Method Article
Point of Care Transcranial Color-Coded Duplex Ultrasound of the Middle Cerebral Artery
W tym Artykule
Podsumowanie
Transcranial ultrasound is an essential tool for monitoring patients with various neurological conditions. Although it is commonly used in a protocolized fashion in consultative studies, the brain has been overlooked in many protocols utilizing point-of-care ultrasound (PoCUS). This study proposes a PoCUS image acquisition protocol.
Streszczenie
In the assessment and management of many clinical problems, point-of-care (PoC) ultrasound is an emerging bedside tool. Transcranial color-coded duplex (TCCD) ultrasound can be valuable in multiple situations, including for patients who are unconscious or have an equivocal neurologic examination, as it helps rule in specific intracranial pathologies. Despite the known diagnostic value of transcranial ultrasound, its use in critical care medicine remains variable. This variability is partly due to inconsistent training across hospitals, stemming from a lack of standardized education and training. Additionally, the brain has often been overlooked in many critical care protocols, such as RUSH (Rapid Ultrasound for Shock and Hypotension) and FAST (Focused Assessment with Sonography in Trauma) exams. To address these gaps, this article proposes a protocol for PoC TCCD image acquisition in adults, detailing indications, limitations, transducer selection, placement, sequence acquisition, and image optimization. Furthermore, the use of PoC TCCD is discussed as a means of screening for three conditions: vasospasm, raised intracranial pressure, and progression of cerebral circulatory arrest.
Wprowadzenie
First described by Aaslid et al. in 1982, transcranial Doppler (TCD) ultrasonography offered a method to evaluate intracranial blood flow and velocity1. Later, transcranial color-coded duplex ultrasound (TCCD) was developed to allow color-coded visualization of intracerebral vasculature. This permits TCCD to partly overcome a limitation of TCD: angle dependence. Specifically, as a result of Doppler shift, measurements of blood flow velocity are most accurate if the angle of the ultrasound beam and the axis of the vessel are between 0-30 degrees2. While flow velocity measurements in TCD assume an angle close to zero, TCCD allows visualization of the angle of insonation and thus angle-corrected velocity measurements3.
TCCD includes several Doppler measurements including but not limited to: pulsatility index (PI), mean flow velocities (MFV), and or time-adjusted velocity (TAV)4. Using these measurements, TCCD permits non-invasive screening for several important conditions including vasospasm, increased intracranial pressure (ICP), and cerebral circulatory arrest, each of which manifests with a unique hemodynamic and sonographic signature5.
Firstly, in the context of cerebral vasospasm following subarachnoid hemorrhage (aneurysmal or traumatic), TCCD provides real-time visualization of intracranial blood flow, allowing for the detection of narrowing or constriction of cerebral arteries. By measuring MFV (defined as end-diastolic velocity + 1/3(peak systolic velocity + end diastolic velocity)6, clinicians can quantify the severity of vasospasm up to 2.5 days prior to the onset of symptoms7. Concurrently, by measuring PI (defined as peak systolic velocity - end diastolic velocity)/mean velocity), one can detect elevated values (>1.2)7. Elevated values in turn suggest increased cerebrovascular resistance, highlighting the compromised distal perfusion associated with distal vessel vasospasm7or increased intracranial pressure. The combined use of TCCD, PI, and MFV facilitates early detection and monitoring of vasospasm, enabling prompt interventions to prevent ischemic injury and improve patient outcomes.
Second, in cases of increased ICP, cerebrovascular dynamics can be assessed through PI and MFV. PI and MFV reflect changes in cerebral blood flow and vascular resistance, both of which are impacted by elevations in ICP. Increased ICP may result in elevated PI values due to impaired cerebrovascular compliance, while decreased MFV indicates reduced cerebral perfusion secondary to elevated intracranial pressures4. Monitoring these parameters allows clinicians to gauge the severity of ICP elevation, guide treatment decisions, and assess the response to interventions aimed at lowering ICP.
Third, in the event of cerebral circulatory arrest, PI and MFV assessments play a critical role in confirming the cessation of cerebral blood flow. Rapid identification of cerebral circulatory arrest using TCCD and hemodynamic parameters is essential for initiating time-sensitive interventions, such as advanced neurocritical care measures, to restore cerebral perfusion if detected in a timely manner.
In summary, TCCD offers a non-invasive bedside tool to screen for cerebral vasospasm, increased ICP, and cerebral circulatory arrest. By providing real-time visualization and quantification of cerebral hemodynamics, TCCD enables clinicians to diagnose, monitor, and manage these critical neurological conditions, with potential for improving patient outcomes and reducing morbidity and mortality. But despite the known diagnostic value of transcranial ultrasound, point-of-care utilization of TCCD in critical care medicine remains variable, in part because training in this modality across hospitals is still inconsistent due to a lack of standardized training and education.
To address these gaps, this article proposes a TCCD image acquisition protocol in adults that can be used at the point-of-care (PoC). In general, a PoC ultrasound is one that is performed and interpreted by a patient's primary treating provider8. This is in contrast to a consultative ultrasound which is requested by a patient's primary treating provider but performed by a separate specialist team. Whereas consultative TCD or TCCD typically includes Doppler interrogation of multiple cerebral arteries, this PoC protocol centers on selective interrogation of the middle cerebral artery (MCA) for two reasons: (1) the MCA is typically the easiest branch of the Circle of Willis to insonate with TCCD and (2) The MCA is responsible for approximately 70% of the flow from the internal carotid artery, therefore analysis of the MCA can bring a good information about cerebral blood flow as a whole9.
This PoC TCCD protocol includes transducer selection and placement, sequence acquisition, and image optimization. Further, use of PoC TCCD will be discussed as a means of screening for the following three conditions: vasospasm, raised intra-cranial pressure, and progression of cerebral circulatory arrest.
Protokół
This procedure adheres to the ethical standards of the institutional committee on human experimentation and the Helsinki Declaration. Ultrasound is considered a minimal-risk procedure; therefore, written consent from the patient is generally not required. Patients with concerns about neurological changes in an appropriate clinical setting were included in the study. Those with open head wounds, surgical incisions, or surgical dressings at the insonation site were excluded. The consumables and equipment used in this study are listed in the Table of Materials.
1. Transducer selection
- Select the phased-array probe (1-5 MHz) for TCCD scan. This probe provides the smallest footprint for insonation of the transtemporal window.
NOTE: The term "phased-array probe" is often used to refer to the linear phased-array sector arc probe6,10. This terminology can be ambiguous, as all contemporary ultrasound transducers utilize phasing to direct the ultrasound beam. To keep things concise, this review will use "phased-array probe" in place of "linear phased-array sector arc probe.
2. Machine settings
- Set the machine to the transcranial preset. This preset is available in most modern machines. This sets the indicator to the right of the screen.
NOTE: If Transcranial preset is not available, the Cardiac preset can be utilized. The indicator will be to the left of the screen for this preset.- Set the initial mode to B-Mode (2-dimensional grayscale11). Set Depth 13-16 cm.
NOTE: This depth will capture a hyperechoic convex line, which represents the ipsilateral temporal bone, usually at a depth of about 1-2 cm. Whereas the contralateral temporal bone will be seen as concave hyperechoic structure at depth of 14-16 cm. - For the best scanning ergonomics, position the machine so that the ultrasound screen is directly in line with the ultrasound probe.
- Set the initial mode to B-Mode (2-dimensional grayscale11). Set Depth 13-16 cm.
3. Patient position
- Place the patient in a supine position with the head of the bed at 30 degrees.
4. Scanning technique
- Apply Gel to the probe.
- Place the probe on the transtemporal window (Figure 1), parallel to the ground with the index mark aimed towards the patient anterior.
NOTE: The transtemporal area lies just above the zygomatic arch and infront of the tragus of the ear6.
5. Transcranial views
- Use a sliding motion to scan through the nearby brain tissue until the intracranial structures that are relevant are identified. These act as a starting point to identify the landmarks needed for PoCUS TCCD.
- Identify the ipsilateral temporal bone, which is typically seen at around 1 cm11.
- Identify the contralateral temporal bone, which is typically around 14-16 cm11.
NOTE: The ipsilateral temporal window appears as a concave or linear hyperechoic structure. The contralateral temporal window is more concave looking11. - Identify the third ventricle, which appears as two hyperechoic lines with a thin hypoechoic structure in between which represent cerebrospinal fluid.
NOTE: This is typically seen at depth of 6-8 cm11. Use sliding or sweeping motion until structure above is identified12. This is not an essential step for this protocol. If not clearly identified can proceed with the next step.
6. Color Doppler interrogation of the middle cerebral artery (MCA)
- Start with the view obtained from the step in the prior section.
- Start by reducing the depth to have the far field be 10 cm.
- On the left side of the top half of the ultrasound screen locates the large color flow sampling box.
NOTE: The MCA should now appear as a linear structure with blood flow directed towards the ultrasound transducer. Red color indicates flow moving towards the transducer. - Initiate Pulse Wave Doppler and center the box over the MCA`s red color flow signal.
- Obtain a Spectral Doppler wave form.
NOTE: Normal MCA blood flow velocity displays a sharp systolic upstroke followed by a gradual deceleration during diastole13.- Trace the contour to measure the velocity time Integral for one cardiac cycle.
NOTE: In ultrasound with transcranial mode, multiple values will automatically be generated once the tracing is complete. - Ensure that MFV or Time Average Velocity (TAV) or Time adjusted peak velocity (TAP) or Time average maximum Velocity (TAMAX) is displayed. If not, calculate2 it by (PSV + (EDV x 2))/3.
NOTE: Mean flow velocity above 120 could raise the concern for possible increased risks of vasospasm. The Angle of insonation must ideally be between 0-30 degrees otherwise measured velocities will be underestimated14. Mean flow velocity (MFV), Time adjusted peak velocity (TAP), Time average maximum Velocity (TAMAX) and Time Average velocity (TAV) will be used interchangeably. - Ensure that Pulsatility index is displayed. If not, calculate it by using the formula PSV-EDV)/MFV15.
NOTE: The PI can be converted to an estimate of ICP using the following formula: ICP = (10.93 x PI)-1.28. Progression to PI > 2 could raise the concern for elevated ICP16. PI is resistant to off-axis insonation as it is a relative ratio. All measurements in this value will be affected equally thus PI value will remain preserved17.
- Trace the contour to measure the velocity time Integral for one cardiac cycle.
7. Post-procedural steps
- Review the acquired images and Doppler spectra to ensure that they meet diagnostic quality standards.
- Ensure that all images and Doppler data are properly saved and labeled for future reference and analysis.
- Inform the patient about any follow-up steps or additional tests if required.
Wyniki
This section will describe the analysis and interpretation of data obtained from the protocol above and its clinical utility. Figure 1 shows the physical location on the head where the TCCD is performed: in the transtemporal window. Figure 2 demonstrates this transtemporal window showing the ipsilateral MCA being interrogated with pulse-wave Doppler (PWD). With the PWD box placed at a depth of 45-65 mm18, a velocity profile should emerge that can be used to calculate MFW and PI. In this particular case, the Doppler data demonstrate a normal MFV (<80 cm/s) and normal PI (<1.2)19. In contrast, an MFV greater than 120 cm/s is abnormal. Such a value would be suggestive of vasospasm in patients with intracranial pathology at risk of causing vasospasm (e.g., subarachnoid hemorrhage).
For example, Figure 3 shows a PoC TCCD obtained on a patient with acute neurological changes on day 8 following right middle cerebral artery aneurysm coiling for subarachnoid hemorrhage. The PoC TCCD revealed elevated mean flow velocity in the ipsilateral MCA compared to prior studies. Subsequently CT angiography of the head was performed, which confirmed vasospasm in the right anterior circulation.
In patients with intracranial pathology that could lead to intracranial hypertension, PoC TCCD can measure the PI to non-invasively screen for a high Intracranial pressure16,20,21. For example, Bellener et al. developed a simplified formula to estimate the relationship20: ICP = 10.93 × PI − 1.28.
Figure 4 shows a patient initially presented with intracranial hemorrhage and initial PoC TCCD had a normal PI. Later, the patient was noted to have worsening mental status, PoC TCCD was repeated and revealed elevated PI concerning for possible elevation in intracranial pressure. To treat this, hypertonic fluids were given and subsequent CT imaging revealed that the patient's hemorrhage was worsening.
PoC TCCD can also be used to screen for progression to cerebral circulatory arrest that precedes brain death. The progression to brain death typically includes a regression in cerebro-arterial flow with an increase in resistivity (Figure 5). These PoC TCCD findings should lead clinicians to obtain further ancillary testing including a comprehensive TCCD study for the purpose of definitive determination of circulatory arrest in accordance with institution-specific guidelines. As an example, Figure 6 is a PoC TCCD of a patient few hours after a prolonged cardiac arrest and subsequent return of cardiac circulation. The immediate trigger for the PoC TCCD exam was the physical exam finding of fixed and non-reactive pupils. Although no consultative TCCD service was available at facility and the patient was too unstable for apnea testing, the PoC TCCD findings were supported by a subsequent CT of the head which revealed diffuse cerebral edema.
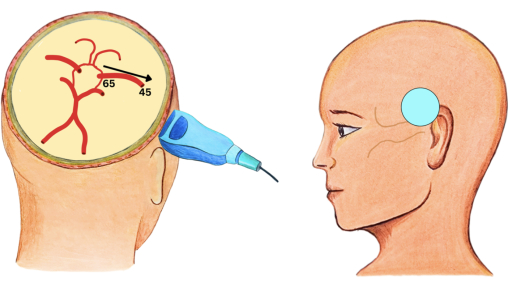
Figure 1: Transtemporal window. Transtemporal window with simplified schematic of circle of Willis. The numbers represent the depth that the ipsilateral MCA will be visualized on the ultrasound. The arrow represents the directionality of blood flow. The blue circle represents the location where the probe should be placed. Please click here to view a larger version of this figure.
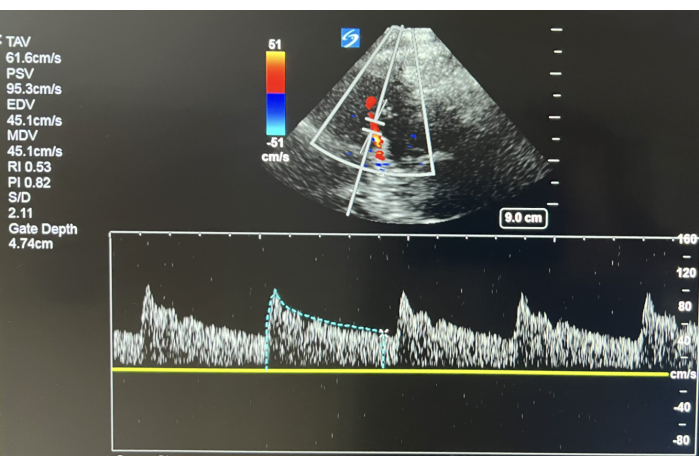
Figure 2: Normal TCCD. TCCD of the Ipsilateral MCA at Depth of 47 mm. The image reveals normal TAV and Normal PI. Please click here to view a larger version of this figure.
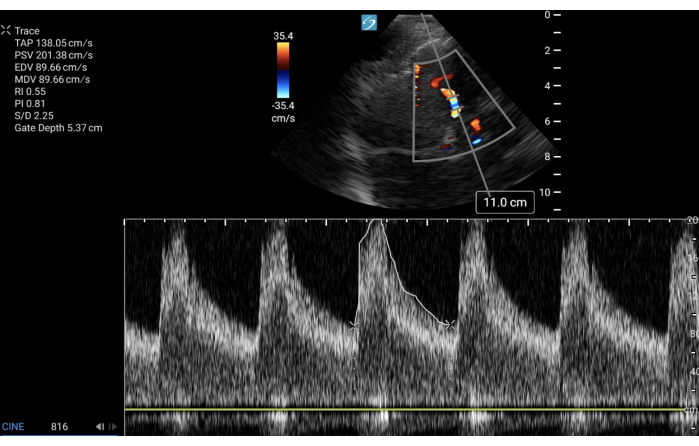
Figure 3: TCCD with elevated mean flow velocity. TCCD of the Ipsilateral MCA at Depth of 50 mm. This image reveals elevated TAP: Time adjusted peak velocity (equivalent for MFV or TAV or TAMAX) and Normal PI. In appropriate clinical setting, this suggests vasospasm. Please click here to view a larger version of this figure.
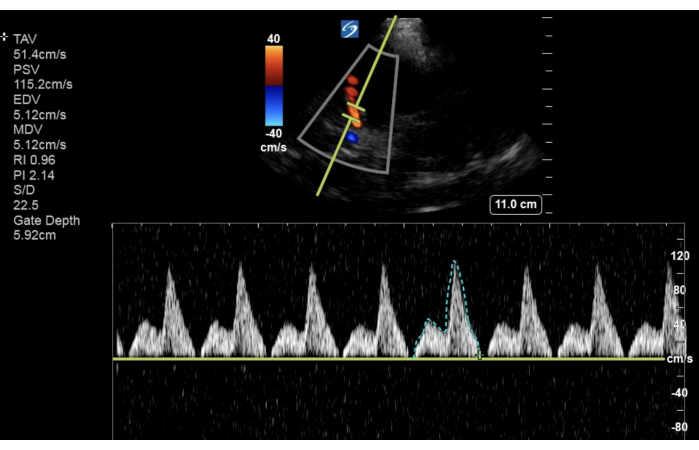
Figure 4: TCCD with elevated pulsatility index. TCCD shows worsening PI with clinical correlation concerning for increasing intracranial pressure in appropriate clinical setting. Please click here to view a larger version of this figure.

Figure 5: Transcranial Doppler progression in cerebral circulatory arrest. Schematic representation of the expected progressive changes in the waveform morphology of the middle cerebral artery as seen on TCD/TCCD in progression to cerebral circulatory arrest. Please click here to view a larger version of this figure.
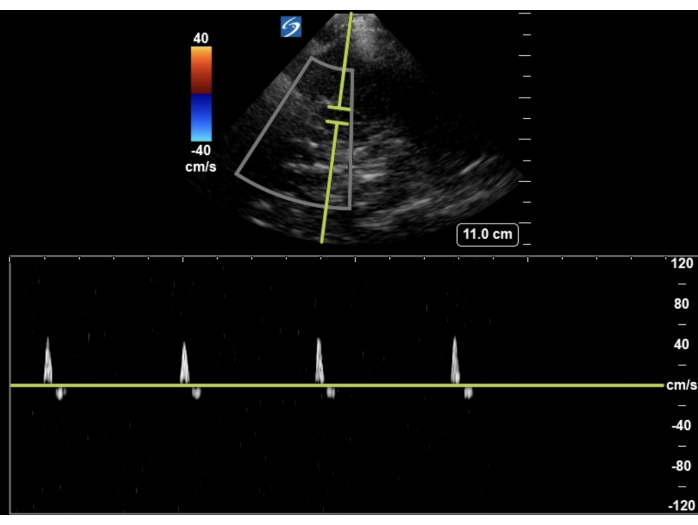
Figure 6: TCCD of cerebral circulatory arrest. Small systolic spikes with small diastolic reversal concerning progression toward cerebral circulatory arrest. Please click here to view a larger version of this figure.
Dyskusje
PoC ultrasound is increasingly playing a vital role in the diagnosis and management of patients with acute organ dysfunction, as seen with RUSH and FAST exams. However, when evaluating cerebral function, to date there is little published guidance for clinicians seeking to perform PoC TCCD.
To develop this PoC protocol, we chose to adapt TCCD rather than TCD imaging. In contrast to traditional TCD, TCCD combines B-mode and color Doppler, allowing for angle correction that results in more accurate measurement of flow velocity22. Further, this protocol proposed in this manuscript abbreviated existing TCCD protocols to focus on a single sonographic window: the trans-temporal. This is because the trans-temporal window is more easily accessible with ultrasound than the alternatives such as the trans-orbital and trans-foraminal12. Further, the trans-temporal window provides the most optimal insonation location to estimate the cerebral blood flow velocity (CBFV) of the MCA, which is the largest artery in the anterior cerebral circulation and receives approximately 70% of the internal carotid artery's blood flow4.
Although the concept of PoC TCCD remains in its nascency, there is some published evidence supporting its use in clinical practice. For example, when screening for increased intra-cranial pressure in the acute setting , PoC TCCD has been shown to provide a rational screening tool for increasing ICP5,23. Based on this existing evidence, European Society of Intensive Care Medicine now lists TCCD as a tool for intensivist to consider when screening patients for elevated ICP24. For the scenario of brain death screening, a meta-analysis in 2016 of 22 published studies showed that TCD detected cerebral circulatory arrest with sensitivity 0.9% and specificity 0.9825.
Although PoCUS TCCD has its advantages, there are also important limitations. First, the exam can be technically difficult in the setting of a poor temporal bone acoustic window, especially in the elderly, with incomplete insonation occurring in 10% of patients with cerebrovascular diseases22. Second, the absolute velocities obtained from TCCD in vasospasm evaluation may misestimate true arterial blood flow velocities since the normal velocities reported are more extensively validated for non-imaging probes utilized in TCD26. Nonetheless, new emerging studies are suggesting that values are at least comparative between the two modalities3. Third, when utilizing TCCD to evaluate the progression of cerebral circulatory arrest, studies have shown that despite the presence of reassuring spectral Doppler waveforms, the mean cerebral flow may be inadequate to sustain life since patients can still qualify as brain death based on validated clinical testing25,27. Fourth, the PI used to estimate ICP level has a wide confidence interval, and thus caution should be made when utilizing the PI to correlate with a specific ICP level28. The wide confidence interval in the relationship between PI and ICP occurs because multiple factors can influence PI without impact on ICP. For instance, changes in PaCO2 or increased arterial blood pressure can affect cerebral blood flow and PI independently of ICP29. A decrease in CPP, which presents an increasing trend in PI, can be either from increased ICP or decrease in MAP. As such, PI is inversely proportional to a mean CPP or directly proportional to arterial blood pressure. Thus, it is recommended that the utilization of increasing PI be used to follow increasing ICP and decreasing CPP trends over time, and not for ICP absolute values30. Even with this in mind, confounders such as lack of pulsatile flow from V-A ECMO or LVAD makes PI uninterpretable for ICP correlate12.
Even with these limitations, PoC TCCD has value as a bedside screening tool in the diagnosis and management of acute neurologic dysfunction. By developing this point-of-care protocol, the hope is to demystify TCCD to non-neurosonologists tasked with caring for the critically ill, especially in resource limited settings.
Ujawnienia
None.
Podziękowania
None.
Materiały
| Name | Company | Catalog Number | Comments |
| Low Frequency Ultrasound Probe (C35xp) | SonoSite (FujiFilm) | P19617 | |
| SonoSite X-porte Ultrasound | SonoSite (FujiFilm) | P19220 | |
| Ultrasound Gel | AquaSonic | PLI 01-08 |
Odniesienia
- Aaslid, R., Markwalder, T. M., Nornes, H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 57 (6), 769-774 (1982).
- Nicoletto, H. A., Burkman, M. H. Transcranial Doppler series part II: Performing a transcranial Doppler. Am J Electroneurodiag Technol. 49 (1), 14-27 (2009).
- Gunda, S. T., et al. A comparative study of transcranial color-coded Doppler (TCCD) and transcranial Doppler (TCD) ultrasonography techniques in assessing the intracranial cerebral arteries haemodynamics. Diagnostics (Basel). 14 (4), 387 (2024).
- Caldas, J., Rynkowski, C. B., Robba, C. POCUS, how can we include the brain? An overview. J Anesth Analg Crit Care. 2 (1), 55 (2022).
- Rajajee, V., et al. Transcranial color-coded sonography with angle correction as a screening tool for raised intracranial pressure. Crit Care Explor. 5 (9), e0953 (2023).
- Bathala, L., Mehndiratta, M., Sharma, V. Transcranial Doppler: Technique and common findings (part 1). Ann Indian Acad Neurol. 16 (2), 174 (2013).
- Barlinn, K., et al. Increased pulsatility of the intracranial blood flow spectral waveform on transcranial Doppler does not point to peripheral arterial disease in stroke patients. J Stroke Cerebrovas Dis. 24 (1), 189-195 (2015).
- Bronshteyn, Y. S., Blitz, J., Hashmi, N., Krishnan, S. Logistics of perioperative diagnostic point-of-care ultrasound: Nomenclature, scope of practice, training, credentialing/privileging, and billing. Int Anesthesiol Clin. 60 (3), 1-7 (2022).
- Robba, C., et al. Basic ultrasound head-to-toe skills for intensivists in the general and neuro intensive care unit population: Consensus and expert recommendations of the european society of intensive care medicine. Intensive Care Med. 47 (12), 1347-1367 (2021).
- Fischetti, A. J., Scott, R. C. Basic ultrasound beam formation and instrumentation. Clin Tech Small Anim Pract. 22 (3), 90-92 (2007).
- . Aium practice guideline for the performance of a transcranial Doppler ultrasound examination for adults and children. J Ultrasound Med. 31 (9), 1489-1500 (2012).
- Lau, V. I., Arntfield, R. T. Point-of-care transcranial Doppler by intensivists. Crit Ultrasound J. 9 (1), 21 (2017).
- Naqvi, J., Yap, K. H., Ahmad, G., Ghosh, J. Transcranial Doppler ultrasound: A review of the physical principles and major applications in critical care. Int J Vasc Med. 2013, 1-13 (2013).
- Lepic, T., et al. Importance of angle corection in transcranial color-coded duplex insonation of arteries at the base of the brain. Vojnosanit Pregl. 72 (12), 1093-1097 (2015).
- Gosling, R. G., King, D. H. The role of measurement in peripheral vascular surgery: Arterial assessment by Doppler-shift ultrasound. Proc Royal Soc Med. 67 (6P1), 447-449 (1974).
- Chan, K. -. H., Miller, J. D., Dearden, N. M., Andrews, P. J. D., Midgley, S. The effect of changes in cerebral perfusion pressure upon middle cerebral artery blood flow velocity and jugular bulb venous oxygen saturation after severe brain injury. J Neurosurg. 77 (1), 55-61 (1992).
- White, H., Venkatesh, B. Applications of transcranial Doppler in the ICU: A review. Intensive Care Med. 32 (7), 981-994 (2006).
- Alexandrov, A. V., Neumyer, M. M., Alexandrov, A. V. . Cerebrovascular ultrasound in stroke prevention and treatment. , 17-32 (2004).
- Alexandrov, A. V., et al. Practice standards for transcranial Doppler (TCD) ultrasound. Part II. Clinical indications and expected outcomes. J Neuroimaging. 22 (3), 215-224 (2012).
- Bellner, J., et al. Transcranial Doppler sonography pulsatility index (pi) reflects intracranial pressure (icp). Surg Neurol. 62 (1), 45-51 (2004).
- Czosnyka, M., Matta, B. F., Smielewski, P., Kirkpatrick, P. J., Pickard, J. D. Cerebral perfusion pressure in head-injured patients: A noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg. 88 (5), 802-808 (1998).
- Nedelmann, M., et al. Consensus recommendations for transcranial color-coded duplex sonography for the assessment of intracranial arteries in clinical trials on acute stroke. Stroke. 40 (10), 3238-3244 (2009).
- Rasulo, F. A., et al. Transcranial Doppler as a screening test to exclude intracranial hypertension in brain-injured patients: The impressit-2 prospective multicenter international study. Critical Care. 26 (1), 110 (2022).
- Robba, C., et al. Basic ultrasound head-to-toe skills for intensivists in the general and neuro intensive care unit population: Consensus and expert recommendations of the european society of intensive care medicine. Intensive Care Med. 47 (12), 1347-1367 (2021).
- Chang, J. J., Tsivgoulis, G., Katsanos, A. H., Malkoff, M. D., Alexandrov, A. V. Diagnostic accuracy of transcranial Doppler for brain death confirmation: Systematic review and meta-analysis. Am J Neurorad. 37 (3), 408-414 (2016).
- Baumgartner, R. W. Transcranial color-coded duplex sonography. J Neurol. 246 (8), 637-647 (1999).
- Hassler, W., Steinmetz, H., Pirschel, J. Transcranial Doppler study of intracranial circulatory arrest. J Neurosurg. 71 (2), 195-201 (1989).
- Zweifel, C., et al. Reliability of the blood flow velocity pulsatility index for assessment of intracranial and cerebral perfusion pressures in head-injured patients. Neurosurg. 71 (4), 853-861 (2012).
- Simm, R. F., De Aguiar, P. H. P., De Oliveira Lima, M., Paiva, B. L., Zuccarello, M., et al. . Cerebral vasospasm: Neurovascular events after subarachnoid hemorrhage. , 75-76 (2013).
- De Riva, N., et al. Transcranial Doppler pulsatility index: What it is and what it isn't. Neurocritic Care. 17 (1), 58-66 (2012).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone