Method Article
Laparoscopic Anatomical Hepatectomy Using Takasaki's Approach and Indocyanine Green Fluorescence Navigation
In This Article
Summary
Here, we present a protocol for laparoscopic anatomical hepatectomy using Takasaki's approach and indocyanine green fluorescence navigation in S4/5/7/8 resection.
Abstract
Laparoscopic anatomical liver resection is a standard treatment for liver cancer. Segmental resection of S4/5/7/8 is complex and lacks standardized procedures, leading to common complications. Innovative techniques are essential for enhancing safety and outcomes. A 45-year-old male with a history of hepatitis B, Child-Pugh Class A liver function, performance status (PS) score 0, and alpha-fetoprotein (AFP) level of 198.3 ng/mL was diagnosed with a 4 cm × 5 cm × 5 cm mass in S4/7/8, indicating primary hepatocellular carcinoma (HCC), closely associated with the middle and right hepatic veins (BCLC A). The 15-min retention rate of indocyanine green (ICG) was 7.8%. The standard liver volume (SLV) was 1073 mL, and the actual liver volume was 1345 mL. We performed laparoscopic resection of segments S4/5/8 and partial S7, resecting the middle hepatic vein (MHV) while preserving the right hepatic vein (RHV) because MHV was so closed with the tumor. The future liver remnant (FLR) was 590 mL, with an FLR/SLV ratio of 55%. The surgical procedure utilized Takasaki's approach to block the right anterior hepatic pedicle and fluorescence staining to identify the transection line. The operation lasted 205 min with an estimated blood loss of 150 mL. The patient experienced no postoperative complications and was discharged on the sixth day. Histopathology confirmed hepatocellular carcinoma with clear resection margins. Takasaki's approach, combined with ICG fluorescence navigation, significantly improves laparoscopic anatomical hepatectomy. This technique enhances visualization, reduces complications, and offers a new standard for complex liver resections.
Introduction
Laparoscopic anatomical hepatectomy has transformed the management of liver diseases, providing a minimally invasive alternative to traditional open surgical techniques. The ongoing evolution of hepatobiliary surgery emphasizes the need to reduce postoperative morbidity while ensuring adequate oncological and functional outcomes. Among the various surgical techniques, Takasaki's approach stands out as a promising strategy for anatomical liver resection. Unlike conventional methods, which may overlook critical vascular structures, Takasaki's technique focuses on a detailed understanding of liver anatomy, essential for preserving liver parenchyma and optimizing the surgical field during segmental resections1.
The liver's complex anatomy, characterized by a densely branched vascular and biliary system, poses significant challenges during surgical procedures. The resection of segments 4, 5, 7, and 8 -- areas critical for maintaining hepatic function and associated with higher complications risks -- requires careful planning and precision. Takasaki's approach enables surgeons to systematically assess and preserve the vascular supply and drainage of adjacent liver segments, thereby minimizing the risk of ischemia and postoperative liver failure2.
Furthermore, the incorporation of indocyanine green (ICG) fluorescence navigation technology enhances this surgical paradigm. ICG, administered intravenously, binds to plasma proteins, allowing for the visualization of hepatic blood flow and bile duct structures through near-infrared imaging3. This real-time feedback provides surgeons with a dynamic view of liver perfusion and helps identify critical anatomical landmarks. In particular, ICG fluorescence navigation is invaluable during complex resections, effectively delineating tumor margins and refining the assessment of vascular anatomy4.
In this study, we focus on the implementation of laparoscopic anatomical hepatectomy with Takasaki's approach, enhanced by ICG fluorescence navigation, for the resection of liver segments S4, S5, S7, and S8. We present a case that illustrates our surgical techniques, highlights the benefits of fluorescence guidance, and evaluates patient outcomes. Through this report, we aim to demonstrate the feasibility and efficacy of this integrated surgical approach, contributing to the advancement of minimally invasive strategies in hepatobiliary surgery5,6,7. The findings of this study underscore the importance of meticulous preoperative planning, advanced imaging integration, and continuous refinement of surgical techniques to enhance patient safety and improve postoperative recovery8.
Protocol
This study was approved by the Ethics Committee of the Third Affiliated Hospital of Sun Yat-Sen University, which waived the requirement for informed consent due to the anonymous retrospective design of this study.
1. Patient selection
- Confirm indication for surgery.
NOTE: A 45-year-old male who has a long history of hepatitis B and liver function Child-Pugh Class A, PS score 0, AFP level 198.3 ng/mL. MRI and CEUS showed a 4 cm 5 cm 5 cm tumor in S4/7/8, indicating primary HCC, closely associated with the MHV and RHV (Tumor stage is BCLC A). The 15-min retention rate of ICG is 7.8%. SLV was 1073 mL, and the actual liver volume was 1345 mL. According to National Comprehensive Cancer Network (NCCN) guidelines, it was decided to perform laparoscopic resection of liver segments S4/5/8 and partial S7 by resection of the MHV while preserving the RHV. Future liver remnant (FLR) was 590 mL, and FLR/SLV was 55%.
2. Informed consent
- Discuss the procedure, risks, benefits, and alternatives with the patient. Obtain informed consent.
3. Preoperative workup
- Perform routine laboratory tests, including complete blood count, liver function tests, and coagulation profiles.
- Conduct imaging studies to localize tumors and evaluate liver anatomy.
4. Operative setup
- Administer general anesthesia following standard protocols.
- Position the patient supine with the patient slightly rotated to the left.
- Place the trocars.
- Establish pneumoperitoneum using a Veress needle or open technique.
- Place 5 trocars: Place one 10 mm camera trocar in the umbilicus. Place the 5 mm or 10 mm working trocars in the left and right upper quadrants and possibly the epigastric region for the hepatotomy.
5. Surgical technique
- Laparoscopic exploration: Begin with a thorough abdominal exploration to assess for any metastatic disease or abdominal complications.
- Cholecystectomy: Expose the Calot's triangle, dissect the cystic duct and cystic artery, then double ligate their proximal ends. Transect the vessels and duct, dissect the gallbladder from the liver bed, and achieve hemostasis on the liver bed surface with electrocautery.
- Dissect the ligament.
- Use an ultrasound scalpel to dissect the round ligament of the liver, falciform ligament, and partial right coronary ligament.
- Expose the second hepatic portal and the root of the hepatic veins (RHV, MHV, and left hepatic vein [LHV])
- Identify the root of the MHV, and mark the left hepatic transection line using the electrocoagulation hook (1 cm right along the falciform ligament).
- Preempt a 12# catheter as the first hepatic portal block band for the pringle procedure.
- Perform intraoperative ultrasound scan (IOUS).
- Scan the entire liver to exclude any lesions not detected preoperatively. Select a high-frequency laparoscopic probe (7.5-10 MHz), preheat the ultrasound console, and adjust the gain to 50-65 dB.
- Scan the tumor location, size, and edge, especially the relationship with RHV and MHV.
- Scan the right/left glission pedicle and RHV/MHV location.
- Using an IOUS scan, mark the tumor margin using an electrocoagulation hook, ensuring the resection margin >1 cm.
- Perform anatomical resection (Takasaki's approach)
- Perform Pringle's maneuver to occlude hepatic hilum inflow, then dissect the right anterior hepatic pedicle via an extraperitoneal approach.
- Divide a few small branches of G5 and moderately free the right anterior hepatic pedicle to facilitate occlusion (use laparoscopic bulldog). This will make cutting off the right anterior hepatic pedicle easier after the subsequent liver parenchyma is split.
- Release the occlusion and observe the liver ischemia line.
- Administer ICG intravenously (3-5 mL, 0.025 mg/mL) after the closure of the right anterior glissonian pedicle. Use the fluorescence staining to observe the extent of the right anterior segment.
- Mark the left resection line along the right side of the falciform ligament, inclined toward the right anterior hepatic pedicle on the visceral surface. Mark the right resection line according to fluorescence staining.
- Perform liver parenchyma transection.
- Utilize ultrasonic scalpels and harmonic devices to initiate parenchymal transection along the demarcated line.
- Maintain hemostasis using bipolar electrocautery as needed.
- On the left side, divide several branches of the G4 and V4 until the root of MHV.
- Split the right liver parenchyma and divide the right anterior hepatic pedicle and MHV.
- Carefully dissect the tumor in S7 adjacent to RHV.
NOTE: As the tumor was closely associated with the MHV and RHV, the RHV was preserved over the MHV because the procedure FLR was 590 mL and FLR/SLV was 55%.
- Complete the resection.
- Separate the resected liver from the surrounding tissues.
- Carefully resect the targeted segments while ensuring all major vessels are secured.
- Specimen retrieval: Retrieve liver segments using an endoscopic retrieval bag through the largest port or an additional incision if necessary.
6. Postoperative care
- Monitoring: Monitor vital signs, fluid balance, and hepatic function in the postoperative period.
- Pain management: Administer appropriate analgesia (consider regional blocks if indicated).
- Early mobilization: Encourage early ambulation to enhance recovery.
- Follow-ups: Conduct follow-up visits to assess liver function and healing and address any postoperative complications.
7. Documentation and quality control
- Maintain a detailed operative report including the preoperative diagnosis, findings, techniques used, as well as intraoperative challenges and solutions.
- Review outcomes and complications in a structured manner for future quality improvement.
Results
The representative outcomes from the application of indocyanine green (ICG) fluorescence in laparoscopic liver resection demonstrate its significant impact on surgical outcomes, particularly in enhancing the visibility of vascular and biliary structures during procedures.
One of the most notable advantages of using ICG navigation during liver resection is its ability to clearly delineate resection margins not only on the Glissonian surface but also deep within the liver parenchyma. By differentiating vascularized from non-vascularized parenchyma, surgeons can more accurately identify ischemic lines, which is crucial for ensuring clear dissection planes and effective tissue removal while preserving vital structures. For instance, Figure 1 illustrates Takasaki's approach to blocking the right anterior hepatic pedicle, showcasing the surgical team's precise identification of the ischemic line.
Figure 2 highlights the right anterior segment after intravenous ICG administration, providing crucial intraoperative feedback on liver anatomy. This enhanced visualization contributes to the reported reduction in estimated blood loss to 150 mL (Table 1), suggesting that fluorescence guidance promotes more cautious dissection practices, helping surgeons avoid damaging surrounding vasculature.
The overall procedure duration of 205 min is reasonable for complex liver surgeries. The patient was discharged on the sixth day without major adverse events, such as hemorrhage or bile leaks, underscoring the safety of this technique (Table 1). Figure 3 and Figure 4 further demonstrate the post-resection anatomy, confirming the successful resection of critical vascular structures, including the LHV, MHV, IVC, and RHV, thereby minimizing the risk of complications.

Figure 1: Takasaki's approach. Takasaki's Approach to block the right anterior hepatic pedicle(using laparoscopic bulldog to block the right anterior hepatic pedicle and show the ischemic line) Please click here to view a larger version of this figure.

Figure 2: Fluorescence staining to identify the right anterior segment. Administer ICG intravenously 3-5 mL at a concentration of 0.025 mg/mL. Please click here to view a larger version of this figure.
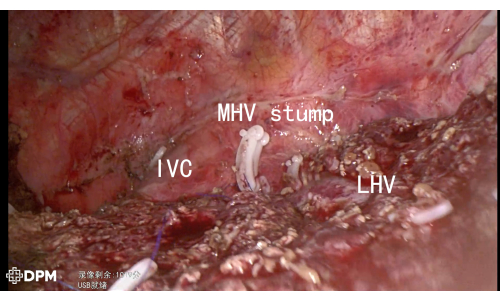
Figure 3: LHV/MHV/IVC demonstrated after liver resection. Please click here to view a larger version of this figure.
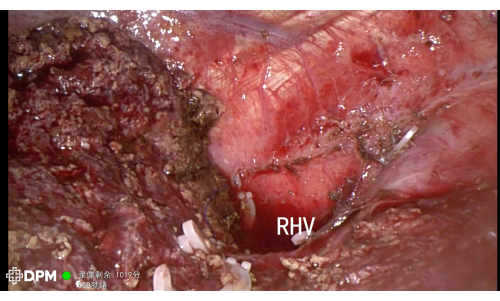
Figure 4: RHV demonstrated after liver resection. Please click here to view a larger version of this figure.
| Blood loss | 150 mL | |
| Duration | 205 min | |
| Hospital stay | 6 days | |
| Drainage | Day 1 | 200 mL |
| Day 4 | 50 mL | |
Table 1: The details of the surgery
Discussion
The laparoscopic anatomical hepatectomy using Takasaki's approach and ICG fluorescence navigation involves several critical steps that are essential for ensuring optimal outcomes. One of the most crucial aspects is the preoperative assessment, which includes imaging studies such as MRI and contrast-enhanced ultrasound (CEUS) to accurately localize the tumor and evaluate liver anatomy. This step is vital for planning the surgical approach, particularly for complex segmental resections (S4/5/7/8)9.
Another pivotal step is the administration of ICG. Administering ICG intravenously (3-5 mL, 0.025 mg/mL) after blocking the right anterior hepatic pedicle enhances the visualization of hepatic blood flow during surgery. This fluorescence guidance allows for real-time assessment of liver perfusion and aids in identifying critical anatomical landmarks10. Furthermore, the Takasaki approach emphasizes systematic dissection and preservation of vascular structures, which minimizes the risk of ischemia and postoperative liver failure11. The integration of intraoperative ultrasound (IOUS) for tumor margin assessment and vascular anatomy verification is also crucial, as it allows for precise demarcation of resection lines, ensuring clear margins and reducing complications12.
While the protocol is designed to be comprehensive, certain modifications may enhance its efficacy. For instance, the timing of ICG administration can be adjusted based on the patient's liver function and the complexity of the resection. In cases where the retention rate of ICG is suboptimal, surgeons may consider administering a higher dose or adjusting the timing of administration to improve visualization13.
Additionally, troubleshooting strategies may be necessary if fluorescence visualization is inadequate. If the fluorescence does not clearly delineate the hepatic anatomy, surgeons should ensure that the ICG is administered correctly and that the imaging system is functioning optimally. Intraoperative adjustments, such as modifying the lighting conditions or camera angles, can also improve fluorescence detection. Moreover, if unexpected bleeding occurs, a thorough understanding of the vascular anatomy, as visualized by ICG, allows for rapid identification and management of bleeding vessels10.
Despite its advantages, the use of ICG fluorescence navigation in laparoscopic hepatectomy has limitations. One significant concern is the variability in ICG retention rates, which can be influenced by liver function, vascular integrity, and tumor characteristics14. In patients with compromised liver function, such as those with cirrhosis, the fluorescence signal may be less reliable, potentially leading to inadequate visualization of critical structures.
Additionally, the reliance on fluorescence imaging may lead to overconfidence in intraoperative decision-making, particularly if surgeons neglect traditional anatomical landmarks and rely solely on fluorescence for guidance12. There is also a learning curve associated with the technique, as surgeons must become proficient in interpreting fluorescence images and integrating them into their surgical workflow13.
The integration of ICG fluorescence navigation into laparoscopic anatomical hepatectomy represents a significant advancement over traditional methods. Conventional approaches often lack the real-time feedback that fluorescence imaging provides, which can lead to increased complications such as bleeding or incomplete resections9. By enhancing visualization, ICG fluorescence allows for more precise dissections and greater preservation of healthy tissue, which is crucial for maintaining liver function postoperatively.
Moreover, the Takasaki approach, combined with ICG, offers a systematic method for segmental liver resections that can standardize procedures and improve outcomes across various surgical teams11. This integration of advanced imaging technology not only enhances surgical safety but also aligns with the broader trend towards minimally invasive techniques in hepatobiliary surgery, promoting faster recovery and reduced hospital stays12.
Looking ahead, the application of ICG fluorescence navigation in laparoscopic liver surgery holds promise for further advancements. Future research could focus on optimizing ICG dosing protocols and enhancing imaging technologies to improve visualization in challenging cases, such as those involving cirrhotic livers or complex vascular anatomy14.
Disclosures
The authors declare that they have no conflict of interest.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant No.82100692) and the Science and Technology Program of Guangzhou (Grant No.202201011097).
Materials
| Name | Company | Catalog Number | Comments |
| Indocyanine green for injection | Dandong Yichuang Pharmaceutical Co., Ltd. | H20055881 | |
| Harmonic devices | Affacare Medical (Beijing) Co., Ltd | AH-1200 | |
| Laparoscopic bulldog | B. Braun Aesculap Co.,Ltd | https://catalogs.bbraun.com/en-01/p/PRID00004560/bulldog-clips | |
| Surgical system | Deeper Network Technologies Co., Ltd | https://www.digipmc.com/Product/info/1071 | |
| Ultrasonic scalpels | Affacare Medical (Beijing) Co., Ltd | AH-600 | |
| Ultrasound | ALOKA Co., Ltd | ARIETTA 850 | |
| Veress needle | Hangzhou Kangji Medical Instrument Co.,Ltd. | https://www.kangjimed.com/laparoscopic-instruments-/surgical-needle-or-knife-/veress-needle-.html |
References
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved