Method Article
A Modified Bilateral Scrotal Flap for Penile Skin Defect Repair
In This Article
Summary
This study presents an application of the modified bilateral scrotal flap for the reconstruction of penile skin shortages and scar contractures.
Abstract
Skin shortages and scar contractures are common complications following penile trauma and tumor surgery, resulting in significant pain and erectile dysfunction. Currently, skin grafts and scrotal flaps are widely used to reconstruct skin shortages. However, various limitations still exist; for instance, the skin graft may cause severe scarring in patients, and the traditional scrotal flap usually requires a two-stage procedure due to the large skin defect.
To treat the shortage of foreskin, a modified bilateral scrotal pedicled flap is used. In this procedure, flaps located on each side of the midline of the scrotum, which was pedicled from the anterior scrotal artery, are harvested. Subsequently, these bilateral scrotal flaps, like a butterfly, can successfully cover the foreskin defect. In this study, seven patients underwent this procedure, and satisfactory outcomes were obtained. Only two patients developed necrosis in some small areas of the flaps, which were recovered after wound care. Postoperative penile length significantly increased compared to the preoperative status in both flaccid and erectile states. We believe that modified bilateral scrotal flaps are a simple and effective solution to penile skin shortages and scar contractures.
Introduction
Penile skin shortages often occur as a consequence of infections, trauma, burning, and surgical excision, owing to benign or malignant penile skin diseases1,2. Reconstructive surgery is a major treatment option for this disease with the ultimate goal of preserving cosmetic appearance as well as normal function by providing redundant skin envelopes to preserve the physiological girth and length expansion during erection and sexual intercourse2,3. For most surgeons, however, reconstructive surgery remains a challenge.
Currently, various techniques can be used to treat penile skin defects, such as split-thickness skin grafting (STSG), scrotal flaps, and/or pedicle flaps2,3,4,5,6,7. All these techniques have reported satisfactory outcomes with different advantages. For most patients with genital skin loss, STSG is a viable treatment that provides a fast-resurfacing solution with enough skin8. However, the contraction and poor expansive ability of survival grafts sometimes lead to poor postoperative satisfaction. Accordingly, flaps are a better choice because they can provide reliable circulation, sufficient size, good flexibility, and subcutaneous tissues for the penile shaft9,10,11. Among the various flaps, the scrotal flap is a viable treatment option for patients whose scrotum is not damaged, because it is closer to the penis and easier to harvest. Moreover, the scrotal anterior flap has a dual blood supply system, which means that it contains a good vascular supply and has a low incidence of necrosis12,13. However, conventional surgery using the scrotal flap is a two-stage procedure in which the nude penile shaft is buried beneath the flap in the first stage, and reconstruction is performed in the second stage14. It is a secure but time-exhaustive procedure, and patients suffer much more physical and psychological damage in this multi-stage surgery.
To resolve these problems, we modified the two-stage scrotal flap technique into a single-stage procedure using a bilateral scrotal skin pedicle flap for penile skin reconstruction. Here, we describe this technique, which makes the treatment simpler and more efficient.
Protocol
The study was approved by the local Medical Ethics Committee of Shanghai Ninth People's Hospital in China. All the studies were conducted in accordance with the Declaration of Helsinki of the World Medical Association, and written consent was obtained from all patients.
1. Preparations for the surgery
- Evaluate patients through a detailed history assessment and a physical examination, comprising of pelvic magnetic resonance imaging, scrotal size measurement, and assessment of the severity of the scar (Figure 1A).
- Ensure that the preoperative anesthesia risk assessment of the patient has been performed by an anesthesiologist.
- Ask the patient to shower and wash the skin of the surgical region daily.
- On the day of the operation, administer intravenously antibiotics containing cefuroxime sodium (1.5 g) in 100 mL of 0.9% sodium chloride solution, 30 min preoperatively.
- After general anesthesia, place the patient in the lithotomic position for optimal exposure of the surgical area.
- For adequate disinfection, continuously disinfect the skin of the surgical area with an iodophor and coverwith surgical drapes.
2. Performing the operation
- Remove the scar tissue and skin around the penis until it is released (Figure 1B). Perform coagulation of bleeding vessels with monopolar electrocoagulation.
- Place a catheter through the urethra for urine drainage and urethral protection intraoperatively.
- Measure the size of the penile skin defect when the penis is completely stretched (Figure 1C). The flaccid stretched penile status is regarded as approximate to the length of the erect penis15.
- Design the bilateral scrotal skin flap according to the length and circumference of the foreskin defect. Make an incision longitudinally along the midscrotal line with a length just half of the circumference of the penis.
- Subsequently, divide the scrotal skin into two parts (Figure 1D). Make a transverse incision across the scrotum to form two long flaps on either side of the midscrotal line with a length equal to that of the stretched penis (Figure 1E).
- Harvest the flaps along the tunica vaginalis by blunt dissection, and carefully preserve as much of the superficial dartos of the flap as possible.
- Rotate each flap approximately 90°, with the base of the flap as the center to cover the corpus cavernosum (Figure 1F). Ensure that the base of the flaps is wider, and the flap is trapezoidal.
- Close the wound using drainage at the bottom of the scrotum. Fix the drainage at the scrotal skin using a silk 2-0 suture.
- Layer the subcutaneous tissue and scrotal skin off with 3-0 absorbable polyglactin sutures (Figure 1G,H). Fix the penis upward with an elastic bandage at an angle of approximately 45° horizontally.
3. Postoperative care
- Postoperatively, administer an intravenous antibiotic containing 1.5 g of cefuroxime sodium in 100 mL of 0.9% sodium chloride solution every 12 h for 3 days.
- Remove the drainage tube and change the dressing on postoperative day (POD) 3. After two dressing changes on POD 3 and 5, discharge the patient on POD 5.
- Ask the patients to perform postoperative disinfection with iodophor by themselves every 2 days to prevent postoperative infection of the incision.
4. Follow-up study
- Ask the patients to attend follow-up examinations on POD 7, 14, and 30. During the follow-ups, assess postoperative outcomes, including postoperative IIEF-5 score and any complications that might have developed.
Results
Using the protocol described above, seven patients underwent the modified bilateral scrotal pedicled flap surgery. The median age, duration of disease, and length of the flap were 32 years (23-53 years), 7 months (3-12 months), and 12 cm (10-13 cm), respectively. Of these seven patients, only two developed necrosis in some small areas of the flaps but recovered after wound care. The necrosis of flaps is mainly caused by bad preservation of the superficial dartos and vascular supply. The length of the flap is not a contributing factor to this. There was a statistically significant difference between the pre- and post-operative penile lengths in the flaccid state (t-test, p < 0.001). The erectile functions of the patients were well preserved, and the median postoperative IIEF-5 score was 23 (range: 5-25). Only one patient did not have sexual intercourse during the follow-up.
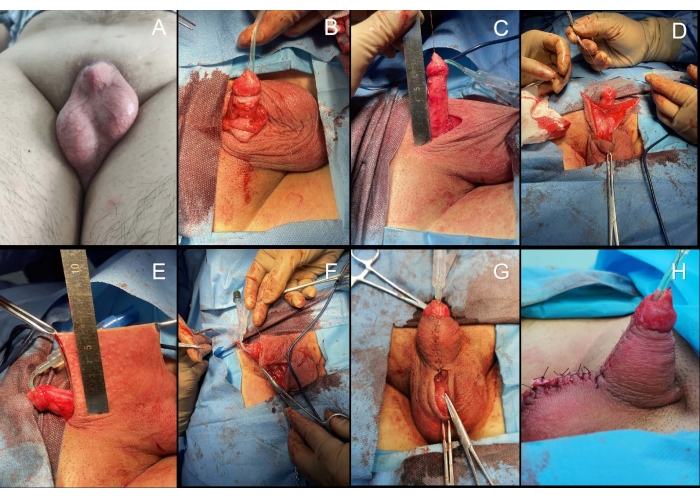
Figure 1: Bilateral scrotal flap approach.(A) The preoperative status showed a buried penis. (B) The penis is released from the scar, and lichen sclerosus is observed on the residual foreskin. (C) The size of the penile skin defect when the skin lesion was completely resected is measured. (D) An incision is made longitudinally along the midscrotal line, and the scrotal skin is subsequently divided into two parts. (E-F) The bilateral scrotal flaps on either side of the midscrotal line are formed, and each flap is rotated approximately 90°, with the base of the flap as the center to cover the corpus cavernosum. (G) The subcutaneous tissue and scrotal skin are layered off with 3-0 absorbable polyglactin sutures. (H) Postoperative status of the penis. Please click here to view a larger version of this figure.
| Patient No. | Age (years) | Duration of disease (months) | Etiology | Length of flap (cm) | Preoperative penile length in flaccid states (cm) | Postoperative penile length in flaccid states (cm) | Complication | Postoperative IIEF-5 Score |
| 1 | 23 | 7 | Trauma | 10 | 3.6 | 8.5 | None | 5 (No sexual intercouse) |
| 2 | 41 | 6 | Trauma | 12 | 3.3 | 9.2 | Necrosis of partial flap | 23 |
| 3 | 32 | 10 | Post-infectious | 12 | 4.1 | 8.2 | None | 25 |
| 4 | 28 | 3 | Trauma | 11 | 4.3 | 8.5 | None | 24 |
| 5 | 31 | 7 | Trauma | 12 | 3.2 | 8.6 | None | 25 |
| 6 | 53 | 6 | Post-infectious | 13 | 3.5 | 7.8 | Necrosis of distal flap | 23 |
| 7 | 42 | 12 | Trauma | 12 | 4.3 | 8.3 | None | 23 |
Table 1: The clinical characteristics and the outcomes of the patients.
Discussion
Extensive loss of penile skin is troublesome and harmful to individuals16. The goal of reconstruction is to achieve a good aesthetic appearance of the penis and restore the extensibility of the foreskin. In most situations, STSG is preferred to cover the defect3,5. However, postoperative scarring and edema of the survival grafts sometimes result in unsatisfactory feedback. There have been reports of multi-stage operations, including the embedding of the denuded penis in the scrotum and later lifting it from its bed surrounded by scrotal skin10; Goodwin and Thelen first described the implantation of the penis under scrotal skin in 195017. This penile skin reconstruction method is an old, simple, and reliable solution. However, multi-stage operations are time-consuming and may lead to secondary sexual dysfunction caused by psychological damage. Thus, one-stage surgery, with a less aggressive surgical strategy, may be preferable5.
We devised a simple and effective technique for penile skin reconstruction using a bilateral scrotal flap. This fasciocutaneous flap can avoid the main disadvantages of STSG, including graft contracture and donor site complications. The fasciocutaneous flap can also preserve adequate sensation and provide sufficient coverage for large defects18. After releasing the scar and measuring the penile skin defect, scrotal flap coverage of the same size was performed for reconstruction.
There are several advantages to the scrotal flap technique, which are as follows: First, the scrotal skin contains superficial dartos without a thick adipose layer, making it thin and flexible19. Second, the scrotal anterior flap has a dual blood supply system that is connected to one another12,13. Third, the scrotal flap contains sensory branches from the ilioinguinal nerves, which may improve intercourse satisfaction. Thus, the critical step of the protocol is good preservation of the superficial dartos and careful dissection of the avascular area. In addition, the flaps should be formed as trapezoids since some penises are conical. This shape also makes for a tension-free suture in the area between the penis and scrotum.
Reconstructing the foreskin is important in terms of function, aesthetics, and psychology. Compared with STSG, the modified bilateral scrotal flap provides better skin laxity for erection, similar skin color, and durability during sexual intercourse20. Inboth the flaccid and erectile status, the shape of the penis is more natural, and its postoperative length is significantly longer18. Meanwhile, less discomfort or pain was observed in the penile erect status, as the scar was released thoroughly. However, this procedure is not feasible for patients with insufficient scrotal skin. In addition, this procedure carries a higher risk of failure than staged and STSG procedures.
In conclusion, the bilateral scrotal flap is suitable for the repair of penile skin defects and provides substantial benefits to patients, owing to satisfactory cosmetic and sexual function results. The surgical procedure includes flap design according to the defect, skin flap transfer to the penis, bilateral flap elevation, and wound closure. This simple, safe, effective, and time-saving procedure is performed in a single stage to avoid economic and social problems, and is recommended for further clinical practice.
Disclosures
There are no conflicts of interest to declare.
Acknowledgements
The authors thank the patient who kindly contributed and shared his disease experience for this article. The authors would like to acknowledge the support of the Project of biobank from Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine (YBKB202119), Medical Research Foundation of Shanghai Science and Technology Commission (20Y11904300), Cross-disciplinary Research Fund of Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine (JYJC201912) and Clinical Research Foundation of Shanghai Municipal Health Commission (202040437).
Materials
| Name | Company | Catalog Number | Comments |
| 10Fr Suction drain (1) | Guanzhou Wellead Medical Co. | ||
| 18Fr silicone urethral catheter (1) | Guanzhou Wellead Medical Co. | ||
| 3-layered compress 30 cm x 45 cm (10) | According to surgeon's preference | 175260 | |
| Allis forceps 16cm | B.Braun | EA092R | |
| Allis forceps 20cm | B.Braun | EA095R | |
| Bard-Parker scalpel number 3 (1) | Jinzhong Medical Instruments | ||
| Bard-Parker scalpel number 4 (1) | Jinzhong Medical Instruments | ||
| Debakey forceps 16 cm (6) | Strong Medical Instruments | ||
| Debakey forceps 20 cm (2) | Strong Medical Instruments | ||
| Debakey needle driver 18 cm (1) | B.Braun Medical Instruments | BM035R | |
| Electrocauter blade 15 cm (1) | Hutong Medical Instruments | CO 150i | |
| Halsted-Mosquito (8) | Jinzhong Medical Instruments | ||
| Jones scissor 18 cm (1) | Strong Medical Instruments | ||
| Mayo-Hegar needle driver 20 cm (1) | B.Braun Medical Instruments | BM022R | |
| Mayo-Stille scissor 17 cm (1) | Strong Medical Instruments | ||
| Monopolar electrocauter Valleylab (1) | Medtronic | E2100 | |
| Nylexogrip 10cm x 4.5m (1) | Urgo | 1641486 | |
| Scalpel blade number 15 (1) | Jinzhong Medical Instruments | ||
| Scalpel blade number 24 (1) | Jinzhong Medical Instruments | ||
| Sterile drapes (4) | Medline | ||
| Sterile gloves (3 pairs) | medicom-china | ||
| Sterile gown (3) | According to surgeon's preference | NA | |
| Surgical compress 10 cm x 10 cm (10) | According to surgeon's preference | 232088 | |
| Surgical forceps 14 cm (2) | Jinzhong Medical Instruments | ||
| Urgostrapping 8 cm x 2.5 m (1) | Urgo | 696037 | |
| Vacuum flask 250 mL (1) | Guanzhou Wellead Medical Co. | ||
| Vicryl 3-0 wire (6) | Ethicon | VCP316H | |
| Vicryl 5-0 wire (2) | Ethicon | VCP433H | |
| Vicryl Rapide 3-0 wire (2) | Ethicon | VF2260 |
References
- Garaffa, G., Raheem, A. A., Ralph, D. J. An update on penile reconstruction. Asian Journal of Andrology. 13 (3), 391-394 (2011).
- Guo, L., et al. Utilities of scrotal flap for reconstruction of penile skin defects after severe burn injury. International of Urology and Nephrology. 49 (9), 1593-1603 (2017).
- Ziylan, O., et al. A practical approach for the correction of iatrogenic penile skin loss in children: Scrotal embedding technique. Turkish Journal of Urology. 41 (4), 235-238 (2015).
- Chertin, B., et al. Fenestrated sheet split-thickness skin grafting for reconstruction of penile skin loss in pediatric population. Journal of Pediatric Surgery. 51 (8), 1362-1365 (2016).
- Black, P. C., Friedrich, J. B., Engrav, L. H., Wessells, H. Meshed unexpanded split-thickness skin grafting for reconstruction of penile skin loss. The Journal of Urology. 172 (3), 976-979 (2004).
- Zucchi, A., et al. Iatrogenic trapped penis in adults: new, simple 2-stage repair. The Journal of Urology. 183 (3), 1060-1064 (2010).
- Vaca, E. E., Mundinger, G. S., Zelken, J. A., Erdag, G., Manahan, M. A. Surgical excision of multiple penile syringomas with scrotal flap reconstruction. Eplasty. 14, 21 (2014).
- Maguiña, P., Palmieri, T. L., Greenhalgh, D. G. Split thickness skin grafting for recreation of the scrotum following Fournier's gangrene. Burns. 29 (8), 857-862 (2003).
- Fakin, R., et al. Reconstruction of penile shaft defects following silicone injection by bipedicled anterior scrotal flap. The Journal of Urology. 197 (4), 1166-1170 (2017).
- Ratner, D. Skin grafting. From here to there. Dermatologic Clinics. 16 (1), 75-90 (1998).
- Muranyi, M., Varga, D., Kiss, Z., Flasko, T. A new modified bipedicle scrotal skin flap technique for the reconstruction of penile skin in patients with paraffin-induced sclerosing lipogranuloma of the penis. The Journal of Urology. 208 (1), 171-178 (2022).
- Zhao, Y. Q., Zhang, J., Yu, M. S., Long, D. C. Functional restoration of penis with partial defect by scrotal skin flap. The Journal of Urology. 182 (5), 2358-2361 (2009).
- Mendez-Fernandez, M. A., Hollan, C., Frank, D. H., Fisher, J. C. The scrotal myocutaneous flap. Plastic and Reconstructive Surgery. 78 (5), 676-678 (1986).
- Yachia, D. Penile injuries. Text Atlas of Penile Surgery. 12, 136-138 (2007).
- Veale, D., Miles, S., Bramley, S., Muir, G., Hodsoll, J. Am I normal? A systematic review and construction of nomograms for flaccid and erect penis length and circumference in up to 15,521 men. BJU International. 115 (6), 978-986 (2015).
- Paraskevas, K. I., Anagnostou, D., Bouris, C. An extensive traumatic degloving lesion of the penis. A case report and review of the literature. International of Urology and Nephrology. 35 (4), 523-527 (2003).
- Goodwin, W. E., Thelen, H. M. Plastic reconstruction of penile skin; implantation of the penis into the scrotum. Journal of the American Medical Association. 144 (5), 384 (1950).
- Yao, H., et al. Reconstruction of major scrotal defects by anterolateral thigh flap. Cell Biochemistry and Biophysics. 70 (2), 1331-1335 (2014).
- Giraldo, F., Mora, M. J., Solano, A., Gonzalez, C., Smith-Fernandez, V. Male perineogenital anatomy and clinical applications in genital reconstructions and male-to-female sex reassignment surgery. Plastic and Reconstructive Surgery. 109 (4), 1301-1310 (2002).
- Ching, W. C., Liao, H. T., Ulusal, B. G., Chen, C. T., Lin, C. H. Salvage of a complicated penis replantation using bipedicled scrotal flap following a prolonged ischaemia time. Journal of Plastic, Reconstructive & Aesthetic Surgery. 63 (8), 639-643 (2010).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved