Method Article
Application of Microwave Ablation in Laparoscopic Partial Splenectomy
요약
The use of laparoscopic partial splenectomy has been limited due to the high risk of bleeding during surgery. Therefore, we introduce a laparoscopic method combined with microwave ablation to solve the problem of intraoperative bleeding.
초록
Splenic hemangioma is the most common pathological classification of splenic tumors, and its surgical indication and treatment have been controversial. Before, open splenectomy was usually used to treat splenic hemangioma. Following the rapid development of laparoscopic techniques, people's requirements for minimally invasive treatment have gradually increased, and laparoscopic splenectomy has gradually become the main treatment method. However, through the deeper study of spleen function, it was found that partial splenectomy can cut down the incidence of postoperative thrombocythemia and decrease side effects on the physiological function of the body, so laparoscopic partial splenectomy came into being. However, due to the special anatomical structure, the incidence of hemorrhage during partial splenectomy is greater. Therefore, during the operation, we removed part of the splenic blood vessels, combined with microwave ablation, which perfectly solved the problem of intraoperative bleeding. Laparoscopic partial splenectomy combined with microwave ablation not only achieves the requirements of minimally invasive treatment but also reduces the risk of intraoperative bleeding, meriting clinical application and promotion.
서문
Benign splenic lesions generally do not require surgical intervention, and regular follow-up is the mainstay. Surgery is indicated when they become larger than 40 mm in diameter or cause clinical symptoms1. For benign splenic mass lesions, total splenectomy is the mainstay of surgery, and laparoscopic total splenectomy (LTS) has long been considered a standard surgical procedure. The advantages of this technique over open surgery are indisputable2. However, total splenectomy can lead to complications such as decreased immunity, venous thrombosis, and infection after overwhelming splenectomy3,4,5, which seriously affects the prognosis of patients. With the in-depth study of spleen function and anatomy, laparoscopic partial splenectomy (LPS), which preserves part of the spleen function, has been widely used in clinical practice6,7, but there is still no consensus on whether LPS is superior to LTS for benign splenic tumors. Because of the fragility of spleen tissue, which makes it much more difficult to suture, LPS has a higher risk of bleeding than LTS8. Therefore, how to reduce intraoperative bleeding is a key issue in the implementation of LPS.
Microwave ablation (MVA) can be used to control life-threatening bleeding by rapidly raising the local temperature of the target tissue above 60 °C. It has been used as a means of hemostasis in a variety of solid tumor needle biopsies and laparoscopic hepatectomy9,10,11,12,13. At present, LPS assisted by MVA is still rarely reported.
In this study, we performed LPS by blocking blood flow in the area where the tumor is located and then using MVA to coagulate the spleen tissue at the plane of the ischemic line, and finally successfully completed the operation. This approach preserves some splenic function and reduces intraoperative blood loss, which decreases the postoperative complication rate after splenectomy.
CASE PRESENTATION:The patient, a 48-year-old woman, complained of left upper quadrant pain for more than 7 years, had a history of hypertension, and denied a history of abdominal surgery. Computed tomography (CT) and contrast-enhanced scan of the upper abdomen in the outer hospital showed that there was a slightly low-density nodule in the spleen, and it was more likely to be considered a hemangioma.
Diagnosis, Assessment, and Plan:
After admission, ultrasound and MRI of the upper abdomen were completed to preliminarily diagnose splenic hemangioma. Considering that the patient's tumor diameter was greater than 5 cm and accompanied by abdominal pain, a partial splenectomy was planned
프로토콜
This protocol meets the norms and requirements of the Medical Ethics Committee of the First Affiliated Hospital of Jinan University, and the informed consent of the patient has been obtained.
1. Preoperative examination
- Determine the location and size of the tumor and blood vessels (Splenic arteriovenous branches) supplying the tumor according to the preoperative CT or MRI, and then plan the resection range and microwave ablation plane. Here, only an MRI was performed before the operation (Figure 1), and it was determined that the tumor was located at the lower pole of the spleen and supplied by the branch of the lower pole of the splenic artery.
- Use the following inclusion criteria: Age 18-75 years; preoperative imaging examination shows a benign occupancy of the spleen, and the diameter of the spleen occupancy mass is ≥ 5 cm, or it is combined with clinical symptoms such as abdominal pain and bloating; the tumor is confined to the upper or lower pole of the spleen and does not involve the splenic arteriovenous vessels.
- Use the following exclusion criteria: A history of blood system-related diseases; spleen lesions caused by other causes (such as portal hypertension, pancreatic disease, malaria, splenic rupture, splenic malignancy, etc.).
2. Anesthesia and preoperative preparation
- Use Endotracheal intubation for general anesthesia. At the same time, perform internal jugular venipuncture to place a 7 Fr intravenous catheter with ultrasound guidance and puncture the radial artery with a 21 G arterial indwelling needle for arterial pressure detection.
- Indwell a 16Fr gastric tube and a 16Fr urinary tube. Administer antibiotics (Latoxef 1 g) 30 min before surgery to prevent infection.
- Let the patient lie down tilted to the right with the head upper than the feet and the lower limbs spread 50°-60°. Adjust the position in time according to the intraoperative situation.
3. Surgical procedure
- Operator position: The first surgeon stands on the patient's right side, while the second is located on the opposite side, and the camera operator stands between the legs (Figure 2).
- Trocar hole layout: Set and maintain a pneumoperitoneum pressure of 12 mmHg. Establish a 10 mm observation hole at the lower umbilical margin using the 5-hole method and implant into it a 30° laparoscope. Establish a 12 mm primary operating hole at the right linea pararectalis umbilicus level, and 5 mm auxiliary operating holes at the right mid-clavicular line below the costal margin, the left anterior axillary line below the costal margin, and left linea pararectalis umbilicus level. Adjust the position of the trocar or increase its number if necessary, during the operation.
NOTE: In the case of the four-hole method, the observation hole is still located at the lower edge of the umbilicus. Establish two 10 mm primary operating holes at the midpoint of the line connecting the xiphoid process to the umbilicus and left anterior axillary line umbilicus level, respectively. Set five 5 mm auxiliary operating holes at the left mid-clavicular line umbilicus level. - Surgical procedures
- Open the left gastrocolic ligament with an ultrasonic knife and separate the gastrosplenic ligament to reveal the splenic portal (Figure 3A). Pay attention to ligating the short gastric arteries while dissecting the gastrosplenic ligament.
- Isolate the lower pole branch of the spleen pedicle and then ligate them with Hem-o-Lok clamps (Figure 3B-C). Dissect the splenic artery to find the branches of the blood vessels supplying the tumor if necessary.
- Reveal the splenic hemangioma (Figure 3D). Separate the splenocolic ligaments (on the lower outer side of the spleen, Figure 3E) and splenorenal ligaments (behind the spleen, Figure 3F) to make the target area fully free.
- Identify the ischemic line between normal spleen tissue and the fraction lacking blood supply (Figure 3G).
- Insert the percutaneous microwave ablation needle and coagulate the spleen tissue by microwave ablation along the ischemic line in phases and gradually, with the power of 60-80 W. Adjust the time according to the specific injection position and depth (Figure 3H-I). The time per ablation is about 3 min. Ensure that the tip of the needle does not penetrate the spleen parenchyma, and that the ablation area is in the same plane.
- Divide the splenic along the coagulation zone (Figure 3J). Check for bleeding in the splenic section and observe the blood supply of the residual spleen (Figure 3K).
- Place the splenic fossa drainage tube (Figure 3L) and remove the splenic tumor specimens from the extended umbilical incision. Use layered sutures to suture the surgical incision, and the surgery is over.
4. Post-surgical procedures
- Perform H&E staining and immunohistochemical (IHC) staining on splenic mass specimens to confirm the diagnosis.
- Recheck the blood sample on the 1st, 3rd, and 7th days after surgery, followed by a weekly blood checkup. Use aspirin if persistently elevated platelets are found. Continue antibiotics for 3 days after surgery to prevent infection. Patients are usually hospitalized for 1-2 weeks after surgery, and re-examination is done using abdominal CT 1 month after surgery.
결과
The lower pole of the splenic, including the tumor, was resected in about 3 h with 100 mL of hemorrhage. The patient recovered without complications such as pancreatic leakage, intestinal leakage, splenic effusion, and portal vein thrombosis.
H&E and CD34 IHC staining was used to determine the postoperative pathology as splenic hemangioma with focal infarction (Figure 4A-C).
After discharge, the patient returned to the hospital for weekly re-examination of blood count, and the peak of platelet was 7.24 x 1011 cells/L at 2 weeks after surgery. Oral aspirin was started to prevent venous thrombosis, and then the platelet count gradually decreased (Table 1). Aspirin was stopped 1 month after the operation when the platelet level returned to normal. Abdominal computed tomography (CT) 1 month after surgery indicated good residual splenic blood circulation (Figure 4D-4F). MRI was not re-examined after surgery due to financial issues.

Figure 1: MRI image. (A-D) A mass with a rich blood supply was found at the sub splenic pole, which was considered a vascular-derived tumor Please click here to view a larger version of this figure.

Figure 2: Trocar placement. Adopt the five-hole method and use the specific punching position shown in the figure. Please click here to view a larger version of this figure.
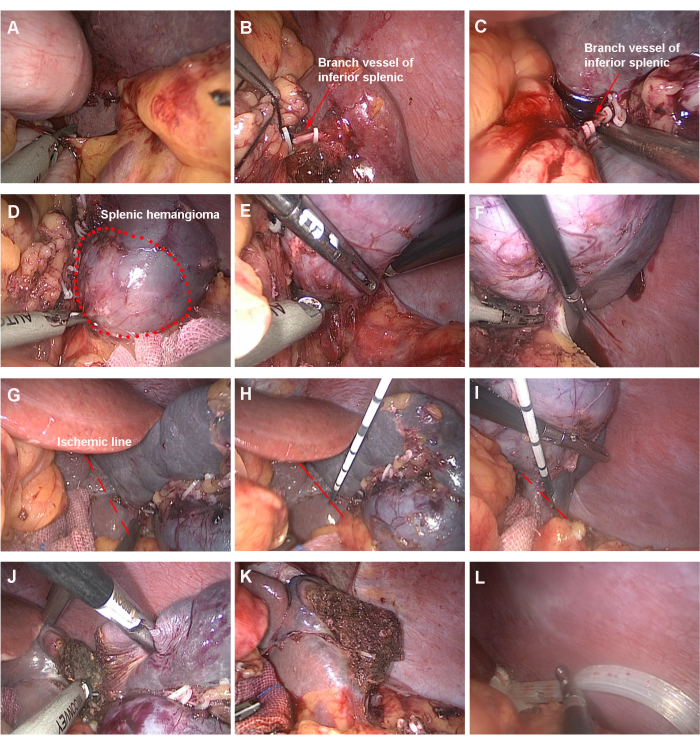
Figure 3: Steps of the surgery. (A) Open the left gastrocolic and gastrosplenic ligaments. (B, C) Dissociate and ligate the lower pole vessels of the spleen. (D) Reveal the hemangioma of the inferior pole of the spleen. (E) Separate the splenocolic ligaments. (F) Separate the ligaments between the spleen and kidney. (G) Observe the ischemic line. (H, I) Start ablation. (J) Sever the spleen. (K) Examine the splenic cross-section and assess the blood supply of the residual splenic. (L) Indwell drainage tube. Please click here to view a larger version of this figure.

Figure 4: Pathological specimen. (A) Image of tumor appearance, scale bars=1 cm. (B) H&E staining image, scale bars=10 µm. (C) CD34 IHC staining image, scale bars=10 µm. (D-F) CT images after surgery. Please click here to view a larger version of this figure.
| Preoperative | 1 day post- operatively | 3 days post- operatively | 7 days post- operatively | 2 weeks post- operatively | 3 weeks post- operatively | 1 month post- operatively | |
| Platelet count (PLT) | 2.61 x 1011 cells/L | 2.74 x 1011 cells/L | 3.51 x 1011 cells/L | 5.02 x 1011 cells/L | 7.24 x 1011 cells/L | 6.13 x 1011 cells/L | 3.35 x 1011 cells/L |
Table 1: Patient platelet count.
토론
The selection of appropriate cases is the first step in the successful development of LPS. Based on personal experience and literature reports, we summarize the following indications14,15: (1) The tumor is located in the upper or lower pole of the spleen and away from the splenic hilum. (2) There is no serious adhesion between the tumor and surrounding tissues. (3) The retained spleen volume should be at least 25% of the original volume. (4) No coagulation dysfunction.
Due to the abundant blood flow to the spleen, a large number of splenic pedicle vessels and parenchymal internal vessels need to be dealt with during the resection, which requires extensive experience in laparoscopic surgery. The risk of LPS is very high, which limits the popularity of this technique. Conventional LPS usually involves exposure of the splenic hilum, followed by ligation of the upper or lower pole arteriovenous vessels where the splenic tumor is located, and severing of the splenic tissue along the ischemic line16,17. Controlling bleeding when the spleen is severed has become a key problem in the development of LPS. A study has found that splenic dissection along the plane 1 cm inside the ischemic line can effectively reduce intraoperative bleeding18. Temporary occlusion of the splenic trunk has been deemed to be a safe, feasible, and repeatable technique in LPS19. Wang et al. performed a bloodless parenchymal splenectomy using a laparoscopic bipolar radiofrequency device20. Radiofrequency ablation is considered to be a safe, simple, and effective technique for reducing intraoperative bleeding in partial splenectomy21,22. In partial splenectomy, thermal ablation to assist hemostasis can minimize blood loss during surgery23. Although there are many ways to control intraoperative bleeding, the effectiveness of these methods needs to be further verified in clinical practice.
Therefore, we recommend a special method of hemostasis, which is to apply MVA to LPS. Compared with radiofrequency ablation, MVA has a higher thermal effect and is often used in the treatment of solid tumors. The application of microwave ablation to assist laparoscopic hepatectomy has been widely reported, but the application of MVA to assist LPS is still rarely mentioned.
With MVA, pre-blockade of the splenic pedicle vessels can be avoided intraoperatively, which reduces ischemia-reperfusion injury to the residual spleen. Intraoperatively, multi-point penetrating ablation in the same plane is used to form a coagulation zone between normal spleen tissue and the ischemic part. Virtually zero bleeding is achieved when the spleen is severed.
Of course, there are certain drawbacks to this technology. It has been reported in the literature that excessive energy is used to stop bleeding, which may result in large areas of necrotic parenchymal tissue margins24. Improper use of ablation needles can lead to thermal damage to surrounding tissues and organs. Therefore, the surgeon must have accumulated extensive experience in MVA techniques in order to perform this procedure successfully.
When using microwave ablation as an adjunct to LPS, the following points should be noted: First, preliminarily plan the ablation route based on CT or MRI prior to surgery; second, control the injection depth according to the size and thickness of the spleen and calculate the time of each ablation to achieve accurate ablation; third, be vigilant when using ablation needle to penetrate the spleen and pay attention to the position of the needle tip to avoid damage to the surrounding tissues at during the operation; finally, needle path ablation is performed while pulling out the ablation needle to avoid needle bleeding.
In conclusion, MVA-assisted LPS is safe and feasible, but further revision of patient inclusion criteria and improvement of ablation techniques are still needed to reduce postoperative complications and improve patient outcomes.
공개
The authors have nothing to disclose.
감사의 말
None
자료
| Name | Company | Catalog Number | Comments |
| 10-mm trocar | Xiamen Surgaid Medical Device Co., LTD | NGCS 100-1-10 | Sterile, ethylene oxide sterilized, disposable |
| 12-mm trocar | Xiamen Surgaid Medical Device Co., LTD | NGCS 100-1-12 | Sterile, ethylene oxide sterilized, disposable |
| 5-mm trocar | Xiamen Surgaid Medical Device Co., LTD | NGCS 100-1-5 | Sterile, ethylene oxide sterilized, disposable |
| Hem-o-lok | America Teleflex Medical Technology Co., LTD | 544240 | Sterile, ethylene oxide sterilized, disposable |
| Pneumoperitoneum needle | Xiamen Surgaid Medical Device Co., LTD | NGCS 100-1 | Sterile, ethylene oxide sterilized, disposable |
| Suction and irrigation tube | Tonglu Hengfeng Medical Device Co., LTD | HF6518.035 | Sterile,dry heat sterilized, reusable |
| Ultrasounic-harmonic scalpel | Chongqing Maikewei Medical Technology Co., LTD | QUHS36S | Sterile, ethylene oxide sterilized, disposable |
| Water-cooled microwave ablation probe(single use) | Nanjing Viking Jiuzhou Medical Device R&D Center | MTC-3CA-II19 | Sterile, ethylene oxide sterilized, disposable |
참고문헌
- Reyes-Jaimes, L., Camacho-Aguilera, J. F. Spontaneous splenic rupture. Case report and literature review. Rev Med Inst Mex Seguro Soc. 61 (4), 523-531 (2023).
- Nyilas, &. #. 1. 9. 3. ;., et al. Laparoscopic splenectomy in our practice at the University of Szeged Department of Surgery. Magy Seb. 75 (2), 200-207 (2022).
- Liu, G., Fan, Y. Feasibility and safety of laparoscopic partial splenectomy: A systematic review. World J Surg. 43 (6), 1505-1518 (2019).
- Theilacker, C., et al. Overwhelming postsplenectomy infection: A prospective multicenter cohort study. Clin Infect Dis. 62 (7), 871-878 (2016).
- Nardo-Marino, A., Brousse, V. Splenectomy in sickle cell disease: do benefits outweigh risks. Haematologica. 108 (4), 954-955 (2023).
- Romboli, A., et al. Laparoscopic partial splenectomy: A critical appraisal of an emerging technique. A review of the first 457 published cases. J Laparoendosc Adv Surg Tech A. 31 (10), 1130-1142 (2021).
- Di Buono, G., et al. Laparoscopic near-total splenectomy. Report of a case. Int J Surg Case Rep. 77s (Suppl), S44-S47 (2020).
- Liao, K. X., et al. Laparoscopic partial splenectomy in the treatment of splenic ectopic pregnancy. Hepatobiliary Surg Nutr. 13 (3), 569-572 (2024).
- Langford, J., Schammel, C. M. G., Bolton, W., Devane, A. M. Microwave ablation to cauterize a bleed after CT-guided lung biopsy. J Vasc Interv Radiol. 33 (11), 1456-1457 (2022).
- Guo, J., Tian, G., Zhao, Q., Jiang, T. Fast hemostasis: a win-win strategy for ultrasound and microwave ablation. Onco Targets Ther. 11, 1395-1402 (2018).
- Rao, Z., et al. Precoagulation with microwave ablation for hepatic parenchymal transection during liver partial resection. Int J Hyperthermia. 36 (1), 146-150 (2019).
- Abdelraouf, A., et al. Initial experience of surgical microwave tissue precoagulation in liver resection for hepatocellular carcinoma in cirrhotic liver. J Egypt Soc Parasitol. 44 (2), 343-350 (2014).
- Sasaki, K., Matsuda, M., Hashimoto, M., Watanabe, G. Liver resection for hepatocellular carcinoma using a microwave tissue coagulator: Experience of 1118 cases. World J Gastroenterol. 21 (36), 10400-10408 (2015).
- Bader-Meunier, B., et al. Long-term evaluation of the beneficial effect of subtotal splenectomy for management of hereditary spherocytosis. Blood. 97 (2), 399-403 (2001).
- de Buys Roessingh, A. S., de Lagausie, P., Rohrlich, P., Berrebi, D., Aigrain, Y. Follow-up of partial splenectomy in children with hereditary spherocytosis. J Pediatr Surg. 37 (10), 1459-1463 (2002).
- Borie, F. Laparoscopic partial splenectomy: Surgical technique. J Visc Surg. 153 (5), 371-376 (2016).
- Di Mauro, D., Fasano, A., Gelsomino, M., Manzelli, A. Laparoscopic partial splenectomy using the harmonic scalpel for parenchymal transection: two case reports and review of the literature. Acta Biomed. 92 (S1), e2021137 (2021).
- de la Villeon, B., et al. Laparoscopic partial splenectomy: a technical tip. Surg Endosc. 29 (1), 94-99 (2015).
- Ouyang, G., et al. Laparoscopic partial splenectomy with temporary occlusion of the trunk of the splenic artery in fifty-one cases: experience at a single center. Surg Endosc. 35 (1), 367-373 (2021).
- Wang, W. D., et al. Partial splenectomy using a laparoscopic bipolar radiofrequency device: a case report. World J Gastroenterol. 21 (11), 3420-3424 (2015).
- Karadayi, K., Turan, M., Sen, M. A new technique for partial splenectomy with radiofrequency technology. Surg Laparosc Endosc Percutan Tech. 21 (5), 358-361 (2011).
- Itamoto, T., Fukuda, S., Tashiro, H., Ohdan, H., Asahara, T. Radiofrequency-assisted partial splenectomy with a new and simple device. Am J Surg. 192 (2), 252-254 (2006).
- Duan, Y. Q., Liang, P. Thermal ablation for partial splenectomy hemostasis, spleen trauma, splenic metastasis and hypersplenism. Hepatogastroenterology. 60 (123), 501-506 (2013).
- Zacharoulis, D., Katsogridakis, E., Hatzitheofilou, C. A case of splenic abscess after radiofrequency ablation. World J Gastroenterol. 12 (26), 4256-4258 (2006).
재인쇄 및 허가
JoVE'article의 텍스트 или 그림을 다시 사용하시려면 허가 살펴보기
허가 살펴보기This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. 판권 소유