Method Article
A Minimally Invasive, Visualized Method for Nasojejunal Tube Placement
* These authors contributed equally
In This Article
Summary
This study introduces a bedside visualized method to improve nasojejunal tube placement in intensive care unit patients, enhancing efficiency and reducing patient discomfort.
Abstract
Malnutrition is a common issue in critically ill patients, often stemming from illness, injury, or surgery. Prolonged fasting leads to intestinal issues, emphasizing the importance of early enteral nutrition, specifically through jejunal nutrition. While enteral nutrition is crucial, complications with current techniques exist. Nasojejunal (NJ) tubes are commonly used, with placement methods categorized as surgical or non-surgical. Non-surgical methods, including endoscopic guidance, have varying success rates, with endoscopic-assisted placement being the most successful but requiring specialized expertise and logistics.
This study introduces a bedside, visualized method for NJ tube placement to enhance success rates and reduce patient discomfort in the intensive care unit (ICU). In this study involving 19 ICU patients, the method achieved an initial success rate of 94.74% with an average insertion time of 11.2 ± 6.4 min. This visualized method demonstrates efficiency and reduces the need for additional imaging, and the introduction of a miniaturized endoscope shows promise, enabling successful intubation at the bedside and minimizing patient discomfort. Adjustments to the guidewire lens and catheter are necessary but pose opportunities for future refinements.
Introduction
Malnutrition frequently manifests as a common complication in critically ill patients, rendering them incapable of consuming or digesting food normally, primarily as a consequence of illness, injury, or surgical interventions1,2,3,4. Between 30% and 60% of hospitalized patients continue to experience malnutrition5. As a result, the provision of early enteral nutrition support is deemed crucial6. The implementation of early jejunal nutrition serves not only to uphold the integrity of gastrointestinal function and safeguard the intestinal mucosal barrier but also contributes to enhanced immunity and a reduction in complications7,8. There exists a consensus asserting the necessity of supplemental nutrition support, with evidence indicating its capacity to enhance outcomes for patients9,10. In such situations, nutrition can be administered through a tube inserted into either the stomach or the small bowel, known as enteral nutrition (EN). Research into the effectiveness of enteral access devices and placement techniques has become more crucial.
Inserting nasogastric (NG) tubes blindly at the bedside is generally successful. Tube feeding can commence once a radiograph confirms the NG tube tip is correctly positioned within the stomach11. However, during critical illness, gastric emptying can be delayed, leading to increased gastric residual volumes (GRVs) during EN delivery12. High GRVs pose a risk of aspiration, prompting healthcare providers to halt EN administration12. As a solution, the nasojejunal (NJ) tube is a commonly employed method for delivering nutrition to critically ill patients. Currently, there exist numerous methods for the placement of NJ tubes, primarily classified as surgical or non-surgical approaches. There are several non-surgical methods for placing a nasojejunal (NJ) tube, including blind insertion, X-ray fluoroscopy with electromagnetic tracing (e.g., Cortrak, ENvue), ultrasound-guided placement, and endoscopic guidance13,14,15,16.
Blind bedside NJ tube placement has been extensively studied, but the success rate of this procedure varies widely, ranging from 17% to 83% in patients17,18. In the absence of guided tube placement, it becomes challenging to know when the NJ tube has successfully passed through the pylorus. Additionally, there is a risk of the catheter mistakenly entering the airway, especially in critical patients who are unconscious. Among the non-surgical methods, endoscopic-assisted tube placement emerges as the most successful, with a success rate ranging from 73.3% to 97.6%14,19,20. Usually, the endoscopic placement of an NJ tube typically necessitates the expertise of a gastroenterologist in an endoscopy room. Additionally, the relatively large diameter of the digestive endoscope can induce significant discomfort for the patient, often mandating the use of general anesthesia.
Furthermore, transferring patients to the gastrointestinal endoscopy room poses a significant logistical challenge, particularly for critically ill patients in the intensive care unit (ICU). These patients frequently exhibit unstable vital signs, including shock and severe respiratory failure. Critically ill patients are at high risk and likely to experience adverse events while being transported21. Various methods for placing NJ tubes using direct endoscopic visualization have been discussed. These methods have reported success rates ranging from 80% to 90% in small studies22,23,24. However, these procedures are often time-consuming, technically challenging, and require a steep learning curve.
Therefore, at our institution, we employ a miniature visualization device to insert the NJ tube in patients at the bedside. This ensures that the tube's tip traverses the pylorus and avoids accidental entry into the airway, all under continuous visual monitoring. Our goal with this method is to offer healthcare professionals, especially those in the ICU, a new approach to enhance the success rate of NJ tube placement in critically ill patients, ultimately minimizing patient discomfort.
Protocol
This study was approved by the Clinical Research Ethics Committee of the People's Hospital of Anji County. All procedures were carried out in accordance with institutionally approved protocols and with the informed consent of the patients.
1. Patient selection and preparation
- Choose patients based on the following inclusion and exclusion criteria.
- Set the inclusion criteria as patients with acute gastrointestinal dysfunction; those undergoing mechanical ventilation, with impaired consciousness or in a comatose state; those experiencing difficulty in swallowing or chewing; individuals unable to tolerate gastric feeding or experiencing gastric retention; patients with pancreatitis, a hypermetabolic state, or malnutrition; individuals prone to reflux, such as those with traumatic brain injury, undergoing chemotherapy for tumors, etc; patients with inflammatory bowel disease, gastroesophageal fistula, or short bowel syndrome; individuals with other conditions, including patients who have undergone oral, pharyngeal, or esophageal surgery; and age greater than 18 years.
- Set the exclusion criteria to be upper gastrointestinal bleeding; pyloric edema or obstruction; paralytic or mechanical intestinal obstruction; intestinal perforation, necrosis, or absorption disorders; history of gastrointestinal surgery; severe stress state or shock; esophageal stricture or cardia stenosis or obstruction; and other conditions, such as severe esophagogastric fundal varices, nasal obstruction, acute or chronic sinusitis, etc.
- Preoperative assessment
- Before the procedure, assess the patient's nutritional status, consciousness, overall condition, swallowing function, oral and nasal conditions, gastrointestinal function, and cooperation level.
- To follow this protocol, use the Nutrition Risk in the Critically Ill (NUTRIC) scoring system specifically developed for ICU patients as the primary nutritional risk assessment tool25. The NUTRIC score includes the following parameters: age, Acute Physiology and Chronic Health Evaluation (APACHE) II26, Sequential Organ Failure Assessment (SOFA) score26, number of comorbidities, days from hospital admission to ICU admission, interleukin-6 levels (if available). The total NUTRIC score ranges from 0 to 10, with higher scores indicating greater nutritional risk. Scores of 0-4 signify low nutritional risk, while scores of 5-9 denote high nutritional risk.
NOTE: For detailed information on the NUTRIC scoring system, as well as the APACHE II and SOFA scores, please refer to Supplemental Table S1.
- To follow this protocol, use the Nutrition Risk in the Critically Ill (NUTRIC) scoring system specifically developed for ICU patients as the primary nutritional risk assessment tool25. The NUTRIC score includes the following parameters: age, Acute Physiology and Chronic Health Evaluation (APACHE) II26, Sequential Organ Failure Assessment (SOFA) score26, number of comorbidities, days from hospital admission to ICU admission, interleukin-6 levels (if available). The total NUTRIC score ranges from 0 to 10, with higher scores indicating greater nutritional risk. Scores of 0-4 signify low nutritional risk, while scores of 5-9 denote high nutritional risk.
- Prior to their participation, explain the purpose, risks, benefits, and rights of individuals as study participants to the patients. Obtain informed consent from potential participants or their families and document it in writing. Ensure the patient's willingness to cooperate during the procedure.
- Utilize the NUTRIC Nutrition Scoring Table25 (specifically designed for critically ill patients) to evaluate the patient's nutritional status.
- Implement preoperative fasting for 6-8 h, with the option of gastrointestinal decompression.
- Before the procedure, assess the patient's nutritional status, consciousness, overall condition, swallowing function, oral and nasal conditions, gastrointestinal function, and cooperation level.
- Preparation of items
- Examine the portable visualization NJ tube placement main unit for functionality (Figure 1), check the integrity and expiration date of the disposable visualization NJ tube packaging, prepare metoclopramide hydrochloride injection, 2% lidocaine gel, and sterile liquid paraffin oil as per doctor's instructions, obtain sterile towels, syringes, saline solution, gloves, and adhesive tape.
NOTE: For detailed information on the preparation of items, refer to Supplemental File 1.
- Examine the portable visualization NJ tube placement main unit for functionality (Figure 1), check the integrity and expiration date of the disposable visualization NJ tube packaging, prepare metoclopramide hydrochloride injection, 2% lidocaine gel, and sterile liquid paraffin oil as per doctor's instructions, obtain sterile towels, syringes, saline solution, gloves, and adhesive tape.
2. NJ tube placement procedure
- Before the tube placement procedure, double-check the patient's name, hospital number, and the procedure name to ensure accuracy.
- Connect the power supply (220 V, 60 Hz) to the visualized NJ tube placement main unit and turn it on by pressing the START button.
- Open the packaging of the visualization NJ tube and immerse the tube in a sterile treatment bend. Rinse the tube lumen with 2 x 20 mL of sterile saline solution.
- Insert the guide wire endoscope into the NJ tube's cavity, connect the balloon and water sac, and adjust the visual lens for proper visualization. Apply sterile liquid paraffin to the exterior of the NJ tube to ensure proper lubrication.
- If the patient is conscious, apply an appropriate amount of 2% lidocaine gel to a cotton swab and then apply it to the patient's nasal mucosa to achieve surface anesthesia.
- Position the patient in a supine position with the bed elevated at a 30-45° angle (Figure 2A).
- Insert the tube through the patient's nostril, under visual observation, slowly advancing the tube approximately 1-2 cm at a time (Figure 2A). When the tip of the tube reaches the oropharynx, if the patient is conscious, instruct them to swallow voluntarily. For conscious coma patients, tilt the head and chin down to straighten the cervical spine and facilitate entry into the esophagus. Continuously observe visually to avoid misplacement into the trachea.
NOTE: Pay attention to the patency of the patient's nasal passages. If difficulties arise due to issues such as deviated nasal septum, attempting the opposite nostril is recommended. - Take care to notice any resistance while slowly advancing the tube towards the esophagus to avoid potential damage to the esophageal mucosa. Once in the esophagus, observe the pale pink mucosa with longitudinal folds.
- During passage through the narrow points of the esophagus, employ dynamic visual observation by gently rotating the tube for insertion. Refrain from forceful actions, carefully navigate through the three narrow points, inject air or saline as needed, and ensure the cleanliness of the guide wire lens at the front end of the visualized NJ tube for a clear image.
NOTE: There are three narrow points in the normal esophagus. The first narrowing is at the beginning of the esophagus, the second where it crosses behind the left main bronchus, and the third at the esophageal hiatus where it passes through the diaphragm. The mucosa of the normal esophagus is moist, smooth, and pink, while the lower esophageal mucosa is slightly light gray. There are 7-10 vertical folds on the mucous membrane, and the cavity appears convex. - Continue to slowly advance the tube under visual observation with the patient's respiratory movements, approximately 1-2 cm at a time.
- As the tube passes through the gastroesophageal junction (the Z-line) and enters the gastric cavity, observe the dark pink gastric mucosa and peristalsis. The mucous membrane surface typically exhibits irregular wrinkles and depressions (Figure 2B).
NOTE: The gastroesophageal junction (the Z-line) is an anatomical point that delineates the shift from the esophageal mucosa to the gastric mucosa. Under endoscopic observation, one can see the transition from a pale pink or pinkish esophageal mucosa to a darker red or orange-yellow gastric mucosa. The presence of a significant amount of gastric content may affect tube placement. It is recommended to enforce a preoperative fasting period of 6-8 h and consider continuous gastrointestinal decompression before the procedure. - If the view inside the stomach appears unclear, inject saline (10-20 mL each time) into the NJ tube to remove any obstructions covering the front-end guide wire lens.
- If the tube curls or bends inside the stomach, retract the NJ tube to a length of 55-65 cm and gently withdraw while simultaneously advancing the visualized guide wire until it moves smoothly.
NOTE: We detect curling during the procedure by meticulously observing the trajectory and movement of the tube using real-time visualization techniques, such as retroflex view, to detect coiling. This involves monitoring the tube's progress through the gastrointestinal tract and noting any deviations or looping that may indicate curling. If necessary, we can also confirm the presence of curling through abdominal X-rays. - Under continuous dynamic visual observation, slowly continue tube insertion, adapting to gastric peristalsis, and search for the pylorus.
- If the pylorus is not found, temporarily withdraw the visualized endoscope guide wire and adjust the length of the NJ tube to 55-65 cm. Assist the patient into a right lateral position, inject approximately 100-200 mL of saline/air, and reinsert the visualized endoscope guide wire. Identify the position through the gastrointestinal mucosa, make appropriate adjustments, and insert slowly.
- Once the pylorus is confirmed, rotate the handle to adjust the tube's orientation and facilitate its passage through the pylorus with greater precision. Ensure continuous observation of the tube's position and direction during slow advancement, making necessary adjustments as needed for optimal navigation.
- After the tube passes through the pylorus and enters the duodenum, observe the typical finger-like villi of the duodenal mucosa (Figure 2C). Gently rotate and partially retract the visualized endoscope guide wire, simultaneously instilling water (approximately 20 mL) while advancing the tube (to prevent kinking), and slowly insert.
NOTE: The water instillation method facilitates intestinal emptying, obtaining a clear image. Identify the position through the duodenal mucosa to prevent mucosal damage. - Continue inserting the catheter slowly, progressing through the duodenal bulb, descending, transverse, and ascending portions of the duodenum in sequence. Position the tube head inside the jejunum.
- After tube placement is complete, slowly retract the guide wire lens.
- Other methods for verifying tube placement
- Aspirate digestive fluid using a syringe, observe the color and volume, and measure the pH value. If the tube tip is in the intestinal lumen, expect <10 mL of fluid with a golden yellow color and a pH > 7.0. If the tube tip is in the stomach, expect >20 mL of fluid, which may appear light green, clear, colorless, or brown, with a pH < 5.0.
NOTE: This method is not essential during the placement process. Additionally, the pH of the aspirated fluid may be influenced by factors such as medications or nutritional solutions. - Perform a vacuum test by injecting air smoothly, and aspirate to create negative pressure. Injecting 10 mL of air and aspirating <5 mL suggests that the tube has passed through the pylorus.
NOTE: The tip's contact with the wall may affect results. - Abdominal X-ray: Have the patient lie flat and take an X-ray at the bedside. If the X-ray reveals the tube's course in an anti-clockwise "C" shape, the tube tip is in the duodenal cavity.
- Aspirate digestive fluid using a syringe, observe the color and volume, and measure the pH value. If the tube tip is in the intestinal lumen, expect <10 mL of fluid with a golden yellow color and a pH > 7.0. If the tube tip is in the stomach, expect >20 mL of fluid, which may appear light green, clear, colorless, or brown, with a pH < 5.0.
- Tube fixation
- When the patient's nasal skin is intact, use the zigzag method with a high-lift platform. When there is skin damage on the nasal skin, perform the butterfly fixation method with a high-lift platform.
NOTE: For detailed information on the tube fixation and nursing care details for the NJ tube, refer to Supplemental File 1.
- When the patient's nasal skin is intact, use the zigzag method with a high-lift platform. When there is skin damage on the nasal skin, perform the butterfly fixation method with a high-lift platform.
Results
Clinical outcomes
In this study, a total of 19 critically ill patients in the ICU underwent NJ tube placement under visualization guidance. Among the study subjects, there were 12 males (63.16%) and 7 females (36.84%), with an average age of 64.47 ± 13.43 years. Diagnoses included severe pneumonia (n = 6, 31.58%), sepsis (n = 1, 5.26%), successful cardiac arrest resuscitation (n = 1, 5.26%), acute pancreatitis (n = 1, 5.26%), acute exacerbation of chronic obstructive pulmonary disease (n = 3, 15.79%), cerebellar atrophy (n = 1, 5.26%), cerebral hemorrhage (n = 4, 21.05%), cerebral infarction (n = 1, 5.26%), traumatic brain injury (without skull base fracture) (n = 1, 5.26%), altered consciousness (n = 15, 78.95%), and patients requiring invasive mechanical ventilation (n = 18, 94.74%) (Table 1). The NUTRIC scores of these patients upon ICU admission was 6.68 ± 1.11 (Table 1). All these patients presented with acute gastrointestinal dysfunction, accompanied by a high risk of gastroesophageal reflux and aspiration.
By employing the aforementioned method, the success rate of tube placement reached 100%. Specifically, the initial success rate of the first tube insertion was 94.74%, with one instance of successful second tube placement. The average insertion time was 11.21 ± 6.44 min (Table 2). The most common long-term complications were accidental tube removals14. After an accidental tube pull during the use of the NJ tube or if there were suspicions of tube coiling inside the stomach during placement, we confirm the tube's tip position through abdominal X-rays. In five patients, the positioning of the tube tip in the descending section of the duodenum was confirmed through abdominal X-rays (Figure 3), while the remaining cases were confirmed under direct visualization. Complications included minor gastrointestinal bleeding (1 case, with no visible blood in stool, no hematemesis, and a positive occult blood test in gastric fluid, Table 2). There were no cases of gastrointestinal perforation and no instances of accidental entry into the airway (Table 2).
In patients undergoing minimally invasive visualized tube placement, there was a mild increase in heart rate (HR) and respiratory rate (R) during the tube placement process compared to pre-placement levels (P < 0.05, Table 3). The mean arterial pressure (MAP) showed a mild increase with no statistical difference (P > 0.05, Table 3). After 2 weeks of enteral nutrition support, these patients exhibited a significant elevation in serum albumin and prealbumin levels compared to pre-placement values (P < 0.05, Table 3), demonstrating a statistically significant difference. Following nutritional support and other comprehensive treatment measures, patients experienced a significant decrease in APACHE II and SOFA scores26 compared to their ICU admission values, indicating a statistically significant difference (P < 0.05, Table 3). The average length of hospital stay for these patients was 34.74 ± 20.38 days, as presented in Table 2.
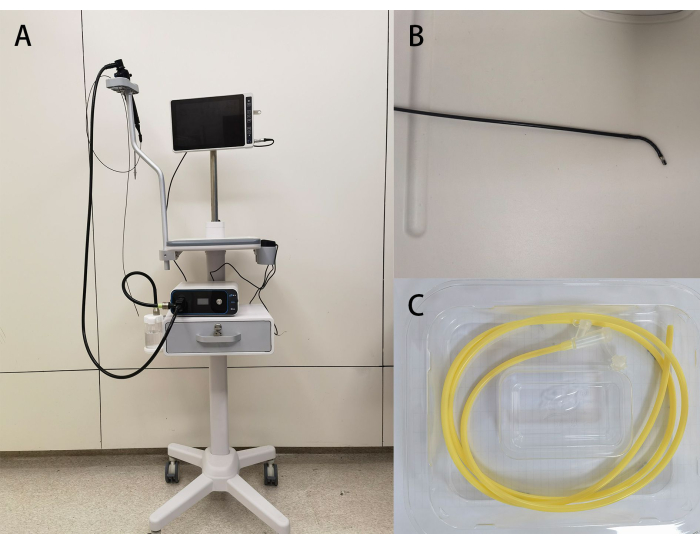
Figure 1: Device images. (A) An overview of the medical endoscope image processor; (B) the steering capability of the guide wire endoscope; (C) the accompanying single-use nasojejunal tube. Please click here to view a larger version of this figure.

Figure 2: Placement of the nasojejunal tube. (A) The procedure during operation; (B) the endoscopic image of gastric mucosa captured by the guide wire endoscope; (C) the endoscopic image of small intestinal mucosa captured by the guide wire endoscope, revealing the presence of small intestinal villi. Please click here to view a larger version of this figure.

Figure 3: Abdominal X-ray image. The NJ tube tip is positioned in the descending section of the duodenum, with a coiled portion of the tube in the stomach. Please click here to view a larger version of this figure.
| N=19, (mean value ± SD) | |
| Characteristic | |
| Age (mean value ± SD) | 64.47±13.43 |
| Sex no. (%) | |
| Male | 12 (63.16) |
| Female | 7 (36.84) |
| Diseases no. (%) | |
| Severe pneumonia | 6 (31.58) |
| Sepsis | 1 (5.26) |
| AECOPD | 3 (15.79) |
| Successful cardiac arrest resuscitation | 1 (5.26) |
| Cerebellar atrophy | 1 (5.26) |
| Cerebral hemorrhage | 4 (21.05) |
| Cerebral infarction | 1 (5.26) |
| Traumatic brain injury (without skull base fracture) | 1 (5.26) |
| Altered consciousness | 15 (78.95) |
| Patients requiring invasive mechanical ventilation | 18 (94.74) |
| Consciousness state no. (%) | |
| Coma | 15 (78.95) |
| Conscious | 4 (21.05) |
| NUTRIC score# | 6.68±1.11 |
Table 1: Demographic and clinical characteristics of the patients at baseline. #NUTRIC score is only assessed on admission to the ICU. Abbreviations: AECOPD = acute exacerbation of chronic obstructive pulmonary disease, NUTRIC score = The Nutritional Risk Score for Critical Illness, hospital stay (days) = the sum of the time spent in ICU monitoring treatment plus the time spent in the general ward after leaving the ICU, SD = standard deviation; mean value ±standard deviation.
| N=19, (mean value ± SD) | |
| Average insertion time (min) | 11.21 ± 6.44 |
| Success rate of initial tube placements no. (%) | 18 (94.74) |
| The position of the NJ tube tip no. (%) | |
| Duodenal bulb | 1 (5.26) |
| Descending portion of the duodenum | 3 (15.79) |
| Transerse portion of the duodenum | 2 (10.53) |
| Ascending portion of the duodenum | 5 (26.32) |
| Upper portion of the jejunum | 8 (42.10) |
| *X-rays no. (%) | 5 (26.32) |
| Bleed no. (%) | 1 (5.26) |
| Gaslrointestinal perforation no. (%) | 0 (0) |
| Cases of accidental entry into the airway no. (%) | 0 (0) |
| Hospital stay (Days) | 34.74 ± 20.38 |
Table 2: Success rate of initial tube placements, average insertion time, complication rate, and hospital stay. *X-rays Number of patients in whom the position of the tip of the NJ tube was confirmed by an abdominal radiograph. Abbreviations: Hospital stay (days) = the sum of the time spent in ICU monitoring treatment plus the time spent in the general ward after leaving the ICU, SD = standard deviation; mean value ±standard deviation.
| Before catheterization | During catheterization | P-value | |
| (n=19) | (n=19) | ||
| (mean value ±SD) | (mean value ±SD) | ||
| MAP (mmHg) | 93.37±15.96 | 96.39±11.67 | 0.288 |
| HR (bpm) | 83.11±15.61 | 92.21±14.92 | 0.000 |
| R (bpm) | 17.32±3.77 | 19.53±3.45 | 0.009 |
| Before catheterization | After catheterization | ||
| ALB (g/L) | 27.10±5.05* | 34.51±5.08** | 0.000 |
| Prealbumin (mg/L) | 135.38±52.80* | 208.69±47.85** | 0.000 |
| APACHE II score | 20.26±5.05* | 10.84±4.15*** | 0.000 |
| SOFA score | 9.53±4.11* | 2.47±2.72*** | 0.000 |
Table 3: Vital signs, APACHE II and SOFA scores, and laboratory results. *Upon admission to the ICU. **Enteral nutrition therapy at 2 weeks. ***Upon transfer out of the ICU. Heart rate, respiratory rate, mean arterial pressure, APACHE II and SOFA scores, serum albumin, and serum prealbumin were subjected to statistical analysis using paired-sample t-tests. The normal range for serum albumin is 40-55 g/L, and the normal range for serum prealbumin is 200-430 mg/L. Abbreviations: HR = heart rate, R = respiratory rate, MAP = mean arterial pressure. APACHE II score = acute physiology and chronic health status II score, SOFA score = sequential organ failure score, SD = standard deviation.
Supplemental File 1: NJ Tube's nursing care. The detailed information on the nursing care for the NJ Tube. Please click here to download this File.
Supplemental Table S1: The NUTRIC scoring system, the APACHE II and SOFA scores. Please click here to download this File.
Discussion
We utilized a small visualization tool to insert NJ tubes at the patient's bedside. By employing visualization methods and adjusting patient positioning, we achieved a 94.47% success rate for the initial tube placement. The average time for inserting the tube was just 11.21 ± 6.44 min (Table 2). One patient initially failed intubation but was successfully intubated after receiving a 10 mg intramuscular injection of metoclopramide 20 min before their second attempt (Table 2).
In recent years, numerous studies have demonstrated the application of various methods and techniques in enteral nutrition support. Some studies have discussed the applicability and effectiveness of different types of tubes in specific contexts, such as nasogastric tubes, NJ tubes, and gastric fistula tubes27,28,29. Due to the frequent occurrence of gastric functional impairment in ICU patients, leading to a high risk of gastroesophageal reflux and aspiration, there is an increased likelihood of developing aspiration pneumonia and worsening respiratory failure. Therefore, for patients without contraindications to enteral nutrition, an NJ tube may be the preferred option. However, effectively positioning the NJ tube in an accurate location presents a difficulty for clinical healthcare providers.
Recent advancements have introduced techniques such as ultrasound-guided, magnetic-guided, percutaneous puncture-guided, and endoscopic-guided methods to enhance the precision and safety of enteral nutrition tube placement16,29,30,31. Magnetic tip guidance is employed for NJ tube placement, utilizing a magnetic-tipped guidewire to navigate the tube through the gastrointestinal tract into the small intestine15. However, its universal applicability is limited due to the requirement for magnetic imaging equipment, which is not available in all medical facilities. The presence of magnetic objects near the patient can also interfere with accurate tube placement32. Bedside ultrasound is valuable for NJ tube confirmation33. However, challenges may arise in patients with anatomical variations or obesity, affecting accurate tube tip visualization. Gastric contents or air in the gastrointestinal tract can hinder ultrasound accuracy, complicating tube placement confirmation34.
Whether the NJ tube is guided by a magnetic head or positioned with ultrasound localization, navigating through the pylorus swiftly and accurately remains a challenge. This process still demands an experienced, highly skilled, and patient operating physician. Successful placement typically entails a considerable amount of time, and in the case of patients with intricate anatomy, achieving successful placement may prove particularly challenging. Additionally, supplementary radiographic examinations such as bedside X-rays may still be necessary to precisely determine the specific location of the tube tip, such as its presence in the small intestine. If the tube tip is not in the small intestine or is positioned too deeply, repositioning or adjusting the tube tip is required, often necessitating repeated radiographic examinations. This exposes the patient to multiple X-ray exposures, contributing to increased healthcare costs. In this study, direct visualization of the small intestinal mucosa through the endoscope allowed for the immediate confirmation of the tube tip's location. After an accidental tube pull during the use of the NJ tube or if there were suspicions of tube coiling inside the stomach during placement, we validated the tube tip's position further through bedside abdominal X-ray examinations in a subset of patients (n = 5, Table 2). Consequently, the NJ tubes placed using the visual method in this study eliminated the need for additional imaging examinations.
Endoscopy-guided NJ tube placement is an advanced procedure utilizing an endoscope to guide the tube into the small intestine35. This method is generally reserved for patients with challenging or complex anatomy or those who have experienced previous unsuccessful attempts at NJ tube placement. Nevertheless, the digestive endoscope has a larger diameter and can only be introduced through the mouth, potentially causing increased discomfort for the patient. The endoscopically guided placement of an NJ tube is frequently a more time-consuming procedure compared to standard gastroscopy. In certain instances, it may necessitate general anesthesia for the entire placement process. In this study, the utilization of a miniaturized endoscope, featuring an integrated guidewire and lens with an overall diameter of only 2 mm, facilitated transnasal access, contributing to a reduction in patient discomfort. During the placement process, there was a mild increase in the patient's heart rate and respiratory rate, with a slight, statistically insignificant increase in average arterial pressure (P > 0.05, Table 3). Furthermore, all patients in this study were successfully intubated at the bedside, eliminating the need to transfer critically ill patients and mitigating associated risks.
Similar to conventional endoscopes, the mini-endoscope utilized in this study features a steering function. This design facilitates the successful placement of NJ tubes, even in patients with complex anatomy. The "through-the-scope" method involves passing a small feeding tube (7F or 10F) through the biopsy channel of the endoscope into the jejunum following which the endoscope is withdrawn and the tube is left in place. The procedure is completed after transferring the tube from oral to nasal access. Bosco et al.36 reported a 90% success rate with this technique, with an average procedure time of 19 min. However, this method has limitations. Only small-diameter tubes can fit into the biopsy channel. In addition to the requirement of a therapeutic upper endoscope to pass the 10F "through-the-scope" NJ tube, an oral-nasal transfer must also be done. In this study, we were able to insert a 14F NJ tube. The larger diameter of the NJ tube allows for a greater variety of nutritional fluids to be used in clinical applications, while also reducing the risk of blockage.
The percutaneous endoscopic gastrostomy tube with jejunal extension (PEG-J) is a method utilized to deliver enteral feedings to patients incapable of tolerating oral or gastric feeds37. While effective in delivering enteral nutrition, the PEG-J technique has drawbacks that need attention. Inserting a PEG-J tube demands a considerable level of expertise and experience, and it is an invasive procedure that may not be suitable for all patients38. Moreover, the placement process is protracted. Our method, in contrast, was efficiently completed with a relatively short duration and minimal trauma, making it particularly suitable for conscious patients. Furthermore, no evidence of gastrointestinal perforation and no instances of accidental entry into the airway were detected in any study subjects. There was only one case with a minor occurrence of gastric bleeding (Table 2).
In this study, following enteral nutrition support therapy and other comprehensive management treatments, the APACHE II and SOFA scores of these critically ill patients significantly decreased compared to their scores upon ICU admission (Table 3). The average length of hospital stay was 34.74 ± 20.38 days, as presented in Table 2. This demonstrates that the visualization-guided tube placement method allows for early initiation of enteral nutrition support therapy, thereby improving the patient's condition and prognosis.
Nevertheless, it is important to acknowledge the limitations of this study, specifically, to obtain a clear image with the guidewire lens of the microendoscope, it is imperative that the head end of the NJ tube remains open. Consequently, adjustments to the position of the guidewire lens head end and the catheter are necessary before initiating tube placement. This adjustment is essential to prevent the guidewire lens head end from surpassing the catheter, thus mitigating the risk of gastrointestinal mucosal injury, bleeding, and perforation. In future studies, we plan to enhance the design of guidewire lenses and NJ tubes to improve image clarity and mitigate associated risks.
In summary, the described method is straightforward, secure, and efficient, making it conducive to rapid implementation at the bedside, particularly suitable for critically ill patients in the ICU. This visualized method offers a promising alternative for NJ tube placement in critically ill ICU patients, improving success rates and minimizing patient discomfort. Further refinements in design and additional studies are needed to optimize the technique and address potential limitations.
Disclosures
The authors declare no conflict of interest.
Acknowledgements
The study was supported by various colleagues from the hospital's Department of Critical Care Medicine and Department of Orthopedics. This research received external funding from the Zhejiang Province Medical and Health Science and Technology Program (2019RC170) and the General scientific research project of the Zhejiang Provincial Department of Education (Y201941857).
Materials
| Name | Company | Catalog Number | Comments |
| Disposable nasogastrointestinal tube | JiangSu Jianzhiyuan Medical Instrument Technology Co., Ltd. | W -4.7-1400mm -4.7-1400mm | The outer diameter of the guide tube is 4.7 mm. |
| Lidocaine Hydrochloride Gel | Manufacturers are not limited | For local anaesthesia | |
| Medical Endoscopy Image Processor | JiangSu Jianzhiyuan Medical Instrument Technology Co., Ltd. | HD1080 | The diameter of the guide wire lens is 2 mm. |
| Metoclopramide Dihydrochloride Injection | Manufacturers are not limited | Promote gastric motility | |
| SPSS 20.0 software | International Business Machines Corporation | Statistical analysis | |
| Sterile liquid paraffin oil | Manufacturers are not limited | For catheter lubrication |
References
- van Zanten, A. R. H., De Waele, E., Wischmeyer, P. E. Nutrition therapy and critical illness: practical guidance for the ICU, post-ICU, and long-term convalescence phases. Crit Care. 23 (1), 368 (2019).
- Lambell, K. J., Tatucu-Babet, O. A., Chapple, L. A., Gantner, D., Ridley, E. J. Nutrition therapy in critical illness: a review of the literature for clinicians. Crit Care. 24 (1), 35 (2020).
- Zaher, S. Nutrition and the gut microbiome during critical illness: A new insight of nutritional therapy. Saudi J Gastroenterol. 26 (6), 290-298 (2020).
- Ozdemir, U., Yildiz, S., Aygencel, G., Turkoglu, M. Ultrasonography-guided post-pyloric feeding tube insertion in medical intensive care unit patients. J Clin Monit Comput. 36 (2), 451-459 (2022).
- de-Aguilar-Nascimento, J. E., et al. ACERTO guidelines of perioperative nutritional interventions in elective general surgery. Rev Col Bras Cir. 44 (6), 633-648 (2017).
- Jia, Z. Y., et al. Screening of nutritional risk and nutritional support in general surgery patients: a survey from Shanghai, China. Int Surg. 100 (5), 841-848 (2015).
- Wan, B., Fu, H., Yin, J. Early jejunal feeding by bedside placement of a nasointestinal tube significantly improves nutritional status and reduces complications in critically ill patients versus enteral nutrition by a nasogastric tube. Asia Pac J Clin Nutr. 24 (1), 51-57 (2015).
- Jiang, W., et al. Early enteral nutrition in neonates with partial gastrectomy: a multi-center study. Asia Pac J Clin Nutr. 25 (1), 46-52 (2016).
- McClave, S. A., et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N). JPEN J Parenter Enteral Nutr. 40 (2), 159-211 (2016).
- Corrigan, M. L., Bobo, E., Rollins, C., Mogensen, K. M. Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: Revised 2021 standards of practice and standards of professional performance for registered dietitian nutritionists (competent, proficient, and expert) in nutrition support. Nutr Clin Pract. 36 (6), 1126-1143 (2021).
- Caulfield, K. A., Page, C. P., Pestana, C. Technique for intraduodenal placement of transnasal enteral feeding catheters. Nutrition in Clinical Practice. 6 (1), 23-26 (1991).
- Blaser, A. R., Starkopf, J., Kirsimagi, U., Deane, A. M. Definition, prevalence, and outcome of feeding intolerance in intensive care: a systematic review and meta-analysis. Acta Anaesthesiol Scand. 58 (8), 914-922 (2014).
- Lai, C. W., Barlow, R., Barnes, M., Hawthorne, A. B. Bedside placement of nasojejunal tubes: a randomised-controlled trial of spiral- vs straight-ended tubes. Clin Nutr. 22 (3), 267-270 (2003).
- Wiggins, T. F., DeLegge, M. H. Evaluation of a new technique for endoscopic nasojejunal feeding-tube placement. Gastrointest Endosc. 63 (4), 590-595 (2006).
- Taylor, S. J., Karpasiti, T., Milne, D. Safety of blind versus guided feeding tube placement: Misplacement and pneumothorax risk. Intensive Crit Care Nurs. 76, 103387 (2023).
- Mumoli, N., et al. Bedside abdominal ultrasound in evaluating nasogastric tube placement: A multicenter, prospective, cohort study. Chest. 159 (6), 2366-2372 (2021).
- Hillard, A. E., Waddell, J. J., Metzler, M. H., McAlpin, D. Fluoroscopically guided nasoenteric feeding tube placement versus bedside placement. South Med J. 88 (4), 425-428 (1995).
- Cresci, G., Martindale, R. Bedside placement of small bowel feeding tubes in hospitalized patients: a new role for the dietitian. Nutrition. 19 (10), 843-846 (2003).
- Patrick, P. G., Marulendra, S., Kirby, D. F., DeLegge, M. H. Endoscopic nasogastric-jejunal feeding tube placement in critically ill patients. Gastrointest Endosc. 45 (1), 72-76 (1997).
- Schwab, D., et al. Endoscopic placement of nasojejunal tubes: a randomized, controlled, prospective trial comparing suitability and technical success for two different tubes. Gastrointest Endosc. 56 (6), 858-863 (2002).
- Fanara, B., Manzon, C., Barbot, O., Desmettre, T., Capellier, G. Recommendations for the intra-hospital transport of critically ill patients. Crit Care. 14 (3), 87 (2010).
- Neumann, D. A., DeLegge, M. H. Gastric versus small-bowel tube feeding in the intensive care unit: A prospective comparison of efficacy. Crit Care Med. 30 (7), 1436-1438 (2002).
- Levy, H. Nasogastric and nasoenteric feeding tubes. Gastrointest Endosc Clin N Am. 8 (3), 529-549 (1998).
- Dranoff, J. A., Angood, P. J., Topazian, M. Transnasal endoscopy for enteral feeding tube placement in critically ill patients. Am J Gastroenterol. 94 (10), 2902-2904 (1999).
- Rahman, A., et al. Identifying critically-ill patients who will benefit most from nutritional therapy: Further validation of the "modified NUTRIC" nutritional risk assessment tool. Clin Nutr. 35 (1), 158-162 (2016).
- Mutchmore, A., Lamontagne, F., Chasse, M., Moore, L., Mayette, M. Automated APACHE II and SOFA score calculation using real-world electronic medical record data in a single center. J Clin Monit Comput. 37 (4), 1023-1033 (2023).
- Zanley, E., et al. Guidelines for gastrostomy tube placement and enteral nutrition in patients with severe, refractory hypoglycemia after gastric bypass. Surg Obes Relat Dis. 17 (2), 456-465 (2021).
- Chen, M. C., Chao, H. C., Yeh, P. J., Lai, M. W., Chen, C. C. Therapeutic efficacy of nasoenteric tube feeding in children needing enteral nutrition. Front Pediatr. 9, 646395 (2021).
- Wang, L., Tian, Z., Liu, Y. Nasoenteric tube versus jejunostomy for enteral nutrition feeding following major upper gastrointestinal operations: a meta-analysis. Asia Pac J Clin Nutr. 26 (1), 20-26 (2017).
- Liu, Z., et al. Evaluation of ultrasound-guided Freka-Trelumina enteral nutrition tube placement in the treatment of acute pancreatitis. BMC Gastroenterol. 20 (1), 21 (2020).
- Chen, Y., et al. A multifaceted comparative analysis of image and video technologies in gastrointestinal endoscope and their clinical applications. Front Med (Lausanne). 10, 1226748 (2023).
- Roy, S., Santosh, K. C. Analyzing overlaid foreign objects in chest X-rays-clinical significance and artificial intelligence tools. Healthcare (Basel). 11 (3), 308 (2023).
- Ferraboli, S. F., Beghetto, M. G. Bedside ultrasonography for the confirmation of nasogastric tube placement: agreement between nurse and physician. Rev Gaucha Enferm. 43, 20220211 (2022).
- Valla, F. V., Cercueil, E., Morice, C., Tume, L. N., Bouvet, L. Point-of-care gastric ultrasound confirms the inaccuracy of gastric residual volume measurement by aspiration in critically ill children: GastriPed Study. Front Pediatr. 10, 903944 (2022).
- Lu, G., et al. Endoscopic- versus x-ray-guidance for placement of nasojejunal tubes in critically ill patients: a systematic review and meta-analysis of randomized controlled trials. Am J Transl Res. 14 (4), 2134-2146 (2022).
- Bosco, J. J., et al. A reliable method for the endoscopic placement of a nasoenteric feeding tube. Gastrointest Endosc. 40 (6), 740-743 (1994).
- Zafar, M., et al. Complexities of long-term care with gastro-jejunal (GJ) feeding tubes and enteral migration during COVID-19 pandemic times: A case report. Cureus. 14 (8), e27870 (2022).
- Hawk, H., Valdivia, H. Bedside methods for transpyloric feeding tube insertion in hospitalized children: A systematic review of randomized and non-randomized trials. JPediatr Nurs. 60, 238-246 (2021).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved