Method Article
The Transition to an Anterior-Based Muscle Sparing Approach Improves Early Postoperative Function but is Associated with a Learning Curve
W tym Artykule
Podsumowanie
The anterior-based muscle-sparing approach for total hip arthroplasty (THA) is associated with a learning curve. However, the improved clinical outcome in the early post-operative phase makes the consideration to transition worthwhile.
Streszczenie
Surgeons considering transitioning to an anterior-based approach for THA are concerned about the learning curve and the reported marginal clinical benefit. Accordingly, the first cohort of THAs, which were implanted by a single surgeon using the anterior-based muscle-sparing approach (ABMS), was analyzed. The goal of the study was to test 1) whether patient-reported outcomes improved and 2) whether the complication rate decreased with the number of THAs performed. A retrospective cohort study on the first 30 primary THA cases (27 patients) of one surgeon (January 2021-April 2021) using the ABMS approach was conducted. These 30 THAs were compared to 30 primary THA cases (30 patients) done immediately prior to the transition by the same surgeon (September 2020-December 2020) using the posterior approach (PA). The Oxford Hip Score (OHS), Hip Disability and Osteoarthritis Outcome Score (HOOS Junior), and Forgotten Joint Score (FJS) obtained 6 weeks and 6 months after surgery were compared. In addition, three consecutive groups based on equal numbers of THAs were compared for the incidence of complications and surgery time. At 6 weeks after THA, the OHS was 6 points higher after the ABMS approach (p = 0.0408), and the OHS was comparable at 6 months. The HOOS Junior and FJS were similar at 6 weeks and 6 months after surgery. In the first 10 THAs using the ABMS approach, one patient had a greater trochanter fracture, and one patient had an intraoperative proximal femur fracture. No further immediate interoperative or postoperative complications occurred. Surgery time significantly reduced with the number of THAs performed. Transitioning from the PA to the ABMS approach is associated with a learning curve, which is limited to the first 20 cases. The effect of improved clinical outcomes is apparent within the early postoperative period. After 6 months, THA patients do well regardless of the approach.
Wprowadzenie
In total hip arthroplasty (THA), the surgical approach serves to visualize the acetabulum and proximal femur and to prepare the acetabulum and proximal femur for safe and stable implantation of the prosthetic components1. An ideal surgical approach in THA provides adequate exposure while minimizing the risk of damage to the muscles, blood vessels, and nerves and the risk of postoperative instability.
The anterior-based muscle-sparing (ABMS) approach in THA utilizes the muscle interval popularized by Sir Reginald Watson-Jones in 19302. The ABMS approach avails itself of the intermuscular plane between the tensor fasciae latae (TFL) and the gluteus medius (GM) to gain access to the hip joint. The abductor muscles are preserved and not detached during this approach. As the ABMS approach is anterior to the GM and to the greater trochanter (GT), it is similar and shares the advantages of the direct anterior approach (DAA)-being muscle sparing. Even though the ABMS approach can be performed with the patient in a supine position, many surgeons prefer the lateral decubitus position based on its original description3.
The ABMS, like the DAA, has multiple operative and early postoperative benefits. The exposure of the acetabulum is excellent, which facilitates optimal positioning of the acetabular component. Functional recovery is faster in the early postoperative period due to there being less muscle damage and, consequently, lower dislocation rates4.
The reported disadvantages of the DAA are damage to the lateral femoral cutaneous nerve (LFCN), the need for a special operating table, wound healing problems, and more limited exposure to the femur5,6. By avoiding these disadvantages, the ABMS has since its introduction in 2004 routinely been utilized in European countries, and has recently attracted more attention in North America3. Motivated by 1) the concept of a muscle-sparing approach, which negates the necessity of post-operative precautions7, 2) the ability to perform the surgery in a lateral decubitus position, which allows stability evaluation maneuvers familiar to a surgeon performing THA through the posterior approach (PA), 3) avoiding intra-operative fluoroscopy8, 4) the increased anatomical distance to the LFCN in comparison to the DA, and 5) the further lateralized incision, which avoids wound-healing complications caused by overhanging soft-tissue, surgeons might decide to transition to the ABMS approach.
However, surgeons considering transitioning to the ABMS approach for THA are concerned about whether transitioning will ultimately improve patient outcomes and about the learning curve associated with the transition. Accordingly, the first cohort of 30 THAs, which were implanted by a single surgeon using the ABMS approach, was analyzed and compared to results gained from 30 THAs implanted by the same surgeon through the PA immediately before the transition. The present study tested 1) whether early patient-reported outcomes improved in the ABMS group in comparison to the PA group and 2) whether the surgical time and complication rate decreased with the number of THAs performed.
Protokół
An institutional review board approved this retrospective study (IRB 00060819) of deidentified prospectively collected data.The protocol followed the guidelines approved by the human institutional review board of Adventist Health Lodi Memorial. A written informed consent was obtained from the patients before the procedure.
NOTE: As a representative patient, the clinical course of a 78-year-old male with left hip pain is described. His symptoms included a 2 year history of left groin pain aggravated by activity, night pain not adequately relieved by anti-inflammatory medication, and limitations of daily activities. The Oxford Hip Score at his initial clinic visit was 22 points, and the Hip Disability and Osteoarthritis Outcome Score (HOOS Junior) was 53 points. X-rays revealed primary left hip osteoarthritis (Figure 1).

Figure 1: AP radiograph of the pelvis focused low on the symphysis. The left hip demonstrates typical characteristics of end-stage osteoarthritis. Please click here to view a larger version of this figure.
1. Diagnosis, assessment, and plan
- Left hip osteoarthritis
NOTE: Due to failed conservative treatment, the patient was offered left total hip replacement using the ABMS approach.- Use the AP-Pelvis x-ray with the 2.5 cm radiographic calibration marker for preoperative planning (Figure 2).
- Measure the distance from the trochanteric fossa to the planned femoral neck resection to restore equal leg length. Fit adequate component sizes to the bony contours to restore femoral offset.
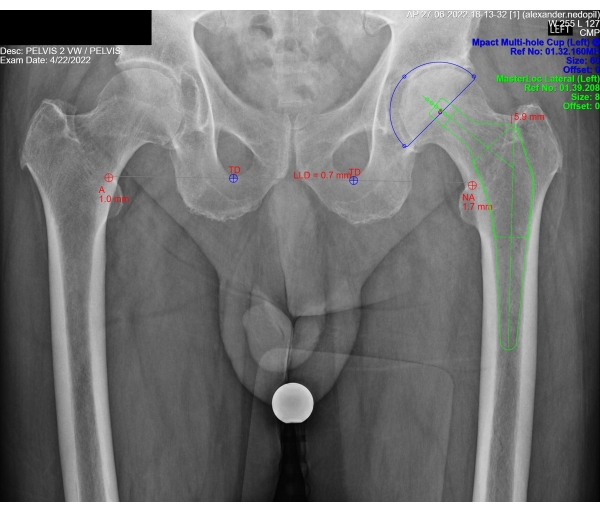
Figure 2: Planning THA. The planning of left THA begins with calibrating the radiograph to the metal ball of 2.5 cm diameter. Next, the preoperative leg length difference is measured (0.7 mm in this example). The appropriately sized acetabular component (blue) is positioned to restore the center of rotation. The appropriately sized femoral component with the ideal femoral offset (green) is positioned within the proximal femur to correct for any leg length difference. The distance between the trochanteric fossa and the planned femoral neck resection is measured (5.9 mm in this example). Please click here to view a larger version of this figure.
2. Surgical preparation
- Starting 5 days before surgery, ask the patient to perform daily skin cleansing using chlorhexidine washing solution. Before surgery, meet the patient in the preoperative holding area and mark the correct hip side with a skin marker.
- After the induction of general anesthesia with inhalation anesthetics and the confirmation of its success by the maintenance of stable vital signs, position the patient in a lateral decubitus position with the operated hip facing up. Perform sterile prepping and draping. Cover the exposed skin with iodine-impregnated adhesive.
- Wrap a sterile elastic bandage around assistant 1's waist to create a belt. The belt serves to hold a sterile mayo-stand cover, which is attached to the belt with two non-penetrating clamps (= kangaroo bag). The kangaroo bag maintains a sterile environment when the leg is dropped behind the patient.
- Position the surgeon in front of the patient and assistant 1 and assistant 2 behind the patient. Position assistant 1 more distal than assistant 2 to maneuver the leg during surgery.
- Mark the incision:
- Palpate and mark the proximal border or greater trochanter (GT) and the anterior border of the proximal femur. Palpate the anterior border of the gluteus medius (GM) fascia, which is tighter than the fascia overlying the tensor fasciae latae muscle.
- Starting 2 cm distal to the GT, make a line along the anterior border of the proximal femur and then slightly turn anterior along the anterior border of the GM fascia, stopping 6 cm proximal to the GT. The incision length is 8 cm.
3. Surgical procedure
- Instruct assistant 1 to abduct the hip. Incise the skin sharply with a #10-blade following the previously made skin mark. Cut down to the fascia with a knife and use a clean lap sponge to expose the fascia.
- The fascia is pierced by a bundle of vessels (= perforating vessels). Identify these perforating vessels as they pierce through the fascia. These vessels locate the interval between the GM and tensor fasciae latae (TFL). Distally open the fascia parallel to the orientation of the fascial fibers, and curve anteriorly at the mid-portion of the incision, staying posterior to the perforating vessels.
- Use finger palpation at the greater trochanter to dissect the muscle plane between the TFL anteriorly and the gluteus muscles posteriorly. Run a finger along the GM toward the GT. Then, let the finger drop anteriorly into the space between the GM and TFL. Once the finger is in the space, palpate the femoral neck and posterior portion of the femoral neck by elevating the gluteus medius and minimus posteriorly.
- While assistant 1 is holding the hip abducted, place a curved Hohmann retractor (Nr. 17) over the posterior neck outside the capsule to retract the glutei muscles. Then, place a straight Hohmann retractor (Nr. 7) over the anterior neck outside the capsule under the TFL and the reflected head of the rectus femoris tendon.
- Instruct assistant 1 to slightly externally rotate the hip and make an H-shaped capsulotomy using electrocautery with the bar of the H longitudinally along the femoral neck. Ensure that the distal line of the H is far lateral connecting the tip of the GT and medially around the neck to release the capsule and clean out the trochanteric fossa and intertrochanteric ridge.
- Using electrocautery, go through the entire capsule proximally toward the head and acetabular rim, which is felt as a step with an electrocautery tip. At the acetabular rim, turn the electrocautery 90° and release the capsule along the acetabular rim medially and laterally.
- Reposition the retractors underneath the capsule with the assistant holding the leg in abduction. While assistant 1 increases the external rotation and extension, make a subcapital femoral neck cut oblique from proximal to distal to facilitate the lift of the distal femur once the cut is complete.
- Hold the anterior retractor (Nr. 7 retractor) and, with a key elevator positioned at the osteotomy site, level the femoral neck into the surgical field while assistant 1 hyperextends the hip to "dislodge" the osteotomy. Instruct assistant 1 to place the leg in the kangaroo bag and externally rotate the hip so that the patella is pointing upward and the tibia is perpendicular to the floor.
- Reposition the Nr. 17 retractor over the GT and clean up the trochanteric fossa from the soft tissue using electrocautery.
- Instruct assistant 1 to adduct the hip so that the femoral neck is elevated more out of the wound. Identify the femoral neck cut at the planned level distal to the trochanteric fossa. Ideally, use a template to mark out the neck cut using electrocautery. Then, perform a neck cut using an oscillating saw.
- Cut the medial neck first and then proceed to the lateral neck, paying attention not to violate the GT. Remove the free bone piece of the femoral neck with an osteotome and grasper.
- Remove the Hohmann retractors, and instruct assistant 1 to place the leg out of the bag in a neutral position on the mayo stand to allow hip abduction and slight flexion.
- Place Nr. 15 or Nr. 17 retractors over the posterior acetabulum. The Nr. 15 retractor is wider than the Nr. 17 retractor but with comparable shape and curvature. Then, place the Nr. 7 retractor over the anterior acetabulum. Push through the capsule with the spike.
- Remove the femoral head with the Hohmann retractor and grasper. Push on the inferior part of the head to dislodge it superiorly. Then, use a grasper to remove the head. Remove the labrum using a long knife, and incise the inferior capsule if it is in the hemisphere of the acetabulum.
- Ream the acetabulum to an appropriate size, starting 1 mm smaller than the planned cup diameter. Then, insert the final acetabular component in 40° abduction and 10°-15° anteversion. Insert the final polyethylene liner by manually placing it within the acetabular component and then impacting the liner in the acetabular component to engage the locking mechanism.
- While assistant 1 places the leg in the kangaroo bag and externally rotates the hip to 90°, place a two-prong retractor under the postero-medial aspect of the femoral neck and the Nr. 17 retractor over the GT. Then, instruct assistant 1 to extend and adduct the hip.
- If needed, perform release along the anterior portion of the GT to deliver the femur out of the wound. Then, open the proximal femur with a box cutter and canal finder.
- Broach to an appropriate size and length and place the final stem with templated offset.
- Perform a trial reduction with a trial head. To reduce the hip, instruct assistant 1 to apply slight traction and internally rotate the hip while the surgeon uses a head-pusher to guide the ball into the socket. Check the hip for anterior and posterior stability. Place the Nr. 17 retractor over the posterior acetabulum to visualize the hip. Perform a shuck test in longitudinal and lateral traction.
- To dislocate the hip, place a bone hook around the neck, and instruct assistant 1 to apply traction and external rotation. Remove the trial head. Irrigate the cup, insert the final head, and reduce the hip.
- Replace the Nr. 17 retractor outside the capsule. Reapproximate the capsule with a nonabsorbable suture.
- Repair the gluteal fascia with a synthetic braided absorbable suture while the leg is in slight abduction and external rotation. Close the subcutaneous tissue with a 2-0 braided absorbable suture and skin with sterile skin staples.
Wyniki
At 6 weeks after THA, the mean OHS was 35 points after the ABMS approach and 29 after the PA (p = 0.0408). The HOOS and FJS did not differ significantly 6 weeks after THA between the ABMS approach and PA. At 6 months after THA, no differences in outcome scores were observed (Table 1).
In the first 10 THAs using the ABMS approach, one patient had a greater trochanter fracture treated with a tension band suture, and one patient had an intraoperative proximal femur fracture treated with a revision cone femoral stem. No further immediate interoperative or postoperative complications occurred. Surgery time significantly reduced with the number of THAs performed from a mean of 113 min for the first 10 patients to a mean of 67 min for the THAs 21-30 (Table 2).
At 6 weeks, the presented patient had an OHS of 42, HOOS Junior of 85, and FJS of 100. The patient used a walking aid for the first 4 days and could return to his desired activities without restrictions 3 weeks after surgery. His post-operative X-rays demonstrated restored leg length and femoral offset (Figure 3).
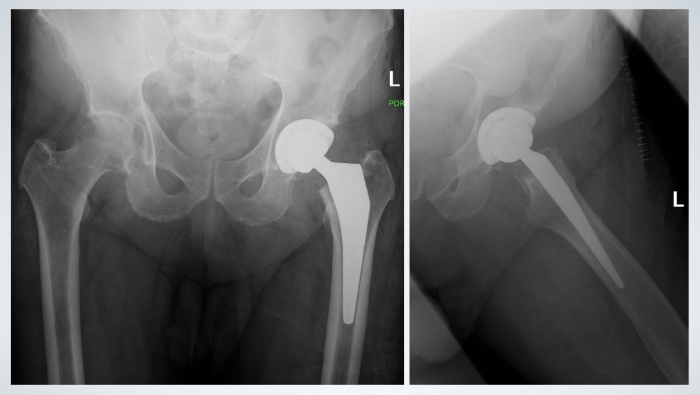
Figure 3: Postoperative AP and lateral radiograph. Composite shows the postoperative AP and lateral radiograph of the pelvis and left hip, respectively. Leg length and femoral offset are restored. The position of the acetabular component is within acceptable ranges. Please click here to view a larger version of this figure.
| THA approach | ||||
| ABMS approach | PA | Significance | ||
| 6 weeks after THA | ||||
| Oxford hip score (OHS) | Mean ± SD | 35 ± 9.7 | 29 ± 10.7 | p = 0.0481* |
| (48 best, 0 worst) | ||||
| Hip Injury and osteoarthritis outcome score (HOOS) | Mean ± SD | 73 ± 14.3 | 70 ± 16.3 | NS, p = 0.3745* |
| (100 best, 0 worst) | ||||
| Forgotten joint score (FJS) | Mean ± SD | 51 ± 29.7 | 44 ± 30.5 | NS, p = 0.4008* |
| (100 best, 0 worst) | ||||
| 6 months after THA | ||||
| Oxford hip score (OHS) | Mean ± SD | 44 ± 5.3 | 44 ± 4.6 | NS, p = 0.8879* |
| (48 best, 0 worst) | ||||
| Hip Injury and osteoarthritis outcome score (HOOS) | Mean ± SD | 89 ± 14.4 | 84 ± 13.9 | NS, p = 0.3145* |
| (100 best, 0 worst) | ||||
| Forgotten joint score (FJS) | Mean ± SD | 86 ± 23.4 | 83 ± 25.2 | NS, p = 0.6994* |
| (100 best, 0 worst) | ||||
| Standard deviation (SD) | ||||
| *Student's T-test | ||||
Table 1: Comparison between the anterior-based muscle-sparing (ABMS) approach and the posterior approach (PA). The difference in Oxford Hip Score, Hip Disability and Osteoarthritis Outcome Score (HOOS), and Forgotten Joint Score between the anterior-based muscle-sparing (ABMS) approach and the posterior approach (PA) at 6 weeks and 6 months after THA (Student's T-test*).
| Groups of ten patients treated with ABMS approach | |||||
| 1–10 THAs | 11–20 THAs | 21–30 THAs | Significance | ||
| ANOVA | |||||
| Surgical Time (min) | Mean ± SD | 113 ± 23.4 | 104 ± 3.2 | 67 ± 9.2 | p < 0.0001* |
| Post-hoc Tukey’s test | vs. 11–20 THAs | vs. 21–30 THAs | vs. 1–10 THAs | ||
| NS, p = 0.4169# | p = 0.0009# | p < 0.0001# | |||
| Standard deviation (SD) | |||||
| *ANOVA | |||||
| #Post-hoc Tukey’s test | |||||
Table 2: Mean surgical time. The difference in the mean surgical time across the three patient groups (ANOVA* and post-hoc Tukey's test#), indicating a learning curve regarding surgical efficiency.
Dyskusje
Minimally invasive surgery (MIS) has gained interest in all fields of surgery due to the faster recovery, lower blood loss, and improved perioperative pain control. THA has adopted MIS to increase hip stability and enhance post-operative mobilization. The ABMS approach utilizes the muscle interval between the tensor fasciae latae and the gluteus medius muscles but without incising or detaching the muscles and tendons. A surgeon considering transitioning to the ABMS approach would be well advised to attend a cadaver course and ideally be accompanied by the first assistant. This will help them to become familiar with the critical surgical steps9. A few critical steps should be outlined: 1) incising the fascia overlying the GM just posterior to the intermuscular plane of the GM and TFL to avoid unnecessary muscle dissection; 2) adequate capsular release during the initial capsulotomy to help expose the acetabulum and femur; and 3) performing an in situ osteotomy instead of dislocating the hip to reduce the risk of femur fractures10.
Certain steps in the surgical technique can be modified depending on the surgeon's preference. Performing a capsulectomy instead of a capsulotomy does not influence the post-operative stability and does not add post-operative precautions3. Leg length can be restored by measuring the distance from the trochanteric fossa as described in this protocol or by measuring the distance from the lesser trochanter or the intertrochanteric tubercle9,11. As mentioned in the introduction, the ABMS approach can also be performed in the supine position, which requires a surgical table with the option to hyperextend the hips4.
While in the early phase of adapting to the ABMS approach, considerations can be made to limit patient population by body habitus or preoperative hip deformity; increasing comfort with the surgical technique makes the ABMS approach a generally applicable technique without patient selection restrictions10,12.
Compared to other approaches, clinical studies evaluating the ABMS approach demonstrate better short-term functional outcomes13, less muscle damage14, reliable implant positioning15, a low dislocation rate16, decreased post-operative pain and narcotic requirements, and finally, a shorter learning curve17. The results from the presented study confirm these results. Also, the learning curve in the present study demonstrated a reduction in surgical time over the first 30 THAs. This finding contrasts with previously published data, which showed a persistently long surgical time9. In agreement with the published literature, the present study confirms that the benefit of a muscle-sparing approach diminishes with longer follow-up9. The 6 month OHS indicates that patients do well regardless of the approach, and the risk of revision after ABMS approach is as low as after PA18,19. Further studies will reveal whether the adjunct of intraoperative technologies like navigation or augmented reality will further improve patient outcomes after ABMS approach THA20.
In conclusion, transitioning from PA to the ABMS approach is associated with a learning curve, which implies an increased risk of periprosthetic femur fractures and prolonged surgery times. After 10 THAs have been performed, the risk of femur fractures diminishes, and the surgical time normalizes after the first 20 THAs. Surgeons interested in providing their patients with faster recovery and avoiding post-operative restrictions might find these results valuable when considering changing their THA approach.
Ujawnienia
The authors have nothing to disclose.
Podziękowania
The authors have no acknowledgments.
Materiały
| Name | Company | Catalog Number | Comments |
| 30° Offset Masterloc Broach handle L | Medacta | 01.10.10.461 | |
| 30° Offset Masterloc Broach Handle R | Medacta | 01.10.10.460 | |
| 3D Printed Acetabular Component | Medacta | 01.38.058DH | |
| ACE Wrap 6 in | 140700 | ||
| Acetabular Liner | Medacta | 01.32.4048HCT | |
| AMIS 2.0 Genera Tray | Medacta | 01.15.10.0294 | Curved cup impactor |
| AMIS 2.0 General Tray | Medacta | 01.15.10.0293 | Screw driver for cup impactor |
| Anterior Auxillery | Medacta | ALAUX | |
| Biolox Ceramic Head | Medacta | 01.29.214 | |
| Chloraprep 26 mL | BD | 301185 | |
| Drape Mayostand | Cardianal | 7999 | |
| Ethibond Size 5 | Ethicon | 103831 | |
| Femoral Neck Elevator | 3006 | ||
| Femoral neck elevator | 01.15.10.0037 | ||
| Ioban | 3M | 15808 | |
| Ketorolac 30 mg/mL | SN | MED00575 | |
| Masterloc Inst (MLOCINS) | Medacta | 01.39S.301US | |
| Masterlock Femoral Stem | Medacta | 01.39.408 | |
| Mpact General (MPACT) | Medacta | 01.32S.300US | |
| Mpact Liner Trial face changing/offset | Medacta | 01.325.305 | |
| Mpact Liner Trial face changing/offset | Medacta | 01.325.305 | |
| Mpact liner trial flat/hooded | Medacta | 01.32S.301 | |
| Mpact liner trial flat/hooded | Medacta | 01.32S.301 | |
| Mpact Reamers (MPACT) | Medacta | 01.32S.101US | Regular hemi reamers swapped out for Half-Moon Reamers |
| Single Prong Acetabular Retractor, Extra Deep | 6570-01 | ||
| Single Prong Acetabular Retractor, Standard | 6570 | ||
| Single Prong Broad Acetabular Retractor | 6320 | ||
| Stapler Kine Proximate Plus 35 W | Ethicon | 52686 | |
| Tranexamic acid 1 g | SN | MED01071 | |
| Unger Narrow Hohmann | 3002 | ||
| Vicryl 1 CTX | Ethicon | 143836 | |
| Vicryl 2-0 CT2 | Ethicon | 9174 |
Odniesienia
- Melman, W. P., Mollen, B. P., Kollen, B. J., Verheyen, C. C. First experiences with the direct anterior approach in lateral decubitus position: Learning curve and 1 year complication rate. Hip International. 25 (3), 251-257 (2015).
- Rottinger, H. The MIS anterolateral approach for THA. Orthopade. 35 (7), 708-715 (2006).
- Bertin, K. C., Röttinger, H. Anterolateral mini-incision hip replacement surgery: A modified Watson-Jones approach. Clinical Orthopaedics and Related Research. 429, 248-255 (2004).
- Civinini, R., et al. The anterior-based muscle-sparing approach to the hip: The "other" anterior approach to the hip. International Orthopaedics. 43 (1), 47-53 (2019).
- De Geest, T., Fennema, P., Lenaerts, G., De Loore, G. Adverse effects associated with the direct anterior approach for total hip arthroplasty: A Bayesian meta-analysis. Archives of Orthopaedic and Trauma Surgery. 135 (8), 1183-1192 (2015).
- Christensen, C. P., Karthikeyan, T., Jacobs, C. A. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. The Journal of Arthroplasty. 29 (9), 1839-1841 (2014).
- Leiberman, J. R., Berry, D. J. Advanced Reconstruction: Hip 2. , Lippincott Williams & Wilkins. Philadelphia, PA. (2018).
- Delanois, R. E., et al. The Rottinger approach for total hip arthroplasty: Technique, comparison to the direct lateral approach and review of literature. Annals of Translational Medicine. 5, Suppl 3 31(2017).
- Martin, R., Clayson, P. E., Troussel, S., Fraser, B. P., Docquier, P. L. Anterolateral minimally invasive total hip arthroplasty: A prospective randomized controlled study with a follow-up of 1 year. The Journal of Arthroplasty. 26 (8), 1362-1372 (2011).
- Laffosse, J., et al. Learning curve for a modified Watson-Jones minimally invasive approach in primary total hip replacement: Analysis of complications and early results versus the standard-incision posterior approach. Acta Orthopaedica Belgica. 72 (6), 693(2006).
- Chen, D., Berger, R. A. Outpatient minimally invasive total hip arthroplasty via a modified Watson-Jones approach: Technique and results. Instructional Course Lectures. 62, 229-236 (2013).
- Rottinger, H. Minimally invasive anterolateral surgical approach for total hip arthroplasty: early clinical results. Hip International. 16, Suppl 4 42-47 (2006).
- de Jong, L., Klem, T. M., Kuijper, T. M., Roukema, G. R. The minimally invasive anterolateral approach versus the traditional anterolateral approach (Watson-Jones) for hip hemiarthroplasty after a femoral neck fracture: an analysis of clinical outcomes. International Orthopaedics. 42 (8), 1943-1948 (2018).
- Müller, M., Tohtz, S., Dewey, M., Springer, I., Perka, C. Evidence of reduced muscle trauma through a minimally invasive anterolateral approach by means of MRI. Clinical Orthopaedics and Related Research. 468 (12), 3192-3200 (2010).
- Kawarai, Y., et al. Does the surgical approach influence the implant alignment in total hip arthroplasty? Comparative study between the direct anterior and the anterolateral approaches in the supine position. International Orthopaedics. 41 (12), 2487-2493 (2017).
- Batailler, C., et al. Total hip arthroplasty using direct anterior approach and dual mobility cup: safe and efficient strategy against post-operative dislocation. International Orthopaedics. 41 (3), 499-506 (2017).
- D'Arrigo, C., Speranza, A., Monaco, E., Carcangiu, A., Ferretti, A. Learning curve in tissue sparing total hip replacement: Comparison between different approaches. Journal of Orthopaedics and Traumatology. 10 (1), 47-54 (2009).
- Rothwell, A. G., Hooper, G. J., Hobbs, A., Frampton, C. M. An analysis of the Oxford hip and knee scores and their relationship to early joint revision in the New Zealand Joint Registry. The Journal of Bone and Joint Surgery. British Volume. 92 (3), 413-418 (2010).
- Devane, P., Horne, G., Gehling, D. J. Oxford hip scores at 6 months and 5 years are associated with total hip revision within the subsequent 2 years. Clinical Orthopaedics and Related Research. 471 (12), 3870-3874 (2013).
- Alexander, C., et al. Augmented reality for acetabular component placement in direct anterior total hip arthroplasty. The Journal of Arthroplasty. 35 (6), 1636-1641 (2020).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaPrzeglądaj więcej artyków
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone