Method Article
A Technique for Subcutaneous Abdominal Adipose Tissue Biopsy via a Non-diathermy Method
* These authors contributed equally
In This Article
Summary
We standardized an abdominal adipose tissue biopsy using a non-diathermy method performed under local anesthesia. Three cases of excessive post-operation bleeding out of 115 operations (2.61%) occurred.We conclude that an abdominal adipose tissue surgical biopsy using a non-diathermy method can be safely applied to healthy men.
Abstract
Adipose tissue biopsies offer tissue samples that, upon analysis, may provide insightful overviews of mechanisms relating to metabolism and disease. To obtain subcutaneous adipose tissue biopsies in the abdominal area, researchers and physicians use either a surgical or a needle-based technique. However, surgical subcutaneous fat biopsies can offer tissue samples that may provide a more comprehensive overview of the complexities of biological indices in white adipose tissue. Usually, a surgical adipose tissue biopsy includes a diathermy treatment for cauterizing blood vessels to prevent excessive bleeding. Nevertheless, side effects, such as flash fires and skin lesions in the tissue, have been reported after diathermy. Therefore, we aimed to standardize a surgical abdominal adipose tissue biopsy performed under local anesthesia using a non-diathermy method. We conducted 115 subcutaneous adipose tissue biopsies in healthy men using a non-diathermy abdominal surgical biopsy method. Our results showed three cases of excessive post-operation bleeding out of 115 operations (2.61%).In conclusion, our standardized subcutaneous abdominal adipose tissue surgical biopsy using a non-diathermy method can be safely applied to healthy men at the bedside, with minimal side effects.
Introduction
Adipose tissue biopsies offer tissue samples that, upon analysis, may provide an insightful overview of mechanisms relating to metabolism and disease. For instance, they are used for breast cancer tumor identification1, fatty acid composition examination2, and research on important metabolic and hormonal disease pathways3. To obtain subcutaneous adipose tissue biopsies in the abdominal area, researchers and physicians use either a surgical or a needle-based technique. However, surgical subcutaneous fat biopsies can offer tissue samples that may provide a more comprehensive overview of complex biological mechanisms [e.g., messenger ribonucleic acid (mRNA) expression, histological analysis, etc.]4. They have previously been used in healthy adults4 and can be safely performed at the bedside5.
The needle-based biopsy technique requires intense liposuction that may destroy the integrity of the tissue, and it usually retrieves a small amount of tissue (100-500 mg)6. These tissue samples may not be appropriate for complex research studies. Furthermore, compared to the needle-based technique, surgical subcutaneous fat biopsies can offer tissue samples that may draw a more complete picture of several inflammatory indices (e.g., B- and T-cell signaling); cytoskeleton regulation; cellular pathways; metabolic pathways of lipids, carbohydrates and amino acids; and oxidative phosphorylation pathways4. Also, the needle-based technique includes a higher risk for blood cell contamination than the surgical one4, while providing little information about the fibrotic regions of the tissue4,7,8.
Usually, a surgical adipose tissue biopsy includes a diathermy treatment for cauterizing blood vessels to prevent excessive bleeding9. A diathermy is also used to burn and destroy tissues affected by neoplasms and warts or tissues that are infected by disease9. This technique is particularly applicable in neurosurgery and eye surgery9.
The excessive use of diathermy may lead to the formation of necrotic tissue, causing infections and delaying the healing process10. Indeed, side effects such as flash fires and skin lesions in the tissue have been reported following diathermy9. Additionally, concerns have been raised about the toxicity of surgical smoke released by diathermy into the surgery environment, which may be inhaled by the participant/patient and the operating staff9. Indeed, the use of diathermy may cause air toxicity in the operating room equal to that produced by smoking six cigarettes11 and, although operating rooms typically have good ventilation systems, the contamination can last for at least 20 min12. However, in patients undertaking a tonsillectomy surgery, the diathermy method has shown less, but non-significant, post-operative pain13 and bleeding14 than the classic ligation hemostasis method. Overall, evidence regarding differences in the post-operative pain and bleeding rates after adipose tissue biopsies in healthy individuals barely exists. Given the lack of evidence and the side effects of diathermy, standardization of a non-diathermy method for adipose tissue biopsy is warranted. Accordingly, the aim of this study was to standardize a surgical technique for subcutaneous abdominal adipose tissue biopsy, performed under local anesthesia using a non-diathermy method in healthy men. Moreover, we outline the procedures for tissue collection to determine mRNA expression and protein concentration and to perform histological analyses.
Protocol
The study conformed to the standards set by the Declaration of Helsinki and was approved by the University of Thessaly, Department of Exercise Science, Βiοethics Committee.
1. Preparation of the Surgery Equipment and Consumables
- Position a disinfected surgical field on a 4-wheel surgical Mayo stand.
- Position the following consumables and surgical equipment on a 4-wheel surgical Mayo stand:
One pair of straight operating scissors (15 cm)
One scalpel (No. 11)
One scalpel handle
One pair of curved scissors (14 cm)
One mosquito forceps
One pair of Kocher tweezers
One surgical tweezer
Povidone-iodine (on a sterile gauze)
One suture (4.0)
One pair of straight scissors (11 cm)
One needle holder (15 cm)
Five sterile gauzes
One adhesive sterile gauze
One 10-mL syringe with a disinfected needle
10mL of 2% xylocaine (no adrenaline)
One pair of disinfected surgical gloves - Position the following materials on a separate bench:
Two microcentrifuge tubes
One tube containing 5 mL of 10% formalin
One small container containing 50-100 mL of liquid nitrogen at -190 °C.
2. Preparation of the Participants
- Have participants follow an 8 h fast15 prior to the biopsy procedure.
- Have participants refrain from physical exercise, excessive stressors, alcohol, and active and passive smoking 72 h prior the biopsy16,17.
3. Performing the Subcutaneous Adipose Tissue Biopsy
- Position the participant on the surgical bed in a supine position.
- Disinfect the region of the incision using povidone-iodine.
- Inject 10 mL of 2% xylocaine (no adrenaline) slowly and steadily18 into the selected region to serve as local anesthesia.
- Position a sterile surgical field over the area to cover the body of the participant, excluding the region of the incision.
- At least 3-5 min afterwards, apply pressure with a pair of tweezers to the area of local anesthesia and ask the participant if he feels any pain19 to ensure that local anesthesia has been achieved.
- Attach the No. 11 scalpel to the scalpel handle.
- Create an incision of 2-2.5 cm in length, 3-5 cm to the left or right of the navel.
- Remove the subcutaneous tissue with a pair of straight 15 cm operating scissors.
- Once the adipose tissue is revealed, capture it with a pair of tweezers and a pair of curved 14 cm scissors.
- Cut and remove approximately 1 g of adipose tissue.
- Following tissue removal, position sterile gauzes over the incision to achieve hemostasis.
- When hemostasis is confirmed, capture the 4.0 suture with a 14 cm needle and the skin with a pair of surgical tweezers until the subcutaneous tissue is visible.
- Insert the suture-needle into the skin, moving towards the subcutaneous tissue while the skin and subcutaneous are closely aligned.
- With the suture-needle, follow a continuous zig-zag technique into the subcutaneous tissue until driven externally off the skin. Continue until the skin incision is closed.
- Externally tie the suture.
- Clean the area of incision with saline and cover it with an adhesive sterile gauze.
4. Deposition of the Tissue
- Separate the collected adipose tissue into three pieces: 150, 350, and 500 mg.
- Position the 150 and 350 mg pieces of sample tissue in microcentrifuge tubes.
- Immerse the two microcentrifuge tubes in the small container with the liquid nitrogen at -190 °C until final deposition in a freezer at -80 °C.
NOTE: In advance, use a sterile needle to puncture a small hole in the microcentrifuge tubes to avoid cup failure during the immersion of the microcentrifuge tubes in the liquid nitrogen at -190 °C. - Immerse the 500 mg piece of sample tissue-to be used for histological analysis-in a tube containing 5 mL of 10% formalin.
NOTE: Use the mosquito forceps only in cases of excessive bleeding during the surgery. In such cases, capture the vessel with the mosquito forceps to ligate and close until hemostasis is achieved.
Results
The characteristics of the participants are provided in Table 1. The stitches in the area of the incision fell off within the next 8-12 days. We completed a total of 115 subcutaneous adipose tissue biopsies using the non-diathermy abdominal surgical biopsy method in healthy adult men (age: 35.2 ± 6.9 years; body mass index: 27.3 ± 4.4; and body fat percentage: 27.0 ± 9.0%). Post-biopsy excessive bleeding was observed in three cases (prevalence: 2.61%) two days after the surgery. The three individuals who experienced excessive bleeding were older than their counterparts who experienced no side effects [t(113)= -2.115, p = 0.037], and no other differences (i.e., body mass index and body fat percentage) were observed (p >0.05) between the two groups. Finally, three months after each operation, none of our participants reported any side effects (including skin wounds).
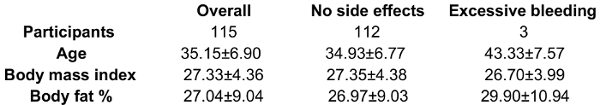
Table 1: Characteristics of the participants.
Discussion
The aim of this study was to standardize a surgical technique for subcutaneous abdominal adipose tissue biopsy, performed under local anesthesia with a non-diathermy method in healthy men. Diathermy is commonly used in the operating room; however, possible side effects (i.e., flash fires and environmental toxicity)9 and delays in healing10 may occur. These unwanted effects of diathermy can generate health risks for both the operating staff and the patients/participants. Therefore, a surgical non-diathermy method for subcutaneous adipose tissue biopsy is warranted.
We observed excessive bleeding in three of our participants two days after the surgery. These three individuals reported pain in the area of the incision. To treat these cases, the area of the skin incision was reopened, any excess blood was removed, and the area was cleaned with saline and closed using the same technique described above. No complications were reported after that, and normal healing was observed in the subsequent days. Our results have shown minimal side effects after the non-diathermy method: three cases of excessive post-operation bleeding out of 115 operations (2.61%). Previous evidence from needle-based adipose tissue biopsies showed minor bleeding in one out of 10 participants 12 h after the surgery15, while no significant bleeding occurred in healthy obese individuals after a side-cutting adipose tissue biopsy needle technique6. Based on our results, we anticipate that a non-diathermy surgical adipose tissue biopsy method may eliminate the risk for skin lesion, flash fires, and toxicity released in the operating environment, which are caused by diathermy during surgical adipose tissue biopsy.
Previous reports have indicated that aging is positively associated with abnormalities in hemostasis20. Interestingly, the three individuals who experienced excessive bleeding in the current study were significantly older (by eight years, on average) than those who did not experience any side effects. Therefore, it may be noted that older individuals have a higher risk for side effects when the non-diathermy surgical adipose tissue biopsy method is applied. However, we believe that the prevalence of such side effects is too low (i.e., 2.61%) to cause any significant concerns. It should be noted that our participants filled in advance a medical history questionnaire to determine their health status. No previous chronic disease conditions were reported by the participants, including the three participants who showed excessive post-operation bleeding. Similarly, no previous chronic medication treatment was reported by both the participants who showed and those who did not show any excessive bleeding. Therefore, the post-operation excessive bleeding we observed in the current study cannot be attributed to previous chronic disease conditions and/or previous chronic medication treatment. In this light, the prevalence of this side effect may be different if the technique is applied to clinical populations.
A critical step during the proposed surgical adipose tissue biopsy is to ensure local anesthesia before the incision, which prevents any pain and discomfort in the participant. Furthermore, a pre-screening of allergic history to the anesthetic must be done to prevent allergic complications during the anesthetic injection. Also, it is crucial to ensure hemostasis before the incision is closed to prevent post-operation bleeding, while it is important to keep in contact with the participants for several days after the procedure is performed until complete healing is achieved to discover any potential abnormalities and to prevent infection and/or cases of post-operation bleeding.
Limitations of the proposed biopsy technique include the discomfort that area of the incision may cause to the participants, particularly relating to their ability to comfortably sit down and take a shower/bath, until complete healing is achieved. The participants should be instructed to avoid washing the area of the incision to prevent infection, as well as to replace the adhesive sterile gauze over the incision area every day until complete healing is achieved. This daily procedure may cause discomfort. Finally, it is important to note that our purpose was to introduce and standardize a new technique. In this light, we did not use a control group undertaking needle-based subcutaneous fat biopsies in order to quantify the differences between this technique and the newly-introduced non-diathermy method.
As previously suggested4,7,8, the proposed surgical biopsy technique may offer tissue samples with higher integrity than the needle-based technique. Indeed, using this technique, we were able to perform mRNA and protein analyses on the obtained tissue and, in addition, to form paraffin cubes for use in histological analyses. Also, we suggest avoiding diathermy in surgical subcutaneous adipose tissue biopsies, given that hemostasis and normal healing can be achieved with our technique.
In conclusion, our standardized subcutaneous abdominal adipose tissue surgical biopsy using a non-diathermy method can be safely performed in healthy men at the bedside, with minimal side effects.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgements
This work received funding from the European Union's Horizon 2020 (grant agreement no. 645710) and 7th Framework (grant agreements no. 612547 and 319010) Programmes. The authors wish to thank Dr. Fotini Sourli-Chasioti for the assistance with the biopsy procedure. The authors also thank Mr. Yiorgos Paterakis for his valuable help in the preparation of the video.
Materials
| Name | Company | Catalog Number | Comments |
| Disinfected surgical field | Hartmann | 23516-00 | |
| Stainless Steel Instrument Stands (surgical Mayo) | Medical Device Depot Inc. | 32000 | |
| Operating Scissors straight 15 cm | Karl Storz | 791903 | |
| Scalpel No 11 | Swann-Morton | 203 | Bipolar, catalog number 429011 |
| Scarpel handle No 3 | Karl Storz | 488090 | |
| Scissors curved 14 cm | Karl Storz | 511514, 752918 | |
| Mosquito forceps | Karl Storz | 535012 | |
| Tweezers Kocher | Karl Storz | 530416 | Bipolar, catalog number 830316 |
| Surgical tweezers | Karl Storz | 793216 | Bipolar, catalog number 831016 |
| Povidone-iodine | Various | Not applicable | |
| Suture 4.0 Vicryl | Johnsons | V4970H | |
| Scissors straight 11 cm | Karl Storz | 512511 DS | |
| Needle holder 15 cm | Karl Storz | 515515 | Bipolar, catalog number 213015 |
| Sterile gauzes | Hartmann | 3021 | |
| Αdhesive sterile gauze | Digas medical equipment | 2889 | |
| 10 mL syringe with disinfected needle | Alpha medical solutions | 10310-55-0010 | |
| 2%-xylocaine (no adrenaline) | Various | Not applicable | |
| Sterile surgical gloves | Sempermed | 10001 | |
| Eppendorf tubes | Kartell | 16283 | |
| 10% formalin | Alpha medical solutions | 11016-30-2909 | |
| Tubes 120 mL | Digas medical equipment | 9025 | |
| Liquid nitrogen at -190°C | Revival | Not applicable |
References
- Bruening, W., et al. Systematic review: comparative effectiveness of core-needle and open surgical biopsy to diagnose breast lesions. Ann Intern Med. 152, 238-246 (2010).
- Beynen, A. C., Katan, M. B. Rapid sampling and long-term storage of subcutaneous adipose-tissue biopsies for determination of fatty acid composition. Am J Clin Nutr. 42, 317-322 (1985).
- Wang, Y., et al. Muscle and adipose tissue biopsy in older adults with type 2 diabetes . J Diabetes Mellitus. 1, 27-35 (2011).
- Mutch, D. M., et al. Needle and surgical biopsy techniques differentially affect adipose tissue gene expression profiles. Am J Clin Nutr. 89, 51-57 (2009).
- Ikeda, S., Sekijima, Y., Tojo, K., Koyama, J. Diagnostic value of abdominal wall fat pad biopsy in senile systemic amyloidosis. Amyloid. 18, 211-215 (2011).
- Alderete, T. L., et al. A novel biopsy method to increase yield of subcutaneous abdominal adipose tissue. Int J Obes. 39, 183-186 (2015).
- Padoin, A. V., et al. A comparison of wedge and needle hepatic biopsy in open bariatric surgery. Obes Surg. 16, 178-182 (2006).
- Kral, J. G., et al. Effects of surgical treatment of the metabolic syndrome on liver fibrosis and cirrhosis. Surgery. 135, 48-58 (2004).
- Fitzgerald, J. E., Malik, M., Ahmed, I. A single-blind controlled study of electrocautery and ultrasonic scalpel smoke plumes in laparoscopic surgery. Surg Endosc. 26, 337-342 (2012).
- Memon, M. Surgical Diathermy. Br J Hosp Med. 52, (1994).
- Tomita, Y., et al. Mutagenecity of smoke condensates induced by CO-laser irradiation and electrocauterization. Mutat Res. 89, 145-149 (1989).
- Brandon, H., Young, L. Characterisation and removal of electrosurgical smoke. Surg Serv Manag. 3, 14-16 (1997).
- Attner, P., Hemlin, C., Soderman, A. C. Ligasure versus diathermy scissors tonsillectomy: A controlled randomized study. Acta Otolaryngol. 130, 1180-1184 (2010).
- Ecker, T., Carvalho, A. L., Choe, J. H., Walosek, G., Preuss, K. J. Hemostasis in thyroid surgery: harmonic scalpel versus other techniques--a meta-analysis. Otolaryngol Head Neck Surg. 143, 17-25 (2010).
- Campbell, K. L., et al. A pilot study of sampling subcutaneous adipose tissue to examine biomarkers of cancer risk. Cancer Prev Res. 2, 37-42 (2009).
- Jamurtas, A. Z., et al. The effects of a single bout of exercise on resting energy expenditure and respiratory exchange ratio. Eur J Appl Physiol. 92, 393-398 (2004).
- Adriaens, P. E. M., Schoffelen, F. M. P., Westerterp, K. R. Intra-individual variation of basal metabolic rate and the influence of daily habitual physical activity before testing. Brit J Nutri. 90, 419-423 (2003).
- Latham, J. L., Martin, S. N. Infiltrative anesthesia in office practice. Am Fam Phys. 89, 956-962 (2014).
- Jurevic, R., et al. Plasma levels of 2% lidocaine with 1:100,000 epinephrine with young children undergoing dental procedures. Anesth Prog. 45, 87-90 (1998).
- Kale, S. S., Yende, S. Effects of Aging on Inflammation and Hemostasis through the Continuum of Critical Illness. Aging Dis. 2, 501-511 (2011).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved