Method Article
Transaxillary First Rib Resection for Treatment of the Thoracic Outlet Syndrome
W tym Artykule
Podsumowanie
Here, we present a protocol of the transaxillary resection of the first rib for treatment of thoracic outlet syndrome caused by compression of the brachial plexus, subclavian vein and artery.
Streszczenie
Thoracic outlet syndrome (TOS) is a common disorder that causes a significant loss of productivity. The transaxillary first rib resection (TFRR) protocol has been used for the decompression of trapped neurovascular structures in the TOS. Among the other surgical procedures, the advantage of the TFRR is that it has the smallest rate of recurrence and better cosmetic outcomes. The disadvantage of TFRR is that it provides a narrow, and deep working corridor that makes obtaining vascular control challenging.
Wprowadzenie
The compression of the brachial plexus, subclavian artery or vein in the scalene triangle is clinically known as thoracic outlet syndrome (TOS), first described by Peet et al.1. Thoracic outlet syndrome is subdivided into neurogenic (NTOS), arterial TOS, and venous TOS based on the underlying etiology1. Patients with NTOS (93-95% of TOS cases) present with pain, numbness, and ipsilateral weakness. Patients with venous TOS (3-5%) present with venous thrombosis, and patients with arterial TOS (1-2%) present with arterial thromboembolic event and ischemia. Conservative management of TOS includes medications and physiotherapy and is the first choice for TOS cases. The surgical treatment modalities include decompression procedures and are performed after conservative management has failed2. Decompression techniques include the transaxillary first rib resection (TFRR), supraclavicular first rib resection scalenectomy (SFRRS), scalenectomy (without first rib resection via supraclavicular or transaxillary), and posterior approach first rib resection (PA-FRR)3. The transaxillary first rib resection, a technique described by Roos et al. in 1966, is an effective method for treatment of TOS4,5. The main goal of TFRR is to completely remove the last cervical and first thoracic ribs and to decompress the underlying neurovascular bundle.
Vascular TOS (VTOS) are diagnosed with CT angiography, color duplex USG, and arteriography or venography, whereas the NTOS is diagnosed with X-ray, electrodiagnostic studies (needle electromyelography), color duplex Doppler USG, and cervical MRI. Physiotherapist and psychiatrist consultations should be obtained to exclude other disorders preoperatively.The symptom relief with lidocaine injection to the anterior scalene muscle is also a good indicator for diagnosis and predictor of surgical benefit in NTOS patients6.
Protokół
This study was conducted in accordance with Declaration of Helsinki and local clinical ethics committee (2018/09).
1. Physical Examination
NOTE: The provocative tests for diagnosis of the TOS are depicted in Figure 1.
- For the Adson test (scalene test, Figure 1A), bring the patient’s shoulder to external rotation with slight abduction and a little bit of extension and palpate the radial pulse. Extend the patient’s head backward and rotate toward the tested shoulder. Ask the patient to breathe in and hold their breath.
- Consider the test positive in cases where reproduction of symptoms or abolition of the radial pulse occurs while symptoms resolve with rotating of the head to the controlateral side.
- For the costoclavicular brace test (Figure 1B), bring the patient’s arm to the back, depress and retract over the patients' scapula on the ipsilateral side. Check the pulse. If the radial pulse disappears or symptoms are reproduced, the test is deemed positive.
- For the hyperabduction test (Figure 1C), slightly extend the patient’s arm and palpate the radial artery. Abduct the arm 90-180°. A positive test is a decrease in the pulse of the radial artery from baseline to the new position.
- For the Roos (East) test (Figure 1D), perform the test in either a sitting or standing position. Take the patient’s shoulders to 90° abduction, externally rotate, and flex elbows to 90°. The elbows should be slightly behind the frontal plane. Have the patient open and close his/her hands for 3 minutes.
- Consider the test positive if the patient experiences heaviness, ischemic pain or weakness of the arms or numbness and tingling of the hands. Discoloration of the hands is also meaningful for the test.
NOTE: Surgical treatment is the first option in VTOS cases, whereas surgical treatment is performed in NTOS cases after 3 months of conservative therapy without any improvement in their daily life, work life, and sleep quality.
- Consider the test positive if the patient experiences heaviness, ischemic pain or weakness of the arms or numbness and tingling of the hands. Discoloration of the hands is also meaningful for the test.
2. Preoperative clinical and electrodiagnostic assessment
- For evaluation of the clinical improvement with surgical treatment, make clinical findings in the physical examination, EMG findings, and the QuickDASH (Disability of Arm, Shoulder, and Hand: https://www.hss.edu/physician-files/fufa/Fufa-quickdash-questionnaire.pdf) questionnaire related to symptoms of daily activities and social and psychological preoperative periods.
- Determine the preoperative EMGs by measuring the compound motor action potential (CMAP), sensory nerve action potential (SNAP), and nerve conduction velocity (NCV) and F-wave latency. Make recordings using a commercial EMG/NCV/EP measuring system (e.g., Nihon Kohden Neuropack 2).
3. Transaxillary first rib resection in a stepwise manner
- Perform anesthesia using a standard anesthetic induction protocol which includes 0.6 mg/kg rocuronium bromide, 0.05 mg/kg midazolam and 1-2 µg/kg fentanyl.
- Administer tiopenthal sodium at 6 mg/kg for maintenance.
4. Patient position (Figure 2)
- After placing the patient in the lateral decubitus position, wrap the arm, elevate and hang in a 90° abduction position. If needed, reduce traction every 3-5 minutes to prevent postoperative complication.
- Use a solution of 10% sterile povidone-iodine for topical sterilization. Drape the arm, axilla and chest. Use sterile sheets on to rest of the body to prevent contamination.
5. Reaching the first rib
- Use the surgical instruments are shown in Figure 3 and the Table of Materials.
- Make an incision in a transverse fashion below the axillary hairline extending from the pectoralis muscle anteriorly and the latissimus dorsi muscle posteriorly at a length of 5-7 cm.
- Cross the skin, subcutaneous tissue, and fascia to reach the anterior chest wall.
- Use blunt dissection to reach the first rib.
6. Releasing the first rib from muscles and fascia
- Pierce the fascia overlying the first rib and dissect away the periosteum overlying the superior part of the rib. Bluntly dissect the inferior edge of the rib from surrounding muscles using monopolar cautery and rib raspatory.
- Split the intercostal muscles until the costoclavicular ligament at the sternocostal junction and the angular costa in the posterior costovertebral junction.
- In the superior edge of the first rib, expose the anterior scalene muscle anteriorly and medius scalene muscle posteriorly. Place the curved forceps under the anterior and middle scalene muscles to cut the muscles at the level of their insertion over the first rib, where they are farthest from the neurovascular bundle.
7. Removal of the first rib or the cervical rib
- Start the resection of the first rib at the sternocostal junction anteriorly. First, turn from its superior edge and then the inferior edge to resect it using a rib cutter from the sternum. Ensure that the neurovascular structures are preserved.
- Afterwards, resect the posterior portion of the rib, and disarticulate the part located distally to the angle of rib; hence complete the rib resection.
- After totally freeing the cervical rib from surrounding tissue, resect and disarticulate the rib until the articular surface of the transverse process is seen.
8. Postoperative Period
- In postoperative period, perform a chest X-ray to rule out complications, such as pnomothorax.
- Remove the thorax drain on postoperative day 1 in uneventful cases.
- Use nonsteroidal anti-inflammatory drugs, narcotic analgesics, and a muscle relaxant for postoperative pain.
- In the early postoperative period, examine movement of the arm in the operated side. Continue physical therapy for the first two post-operative months.
- Advise the patient not to perform any exhausting activity with the operated side.
9. Postoperative clinical and electrodiagnostic assessment
- For evaluation of the clinical improvement with surgical treatment, compare clinical findings in the physical examination, EMG findings, and the QuickDASH (Disability of Arm, Shoulder, and Hand: https://www.hss.edu/physician-files/fufa/Fufa-quickdash-questionnaire.pdf) questionnaire related to symptoms of daily activities and social and psychological preoperative and postoperative (3 months) periods.
- Compare the preoperative and postoperative EMGs by measuring the compound motor action potential (CMAP), sensory nerve action potential (SNAP), and nerve conduction velocity (NCV) and F-wave latency. Make recordings using a commercial EMG/NCV/EP measuring system (e.g., Nihon Kohden Neuropack 2).
- Perform the physical examination postoperatively to evaluate the pain and paresthesia.
Wyniki
Clinical Outcomes
A total of 15 patients were included in this study. Three patients (20%) were male and 12 of patients (80%) were female. The mean age of patients was 30.6 ± 8.98 years. All male participants and 5 of female participants were manual laborers. The most common complaint of the NTOS group was arm-forearm pain and numbness weakness of grip and hypothenar atrophy. In the postoperative clinical follow-up, patients were questioned about their paresthesia and pain severity, overall satisfaction, their activity and work status. QuickDASH scores and EMG value were evaluated preoperatively and in the postoperative period. Comparison of preoperative and postoperative EMG measurements are presented in Table 1, Table 2, Figure 4, Figure 5 and Figure 6. We found a remarkable clinical improvement between preop- and postoperative QuickDASH7.
The postoperative exam at six months was evaluated for recurrence or surgical failure. The recurrence rate has been noted to be between 6-54% in different case series8. In the study here, recurrence was observed in 6% of patients (n=1) at the operative side after six months of operation while 20% of patients (n=3) reported TOS symptoms at the controlateral side in follow-up (4 to12 years).
All patients were discharged between postoperative days 2-5. The morbidity rates have been noted to be between 5-40% and include pneumothorax, infection, nerve injury (long thoracic nerve, cervical sympathetic chain, roots of the brachial plexus), hemothorax, hematoma in the surgical field, and lymphatic fluid leakage. These complications are often temporary and resolve within a few days. Deficits lasting longer may require surgical intervention.
Electrodiagnostic outcomes
The latency of the median F-wave was remarkably prolonged on the affected side compared to the unaffected side preoperatively. There was no significant difference in the latency of ulnar F-waves between sides. Compound motor action potential (medial antebrachial cutaneous), sensory nerve action potential (ulnar), and nerve conduction velocity (median motor amplitude) values increased significantly postoperatively. EMG findings are correlated with postoperative clinical improvement7.

Figure 1: Provocative tests for thoracic outlet syndrome. (A) The Adson test. (B) The Costoclavicular brace test. (C) Hyperabduction test. (D) Roos (East test. Please click here to view a larger version of this figure.

Figure 2: Operative position used for patient positioning. Please click here to view a larger version of this figure.

Figure 3: Surgical instruments used for the procedure. Please click here to view a larger version of this figure.
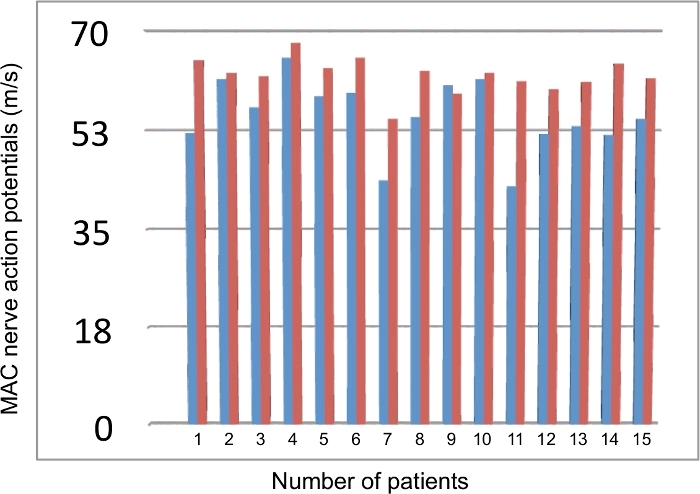
Figure 4: Comparison of preoperative and postoperative values of the medial antebrachial cutaneous (MAC) nerve action potantials on each patient. Blue: preoperative data; Red: postoperative data. Please click here to view a larger version of this figure.
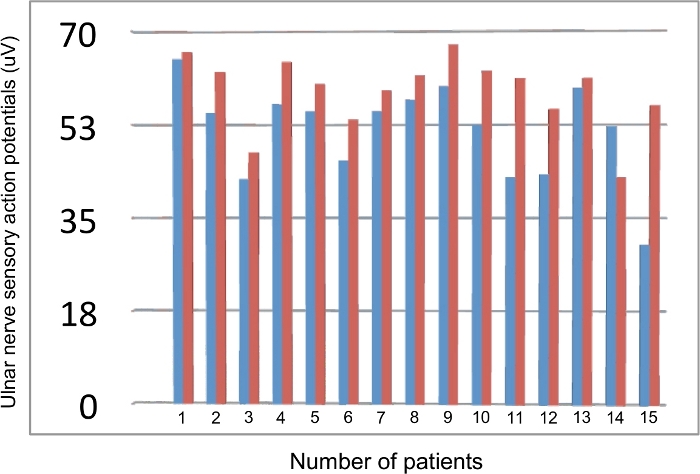
Figure 5: Comparison of preoperative and postoperative values of the ulnar nerve sensory responses on each patient. Blue: preoperative data; Red: postoperative data. Please click here to view a larger version of this figure.
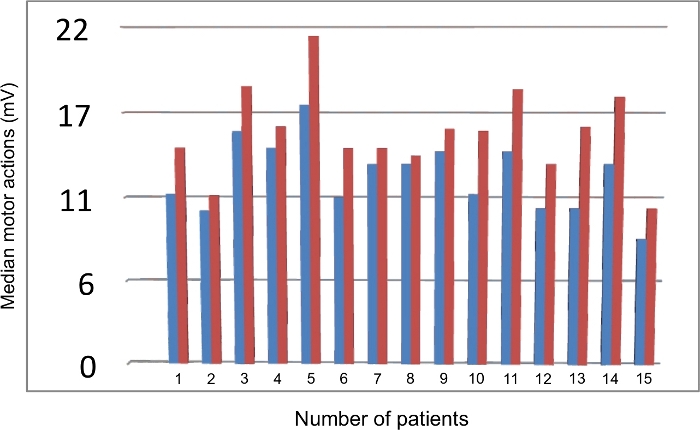
Figure 6: Comparison of preoperative and postoperative values of the median motor actions amplitude responses on each patient. Blue: preoperative data; Red: postoperative data. Please click here to view a larger version of this figure.
| Unaffected Side | Affected Side | p value | |
| Median F Response(ms) | 22.94±1.79 | 23.98±2.05 | 0.015 |
| Ulnar F Response(ms) | 23.57±1.97 | 24.01±2.49 | 0.246 |
| This table has been modified from [7]. | |||
Table 1: Comparison of the median nerve F response and ulnar nerve F response of upper extremities preoperatively.
| Preoperative | Postoperative | p value | |
| MAC(m/s) | 55.1 ± 6.36 | 62.15 ± 3.08 | 0.0001 |
| U-SNAP (µV) | 51.35 ± 8.95 | 58.66 ± 6.8 | 0.003 |
| MMA(mV) | 12.43 ± 2.32 | 15.2 ± 2.82 | 0.0001 |
| MAC: medial antebrachial cutaneous, U-SNAP: ulnar sensory neural action potential, | |||
| MMA: median motor amplitude | |||
| This table has been modified from [7]. | |||
Table 2: Preoperative and postoperative comparisons of the electrophysiological measures.
Video: Transaxillary first rib resection in a stepwise manner. Please click here to download this video.
Dyskusje
TFRR is the most used surgical technique for treatment of TOS9,10,11. The advantage of the TFRR is that it provides a better cosmetic result with a hidden incision in the axilla without requirement of cutting the muscles to reach the surgical field. Its disadvantage is the relatively narrow and deep working space. The supraclavicular approach, which is preferred for arterial TOS treatment, puts the subclavian artery at less risk of damage12. The subclavian vein is followed in the infraclavicular approach commonly used for venous TOS treatment, and the posterolateral FRR is mostly used for the treatment of the recurrent TOS13,14.
A randomized study of the supraclavicular neoplasty of the brachial plexus by Sheeth et al. noted that TFRR provides a better surgical outcome than other surgical techniques15. Another study compared the NTOS cases treated with TFRR, the cases treated with the supraclavicular FRR+scalenectomy, and the cases treated only with scalenectomy, which resulted in clinical improvement rates of 60-92%, 64-86%, and 63-80%, respectively. Although there has not been a significant difference between surgical outcome, lower recurrence rates have been noted in cases treated with TFRR10,16,17,18,19.
The retractor should be used carefully and in an anterior-posterior direction to avoid damage to the neurovascular structures in the narrow field. The scalene triangle has anterior and middle scalene muscles on both side and has the first rib in its basal side. The subclavian artery and brachial plexus passes through the scalene triangle, and scalene vein passes anterior to the anterior scalene muscle, not through the scalene triangle. The first rib is retracted downward, and the middle scalene muscle is cut at its attachment point to the first rib. After the anterior and middle scalene muscles are cut, the fascia and soft tissues along the superior edge of the first rib are freed from the sternum anteriorly to the vertebral body posteriorly. Although not required for this illustrative case, anterior costoclavicular ligament and subclavian muscle division might be needed in some cases. The retraction should be avoided toward the apex of the scalene triangle, where neurovascular structures reside. Intraoperative nerve injury may cause severe disabilities, such as the diaphragm eventration caused by the phrenic nerve injury, winging of the scapula caused by the long thoracic nerve injury, and numbness in the arm caused by the intercostobrachial nerve injury. The inferior edge of the first rib is freed from pleura gently. In case of unintended pleura opening, a chest tube should be placed to prevent the hemothorax or pneumothorax. Since the most common cause of recurrence is leaving a piece of the posterior part of the rib, the first rib should be completely removed. During this procedure, especially posteriorly, there is a risk of injury to the intercostal vein. Oozing from the intercostal veins is stopped by tamponade rather than using the electrocautery, which may damage the brachial plexus causing postoperative causalgia.
Since the surgical corridor in TFRR technique is narrow, hemostasis is crucial to make the working area clean and to prevent postoperative hematoma. During the closure, a hemovac drain can be placed.
In conclusion among surgical treatment modalities used for cases of TOS, the TFRR technique is a unique modality with excellent surgical outcomes and lower recurrence rates. The major limitation of this procedure is that it provides restricted vascular reconstruction options in VTOS cases.
Ujawnienia
None
Podziękowania
None
Materiały
| Name | Company | Catalog Number | Comments |
| Ag Debakey vascular forceps 24 cm, 3.5 mm | Lawton medizintechnik | 30-0032 | Check the hemorrhage |
| Bone chisels curved 13x9.1/2'' | Aesculap Inc. | MB-992R | Dissect the periost of the first rib |
| Doyen-stille retractor 24 cm | Lawton medizintechnik | 20-0650 | Skin- muscle retraction |
| Foerster sponge forceps straight | Lawton medizintechnik | 07-0156 | For swabbing |
| Luer stille bone rongeur curved 27 cm | Lawton medizintechnik | 38-0703 | Bone punches |
| Luer stille rongeur straight 22 cm | Lawton medizintechnik | 38-0400 | Rib cutter |
| Mayo hegar needle holder 20.5 cm | Lawton medizintechnik | 08-0184 | Suturing |
| Metzenbaum scissors curved delicate 23 cm | Lawton medizintechnik | 05-0665 | Dissection |
| Overholt curved forceps delicate 30.5 cm | Lawton medizintechnik | 06-0807 | Split the scalen muscles from the rib |
| Roberts art forceps straight 24 cm | Lawton medizintechnik | 06-0370 | For sponge and remove remain bone |
| Roux retractor medium size 15.5 cm | Lawton medizintechnik | 20-0402 | Wound retraction |
| Semb rasparotry 22,5 cm, 12mm | Lawton medizintechnik | 39-0252 | Dissect the muscle of the first rib |
| Smith peterson model curved osteotome 13x205 mm | Lawton medizintechnik | 46-0783 | Dissect the muscle of the first rib |
| Stille -giertz rib shears 27 cm | Lawton medizintechnik | 38-0200 | First rib cutting |
| Stille osteotome 8x205 mm | Lawton medizintechnik | 46-0248 | Dissect the periost of the first rib |
| Wagner rongeur 5.5x210 mm | Lawton medizintechnik | 53-0703 | Punches |
Odniesienia
- Peet, R. M. Thoracic outlet syndrome: evaluation of a therapeutic exercise program. InProc Mayo Clinic. 31, 281-287 (1956).
- Han, S., et al. Transaxillary approach in thoracic outlet syndrome: the importance of resection of the first-rib. European Journal of Cardio-Thoracic Surgery. 24 (3), 428-433 (2003).
- Yavuzer, &. #. 3. 5. 0. ;., Atinkaya, C., Tokat, O. Clinical predictors of surgical outcome in patients with thoracic outlet syndrome operated on via transaxillary approach. European Journal of Cardio-Thoracic Surgery. 25 (2), 173-178 (2004).
- Roos, D. B. Transaxillary approach for first rib resection to relieve thoracic outlet syndrome. Annals of Surgery. 163 (3), 354 (1966).
- Jubbal, K. T., Zavlin, D., Harris, J. D., Liberman, S. R., Echo, A. Morbidity of First Rib Resection in the Surgical Repair of Thoracic Outlet Syndrome. Hand. , 1558944718760037 (2018).
- Likes, K. C., et al. Lessons learned in the surgical treatment of neurogenic thoracic outlet syndrome over 10 years. Vascular and Endovascular Surgery. 49 (1-2), 8-11 (2015).
- Akkuş, M., Yağmurlu, K., Özarslan, M., Kalani, M. Y. Surgical outcomes of neurogenic thoracic outlet syndrome based on electrodiagnostic tests and QuickDASH scores. Journal of Clinical Neuroscience. 58, 75-78 (2018).
- Peek, J., et al. Long-term functional outcome of surgical treatment for thoracic outlet syndrome. Diagnostics. 8 (1), 7 (2018).
- Sanders, R. J., Annest, S. J. Technique of supraclavicular decompression for neurogenic thoracic outlet syndrome. Journal of Vascular Surgery. 61 (3), 821-825 (2015).
- Sanders, R. J., Hammond, S. L., Rao, N. M. Thoracic outlet syndrome: a review. The Neurologist. 14 (6), 365-373 (2008).
- Vos, C. G., Ünlü, &. #. 1. 9. 9. ;., Voûte, M. T., van de Mortel, R. H., de Vries, J. P. Thoracic outlet syndrome: First rib resection. Shanghai Chest. 1 (1), (2017).
- Desai, S. S., et al. Outcomes of surgical paraclavicular thoracic outlet decompression. Annals of vascular surgery. 28 (2), 457-464 (2014).
- Peek, J., et al. Long-term functional outcome of surgical treatment for thoracic outlet syndrome. Diagnostics. 8 (1), 7 (2018).
- Urschel, H. C. Transaxillary first rib resection for thoracic outlet syndrome. Operative Techniques in Thoracic and Cardiovascular Surgery. 10 (4), 313-317 (2005).
- Sheth, R. N., Campbell, J. N. Surgical treatment of thoracic outlet syndrome: a randomized trial comparing two operations. Journal of Neurosurgery: Spine. 3 (5), 355-363 (2005).
- Urschel, H. C., Razzuk, M. A. Neurovascular compression in the thoracic outlet: changing management over 50 years. Annals of Surgery. 228 (4), 609 (1998).
- Povlsen, B., Hansson, T., Povlsen, S. D. Treatment for thoracic outlet syndrome. Cochrane Database of Systematic Reviews. 11, (2014).
- George, R. S., Milton, R., Chaudhuri, N., Kefaloyannis, E., Papagiannopoulos, K. Totally endoscopic (VATS) first rib resection for thoracic outlet syndrome. The Annals of Thoracic Surgery. 103 (1), 241-245 (2017).
- Strother, E., Margolis, M. Robotic first rib resection. Operative Techniques in Thoracic and Cardiovascular Surgery. 20 (2), 176-188 (2015).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaPrzeglądaj więcej artyków
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone