rodriguez, R., Snider, A. R., Batton, D. Doppler echocardiographic evaluation of right and left ventricular diastolic function in normal neonates. Journal of the American College of Cardiology. 13 (3), 700-705 (1989).
- Schmitz, L., Koch, H., Bein, G., Brockmeier, K. Left ventricular diastolic function in infants, children, and adolescents. Reference values and analysis of morphologic and physiologic determinants of echocardiographic Doppler flow signals during growth and maturation. Journal of the American College of Cardiology. 32 (5), 1441-1448 (1998).
- Schmitz, L., et al. Doppler-derived parameters of diastolic left ventricular function in preterm infants with a birth weight <1500 g: Reference values and differences to term infants. Early Human Development. 76 (2), 101-114 (2004).
- Ito, T., Harada, K., Takada, G. Changes in pulmonary venous flow patterns in patients with ventricular septal defect. Pediatric Cardiology. 23 (5), 491-495 (2002).
- Mori, K., et al. Pulsed wave Doppler tissue echocardiography assessment of the long axis function of the right and left ventricles during the early neonatal period. Heart. 90 (2), 175-180 (2004).
- Galiè, N., et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. European Heart Journal. 25 (24), 2243-2278 (2004).
- Shiraishi, H., Yanagisawa, M. Pulsed Doppler echocardiographic evaluation of neonatal circulatory changes. Heart. 57 (2), 161-167 (1987).
- Howard, L. S., et al. Echocardiographic assessment of pulmonary hypertension: Standard operating procedure. European Respiratory Review. 21 (125), 239-248 (2012).
- . Neonatologist Performed Echocardiography. Teaching Manual Available from: https://neonatalhemodynamics.com/PDF/NPE%20Teaching%20Manual%20El-Khuffash%20-%202019.pdf (2019)
- . Neonatal Hemodynamics Research Center Available from: https://neonatalhemodynamics.com/ (2022)
- . Targeted neonatal echocardiography application Available from: https://itunes.apple.com/i.e./app/tnecho (2022)
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaPrzeglądaj więcej artyków
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone