Method Article
Full Endoscopic Interlaminar Approach for Paracentral L5-S1 Disc Herniation
In This Article
Summary
Here, we present a protocol to describe the full endoscopic interlaminar approach (FEILA) technique, including every cutoff step required to reach technical proficiency. FEILA is a surgery with a relatively steep learning adaptation. Despite this, any surgeon capable of microdiscectomy can perform FEILA with enough practice and suitable patient selection.
Abstract
The full endoscopic interlaminar approach (FEILA) is a minimally invasive technique for lumbar discectomy. It has multiple advantages over other conventional discectomy methods, including less traumatization of the soft tissues, fewer complication rates (dural injury, bleeding), rapid rehabilitation, quick return to daily life activities, and preferable cosmetic results. FEILA is a surgery with a relatively steep learning adaptation. Endoscopic surgery is a closed tubular approach, and all surgical maneuvers are performed within a uniportal single working channel. Also, the technique has not yet been standardized and well-documented. Therefore, the early learning stages of this technique may not be easy for most surgeons. Despite these, FEILA is easy, and the operation length is comparable to and even shorter than other techniques of lumbar discectomy. FEILA for lumbar discectomy could be considered a safe and effective alternative procedure for paracentral L5-S1 disc herniation. Here, we describe the technique of FEILA, including every cutoff step required to reach technical proficiency for surgeons who want to start applying this approach.
Introduction
Lumbar degenerative disc disease is an anatomical and morphological change causing clinical complaints1. Surgery is the appropriate treatment in cases that do not respond to conservative treatments2. Conventional surgeries have been used, but they have disadvantages such as prolonged hospital stay, high amount of tissue damage, delayed mobilization, and risk of epidural fibrosis and instability. Because of these disadvantages, researchers have tried to develop less invasive methods. The full endoscopic (interlaminar-transforaminal) technique with posterolateral access evolved out of this2.
Due to the lateral iliac blocks of the L5-S1 segment, the transforaminal approach is limited. However, the L5-S1 level usually has the widest interlaminar window and a sufficient interval for the endoscope to fit. FEILA provides a direct route for decompression at the L5-S1 level. Therefore, this article aims to enable surgeons who are trying this technique for the first time to learn the technique in more detail and faster.
FEILA is a minimally invasive method to decompress lumbar disc herniation under excellent visualization and continuous saline irrigation3,4. FEILA is performed via a dilator placed through a small skin incision in the lumbar region. The dilator allows surgeons to place the working sleeve and endoscope over the dilator. Then, the surgeons use tools through the endoscope to perform a discectomy and decompression of the nerve. It has multiple advantages compared to conventional surgeries, including less traumatization of the soft tissues, fewer complication rates (less dural injury and bleeding), rapid rehabilitation, quick return to daily life activities, better cosmetic results, and a lower cost4.
FEILA is a surgery with a relatively steep learning adaptation. Because full endoscopic surgery is a closed tubular approach, all surgical maneuvers are performed within a uniportal single working channel5. In addition, the technique has not yet been standardized and well-documented. Therefore, the early learning stages of this technique may not be easy for most surgeons6. Despite these facts, the surgery is easy, and the operation length is comparable to and even shorter than other techniques of lumbar discectomy, especially at the L5-S1 level.
Surgical indications and contraindications for FEILA are evaluated after physical examination of the patients and neuroradiological imaging (X-ray and magnetic resonance imaging [MRI]) are performed. FEILA is indicated for sequestered or non-sequestered disc herniations (especially paracentral disc herniation), recurrent disc herniations after traditional or other minimally invasive methods, zygapophyseal joint cysts, and lateral bony and ligament spinal canal stenosis. FEILA is contraindicated for compressive intra- or extraforaminal pathologies, extensive central spinal canal stenoses, a pronounced bony shift in the interlaminar window and calcified discs, severe adhesion due to fibrotic tissue, fusions or instabilities in the spinal canal, cauda equina syndrome, weakness without pain, spondylodiscitis, and other severe spine infections7,8,9.
Protocol
The study protocol was approved by the institutional review board of the Istanbul Faculty of Medicine. Written consent was obtained from the patients before the surgical procedure.
1. Preoperative procedures
- Perform the procedure under general anesthesia with an anesthetist. Set the endoscopic and optic instruments, and C-arm devices in the operation room.
- Ensure the following tools are available for the procedure; dilator, working sleeve, endoscope with a 20° viewing angle, Kerrison punch, ronguer, punch, tip control radioblator probe that applies a radiofrequency current of 4 MHz, fluid conrol irrigation, and suction pump devices.
2. Technical note
- Position of patient
- Place the patient in a prone position (support the thorax and pelvis with pillows) with the hip and knee flexed to achieve a wider interlaminar space.
- Preparing the surgical field
- Sterilize the lumbar region with iodine or chlorhexidine (10%).
- Use sterile sheets to outline the prepared surgical site.
- Drape the operation field and C-arm with a waterproof surgical drape.
- Determine the entry point.
- Obtain an anteroposterior (AP) X-ray view and mark the interlaminar space at the L5-S1 level (Figure 1A).
NOTE: The C-arm is a device that can rotate 360° around the patient and obtain anteroposterior (AP) and lateral X-ray views intraoperatively. - Mark (with a sterile, surgical skin marker) as close to medial in the craniocaudal middle of the interlaminar window as possible for enough lateral access.
- Obtain an anteroposterior (AP) X-ray view and mark the interlaminar space at the L5-S1 level (Figure 1A).
- Incision
- Make a 10 mm skin incision as close to the midline as possible with a 20-blade.
- Check that the fascia of the paraspinal muscle has been passed.
- Insertion of the dilator
- Insert the dilator through the incision and laterally advance until it reaches the facet joint (Figure 1B).
- Obtain a lateral and AP X-ray view with the C-arm to confirm that the tip of the dilator is at the desired level and facing toward the facet joint of the ipsilateral pathology.
- Insertion of working sleeve
- Slide the working sleeve with the beveled opening toward the midline over the dilator.
- Obtain a lateral X-ray view with the C-arm to confirm that the tip of the working sleeve has reached the end of the dilator.
- Remove the dilator.
- Introduce the endoscope.
- Introduce an endoscope with a continuous inflow of saline (0.9% sodium chloride) over the working sleeve until the interface of the ligamentum flavum and muscle (Figure 1C).
NOTE: The flow rate is arranged by fluid control irrigation and suction pump devices. There is no specific rate flow. The surgeon can arrange the rate of flow to obtain optimum visualization. - Perform the rest of the procedure with continuous irrigation. Fluid flow will keep the surgical field clear. Control any risk of bleeding with the fluid pressure and direct application of the cautery (RF 4 Mhz).
- Introduce an endoscope with a continuous inflow of saline (0.9% sodium chloride) over the working sleeve until the interface of the ligamentum flavum and muscle (Figure 1C).
- Exposure of ligamentum flavum
NOTE: The first structures to be visualized after the endoscopic introduction should be at the interface of the ligamentum flavum and muscle.- Remove the soft tissues using a rongeur until the ligament flavum is exposed (Figure 1D).
- Perform bone resection via a high-speed burr to achieve a wider interlaminar space if there is not a wide enough interlaminar window to fit the endoscope.
- Resection of ligamentum flavum
- Tense the ligamentum flavum with the long side of the working sleeve.
- Separate the ligamentum flavum from the dura for a safer resection, as the dura is more prominent in the midline.
- Begin the ligamentum flavum resection from the medial side using a 5.4 mm punch.
- Control the cutting edge of the punch while the ligamentum flavum is being resected. Doing so otherwise risks a dural tear.
- Continue ligamentum flavum resection laterally until the lateral recess and pedicle are visualized to expose the nerve root and its lateral border (Figure 1E).
- Discectomy
- Remove the epidural fat tissue totally using the rongeur for a clear view of the compression.
- Mobilize the nerve root medially using the dissector to relieve it from any adhesions.
- Rotate the long side of the working sleeve clockwise or counterclockwise to medialize the nerve root and expose the pathology (Figure 1F).
- Visualize the anterior epidural space, annular defect, disk interval, and end plates.
- Remove the migrated disc material and loosen the fragments under the annulus through the defect if they are present and visualized.
- Use the punch to open the posterior longitudinal ligament and the annulus fibrosis if there is a subligamentous protruding material.
- Use the rongeur to remove the disc material, after detecting the annular defect and disc material in both situations.
- Use the punch to obtain enough space if no annular defect is encountered or the annular defect is too narrow for sufficient removal.
- Evacuate the disc space with the rongeur or punch until achieving nerve root decompression.
- During the discectomy, do not perform excessive retraction, so as to prevent neural trauma. Intermittent release or de-rotation of the working sleeve is necessary to decrease neurological complications.
- After the discectomy, coagulate the defect of the annulus by bipolar electrocautery for sealing and hemostasis purposes.
- Achieve hemostasis in every procedure step with continuous fluid flow or bipolar electrocautery (RF 4 Mhz).
- Remove the endoscope and working sleeve.
- Close the incision with a single proline suture (2.0) without drainage.
3. Postoperative procedures and follow-up
- The hospital stay is short, and mobilization is immediateon the day of surgery.
- Discharge the patients the next day if there are no complaints.
NOTE: Rehabilitation and physical therapy are not necessary. Analgesics and rehabilitative measures are not primarily necessary. - Recommend the patients to be admitted to an outpatient clinic in the 1st and 4th weeks.
Results
A 52-year-old male patient presented with low back pain radiating down his left leg without motor weakness for 6 months. The visual analog scale (VAS) score was 6/10 on the trunk and 8/10 on the left leg. The patient's symptoms were resolved and he was discharged the day after surgery. The postoperative follow-up VAS score was 2/10 on the trunk and 2/10 on the left leg. The preoperative and postoperative lumbar MRI of the patient showed total removal of the disc material by the full endoscopic interlaminar approach (Figure 2). The procedure can easily be performed under X-ray guidance. The incision is planned as medially as possible at the interlaminar window. Once incision of the skin and fascia of the paraspinal muscles is achieved, the dilator and working sleeve are introduced, and finally, the endoscope itself. The procedure is performed under direct visualization achieved under continuous irrigation. The cranial and caudal lamina, descending and ascending facets, and ligamentum flavum are the main landmarks. The ligamentum flavum and the epidural fat tissue are removed. Then, the main dura and the compressed nerve root are exposed. All these can be performed easily by experienced surgeons. The nerve root is mobilized and retracted medially by the working sleeve through rotation. Disc material is isolated and removed, and decompression of the nerve root is achieved (Figure 1).
The average operation time of 66 patients who were operated on in last 3 years was 57 min (32-78) in our department. No drainage was required. Intraoperative conversion to the microscopic procedure was encountered in two cases, because of technical glitches. Blood loss could not be measured due to continuous saline irrigation and suction. Early mobilization was encouraged without a lumbar corset (because no instability is expected) and patients were discharged the day after surgery. Wound care was easy, and wound healing was fast. There were no significant complications like spondylodiscitis, hematomas, or wound detachment. Four reoccurrences were revised with microendoscopic discectomy in the follow-up period (Table 1).

Figure 1: X-ray images and endoscopic views of the key steps of FEILA. (A) The interlaminar window for the L5-S1 interval is detected under an endoscopic image. (B)The dilator and working sleeve are inserted under lateral X-ray assistance. (C) Once the dilator is removed, the endoscope is introduced through the working sleeve. The system can be maneuvered freely. (D) After removing the initial soft tissues, the ligamentum flavum is exposed. (E) Then, the ligamentum flavum and the epidural fat tissue are removed, exposing the nerve root and the main dura. (F) The working sleeve is rotated to isolate the disc herniation to provide safe removal of the disc material. Please click here to view a larger version of this figure.
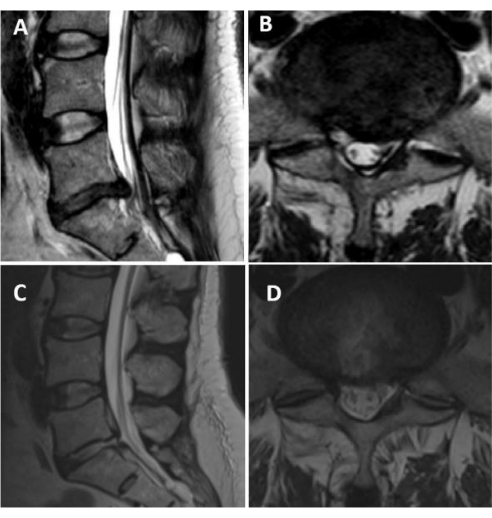
Figure 2: Magnetic resonance images (MRI) of a patient with left paracentral disc herniation. (A,B) Preoperative T2-weighted sagittal and axial MRI scans showing left paracentral disc herniation at the L5-S1 level. (C,D) Postoperative T2-weighted sagittal and axial MRI scans after full endoscopic interlaminar discectomy. A complete evacuation of the disc material can be appreciated. Please click here to view a larger version of this figure.
| Surgical outcomes | ||||
| Total number of patients | 66 | |||
| Average operation time | 57 min (32–78 min) | |||
| Drainage | not required | |||
| Number of patients who had to undergo intraoperative conversion to the microscopic procedure because of technical glitches | 2 | |||
| Number of patients with reoccurrences revised with microendoscopic discectomy | 4 | |||
| Complications | Spondylodiscitis | 0 | ||
| Hematomas | 0 | |||
| Wound detachment | 0 | |||
Table 1: Surgical outcomes.
Discussion
The results of recent studies depict the possibility of sufficient decompression via FEILA; these results are equal to those of traditional methods. Also, the advantages of the significant relief of back pain, faster recovery after surgery (short period of hospital stay), fewer complications, lower recurrence rate, minimizing soft-tissue disruption (small incision, less muscle cutting, less blood loss), and reducing segment instability have been shown10,11. So, as presented, FEILA is an effective and safe alternative to other traditional procedures. Despite these all advantages, FEILA also has disadvantages, such as a steep learning adaptation, Due to the difficulty in identifying the anatomical structure under endoscope visualization initially.
The steps of the technique are easy to apply. The L5-S1 interlaminar window is usually wide enough for the endoscope and working sleeve12. Therefore, drilling is not necessary most of the time. However, approaches for upper levels will require a drilling process13. Attention must be paid, especially to the resection of the ligamentum flavum and nerve retraction. If care is not taken, complications can develop, such as dural tearing, neural tissue injury, nerve root-induced hyperalgesia, and weakness. Another important point is the coagulation of the annulus defect to prevent the recurrence of disc herniation14,15.
FEILA has a long and challenging learning process at first. The technique is a closed tubular approach, and all surgical maneuvers are performed within a uniportal single working channel. In addition, it requires attention, especially in learning the anatomical orientation and manipulation of neural structures1. According to the literature regarding FEILA, the mean duration of surgery is 29 to 68.5 min16. Because of the learning curve, the time of earlier surgeries is longer17. In the case of a learning curve, any surgeon capable of microdiscectomy can perform FELIA with enough practice and suitable patient selection.
Endoscopic surgery has been successfully and widely used in managing spinal disease. FEILA, in particular, is becoming more popular, and the application area is expanding. Recently, Tsai et al. reported decompression of the nerve root due to a metastatic tumor with an endoscopic interlaminar approach. The progressive advancement of technology and instruments will help to manage many other spinal conditions with a broader range of other clinical situations, such as tumor and infection management, in the future18.
Materials
| Name | Company | Catalog Number | Comments |
| Burr Oval Ø 5.5 mm | RiwoSpine | 899751505 | PACK = 1 PC, WL 290 mm, with lateral protection |
| C-arm | ZIEHM SOLO | C-arm with integrated monitor | |
| Dilator ID 1.1 mm OD 9.4 mm | RiwoSpine | 892209510 | For single-stage dilatation, TL 235 mm, reusable |
| Endoscope | RiwoSpine | 892103253 | 20° viewing angle and 177 mm length with a 9.3 mm diameter oval shaft with a 5.6 mm diameter working channel |
| Kerrison Punch 5.5 mm x 4.5 mm WL 380 mm | RiwoSpine | 892409445 | 60°, TL 460 mm, hinged pushrod, reusable |
| Punch Ø 3 mm WL 290 mm | RiwoSpine | 89240.3023 | TL 388 mm, with irrigation connection, reusable |
| Punch Ø 5.4 mm WL 340 mm | RiwoSpine | 892409020 | TL 490 mm, with irrigation connection, reusable |
| Radioablator RF BNDL | RiwoSpine | 23300011 | |
| RF Instrument BIPO Ø 2.5 mm WL 280 mm | RiwoSpine | 4993691 | for endoscopic spine surgery, flexible insert, integrated connection cable WL 3 m with device plug to Radioblator RF 4 MHz, sterile, for single use |
| Rongeur Ø 3 mm WL 290 mm | RiwoSpine | 89240.3003 | TL 388 mm, with irrigation connection, reusable |
| Working Sleeve ID 9.5 mm OD 10.5 mm | RiwoSpine | 8922095000 | TL 120, distal end beveled, graduated, reusable |
References
- Wang, B., Lü, G., Patel, A. A., Ren, P., Cheng, I. An evaluation of the learning curve for a complex surgical technique: The full endoscopic interlaminar approach for lumbar disc herniations. The Spine Journal. 11 (2), 122-130 (2011).
- Jhala, A., Mistry, M. Endoscopic lumbar discectomy: Experience of first 100 cases. Indian Journal of Orthopaedics. 44 (2), 184-190 (2010).
- Ruetten, S., Komp, M., Merk, H., Godolias, G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine. 33 (9), 931-939 (2008).
- Passacantilli, E., et al. Endoscopic interlaminar approach for intracanal L5-S1 disc herniation: Classification of disc prolapse in relation to learning curve and surgical outcome. Asian Journal of Endoscopic Surgery. 8 (4), 445-453 (2015).
- Wang, B., Lü, G., Liu, W., Cheng, I., Patel, A. A. Full-endoscopic interlaminar approach for the surgical treatment of lumbar disc herniation: The causes and prophylaxis of conversion to open. Archives of Orthopaedic and Trauma Surgery. 132 (11), 1531-1538 (2012).
- Kuonsongtum, V., et al. Result of full endoscopic uniportal lumbar discectomy: Preliminary report. Journal of the Medical Association of Thailand. 92 (6), 776-780 (2009).
- Wagner, R., Haefner, M. Indications and contraindications of full-endoscopic interlaminar lumbar decompression. World Neurosurgery. 145, 657-662 (2021).
- Andersson, G. B., et al. Consensus summary on the diagnosis and treatment of lumbar disc herniation. Spine. 21 (24), 75-78 (1996).
- McCulloch, J. A., et al. Focus issue on lumbar disc herniation: macro- and microdiscectomy. Spine. 21 (24), 45-56 (1996).
- Ruetten, S., Komp, M., Merk, H., Godolias, G. Recurrent lumbar disc herniation after conventional discectomy: A prospective, randomized study comparing full-endoscopic interlaminar transforaminal versus microsurgical revision. Journal of Spinal Disorders & Techniques. 22 (2), 122-129 (2009).
- Ruetten, S., Komp, M., Merk, H., Godolias, G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: A prospective, randomized, controlled study. Journal of Neurosurgery. Spine. 10 (5), 476-485 (2009).
- Ebraheim, N. A., Miller, R. M., Xu, R., Yeasting, R. A. The location of the intervertebral lumbar disc on the posterior aspect of the spine. Surgical Neurology. 48 (3), 232-236 (1997).
- Hua, W., et al. Full-endoscopic discectomy via the interlaminar approach for disc herniation at L4-L5 and L5-S1. Medicine. 97 (17), e0585 (2018).
- Wasinpongwanich, K., et al. Full-endoscopic interlaminar lumbar discectomy: retrospective review of clinical results and complications in 545 international patients. World Neurosurgery. 132, e922-e928 (2019).
- Kim, H. S., Park, J. Y. Comparative assessment of different percutaneous endoscopic interlaminar lumbar discectomy (PEID) techniques. Pain Physician. 16 (4), 359-367 (2013).
- Li, Z. Z., Hou, S. X., Shang, W. L., Song, K. R., Zhao, H. L. The strategy and early clinical outcome of full-endoscopic L5/S1 discectomy through interlaminar approach. Clinical Neurology and Neurosurgery. 133, 40-45 (2015).
- Choi, J. Y., et al. A retrospective study of the clinical outcomes and significant variables in the surgical treatment of temporal lobe tumor associated with intractable seizures. Stereotactic and Functional Neurosurgery. 82 (1), 35-42 (2004).
- Tsai, S. H., Wu, H. H., Cheng, C. Y., Chen, C. M. Full endoscopic interlaminar approach for nerve root decompression of sacral metastatic tumor. World Neurosurgery. 112, 57-63 (2018).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved