Method Article
Minimal Invasive Resection of Large Retrosternal Thyroid Goiter
In This Article
Summary
Here, we present a protocol for retrosternal thyroid goiter resection using a thoracoscopic-assisted transcervical approach.
Abstract
Resecting a large goiter extending into the retrosternal space is challenging, especially when a sternotomy or thoracotomy is required. The transthoracic approach is linked to higher postoperative morbidity, reaching up to 30% when compared to the transcervical approach. Although alternative options like thoracoscopic resection have shown promising results, the morbidity of mediastinal dissection remains a concern. Thoracoscopic-assisted transcervical approach might be a feasible, less invasive alternative. This video outlines the steps and potential pitfalls of the procedure.
The patient is positioned supine with an extended neck. Initially, the endocrine surgeon mobilizes the thyroid gland through cervical access. If a transcervical resection is not feasible, the patient is mobilized into a lateral decubitus position, and a second team thoracoscopically guides the mediastinal tumor through the thoracic inlet. This allows a stepwise controlled transcervical dissection of the retrosternal mass until complete resection is achieved, thus eliminating the need for mediastinal dissection.
To demonstrate the procedure, we present the case of an 84-year-old male with lymph node-positive oncocytic thyroid carcinoma and a large retrosternal goiter extending posteriorly into the mediastinum up to the aortic arch. Thoracoscopic-assisted transcervical resection was performed. The recurrent laryngeal nerve was identified and monitored with a neurostimulation device during dissection. No palsy was noted in the postoperative evaluation. The patient had an uneventful postoperative course and was discharged on the second postoperative day.
Thoracoscopic-assisted transcervical resection of large retrosternal goiter seems a feasible alternative to mitigate risks associated with thoracotomy, sternotomy, or thoracoscopic mediastinal dissection. Potential advantages include decreased postoperative morbidity and length of stay. This technique requires thoracoscopic expertise and may be limited depending on the goiter's size and mediastinal positioning.
Introduction
A retrosternal goiter represents an entity of abnormal thyroid enlargement, with its largest mass extending through the thoracic inlet into the intrathoracic space1. Therefore, retrosternal goiters differ from nodular goiters anatomically rather than physiopathologically. Triggered by environmental and genetic factors, goiter development is also associated with iodine deficiency, thyroid nodules, Hashimoto's thyroiditis, and Graves' disease. The prevalence of retrosternal goiters varies greatly by region, from 0.02% to 30% and adopted definitions1,2,3,4. Retrosternal goiters typically occur in the anterior mediastinum (80-90%) and more rarely posterior to the trachea or esophagus in the posterior mediastinum. Since anatomical structures limit thyroid tissue expansion except in the inferior part, goiters expand downward through the thoracic inlet4. This might also be triggered by gravity, traction during swallowing, negative pressure, and individual anatomy.
Surgery is indicated for retrosternal goiters with suspected malignancy, compressive symptoms, and cosmetic issues and selectively for hyperthyroid goiters5. Resection of asymptomatic goiters is usually not indicated, although controversial due to malignancy risk and size expansion over the years4,5. Due to their anatomical position, retrosternal goiters present specific challenges during surgical resection. Most goiters can be resected through a transcervical approach; however, a transthoracic approach via sternotomy or thoracotomy may be indicated6. These procedures are clearly linked to higher postoperative morbidity. Therefore, minimally invasive approaches are being investigated to improve outcomes7,8,9,10,11,12. However, the morbidity linked to mediastinal dissection remains a concern.
This article presents an innovative yet simple technique: a thoracoscopic-assisted transcervical approach without mediastinal dissection that might potentially mitigate the risks of conventional techniques. To introduce the technique, a brief background is provided with the following key points: (i) Retrosternal goiter: definition and incidence, (ii) Indication for resection, (iii) Transcervical resection is feasible in >95% of cases, (iv) Transthoracic approaches for larger goiter (linked to higher morbidity, longer length of stay, and higher transfusion rate), (v) Thoracoscopic-assisted transcervical resection as an alternative approach.
To illustrate the procedure technique and pitfalls, we present the case of an 84-year-old male with a large retrosternal goiter on the right side (Figure 1) and an oncocytic thyroid carcinoma on the left side with positive lymph nodes in the cervico-lateral compartment undergoing a thoracoscopic-assisted transcervical thyroidectomy.
Protocol
The protocol follows the guidelines of Bern University Hospital's human research ethics committee. The patient provided both written and oral consent for the anonymous use of his surgical images.
1. Surgery Part I: Transcervical resection
NOTE: The first step of this procedure involves a thyroidectomy performed in a standard fashion with a transcervical approach. Since the carcinoma is located on the left side, it is common practice to begin on this side.
- Position the patient: Position the patient supine with the neck extended.
- Perform incision: Perform a 6 cm Kocher incision (or collar incision) at the base of the neck, two transverse fingers above the sternal notch.
- Gain access to the thyroid gland.
- Perform the dissection of the platysma and exposure of the strap muscles up to the larynx and down to the posterior face of the manubrium sterni.
- From the midline, mobilize the strap muscles laterally to expose the left thyroid gland.
- Perform a transcervical left thyroidectomy with intermittent neuromonitoring of the vagal and recurrent laryngeal nerve to ensure the preservation of these structures.
NOTE: Identification and preservation of the recurrent laryngeal nerve are critical to avoid postoperative palsy, which can manifest as hoarseness, changes in the pitch of the vocal, or noisy breathing (unilateral). If palsy is suspected after resection on one side, surgery on the contralateral side is contraindicated due to the risk of postoperative palsy of the recurrent laryngeal nerve on both sides and, therefore, airway obstruction upon extubation. Neuromonitoring is performed using the NIM 3.0 Nerve Monitoring System from Medtronic with audible and visual signals for the vagal and recurrent laryngeal nerves to ensure their preservation. The process includes the following steps.- Ensure placement of endotracheal tube electrodes by the anesthesiology team before surgery.
- Establish baseline electrical activity by stimulating the recurrent laryngeal and vagal nerves.
- Divide the upper and inferior pole vessels between ligatures. Identify and spare the parathyroid glands.
NOTE: To prevent postoperative hypoparathyroidism, it is crucial to actively locate the parathyroid glands for preservation or reimplantation if necessary. - Conduct intermittent or continuous monitoring during tissue dissection and removal of the thyroid gland and lymph nodes to identify and protect the nerves.
- Remove the entire enlarged thyroid lobe, including the isthmus. Ensure thorough hemostasis.
NOTE: Careful ligation of vessels and ensuring proper hemostasis are essential to prevent postoperative bleeding. This is especially important during the dissection of the retrosternal goiter. - Repeat neuromonitoring of the vagal nerve and document the presence of a strong, unaltered signal.
- Perform cervico-lateral lymphadenectomy with neuromonitoring of the vagal nerve.
- Perform a cervico-lateral lymphadenectomy (level II-V) on the left side.
NOTE: This step is performed in the case discussed here because the preoperative diagnosis revealed positive lymph nodes in the cervico-lateral compartment on the left side. Cervico-central lymphadenectomy was limited due to the size of the goiter and was performed together with the thyroidectomy. - Repeat neuromonitoring of the vagal nerve and document the presence of a strong, unaltered signal.
- Perform a cervico-lateral lymphadenectomy (level II-V) on the left side.
- Mobilize the right thyroid lobe.
- Initially, perform the same procedure as on the left side. In this case, the right thyroid lobe is enlarged and extends deeply into the posterior mediastinum.
- Gradually mobilize the thyroid gland. Here, this is only partially possible due to the size and the retrosternal extension of the goiter. If necessary, continue the resection with thoracoscopic assistance.
2. Surgery Part II: Thoracoscopic-assisted transcervical resection
NOTE: The thoracic and cervical surgical team should possess the expertise necessary to manage potential complications associated with the dissection of a retrosternal goiter, such as uncontrolled bleeding in the mediastinum. In this case, an emergency thoracotomy or a thoracoscopic mediastinal dissection might be indicated.
- Position the patient.
- Position the patient in a lateral decubitus position. For this maneuver, cover the transcervical wound with a sterile bandage and remove the sterile drapes. Place a right bronchial blocker in a standard endotracheal tube.
NOTE: The placement of the right bronchial blocker is done by the anesthesiology team. Careful preoperative work-up is crucial to assess and ensure that the patient is capable of tolerating one-lung ventilation during the thoracic part of the procedure. - Perform a new disinfection and sterile draping of the patient.
- Position the patient in a lateral decubitus position. For this maneuver, cover the transcervical wound with a sterile bandage and remove the sterile drapes. Place a right bronchial blocker in a standard endotracheal tube.
- Perform right thoracoscopy.
- Perform a right thoracoscopy with the placement of two 12 mm trocars (subscapular and submammary). The right lung is desufflated after bronchial blocker placement, allowing visualization of the large goiter extending to the azygos arch.
- Perform a thoracoscopic-assisted transcervical right thyroidectomy with intermittent neuromonitoring of the vagal and recurrent laryngeal nerve (Figure 2).
- Thoracic team (one surgeon positioned on the patient's right): push the goiter cranially through the thoracic inlet.
- Cervical team (one surgeon and an assistant positioned on the patient's left): Perform a stepwise dissection and resection of the right thyroid lobe, including the retrosternal goiter (right thyroid gland, size: 13.5 cm x 8.5 cm x 8.5 cm, weight: 320 g).
- Repeat neuromonitoring of the vagal nerve and document the presence of a strong, unaltered signal.
- Insert drainage and perform wound closure.
- Insert a negative pressure drainage into the thyroid bed on both sides. Close the strap muscles and platysma with a continuous suture.
- Close the skin with a resorbable continuous intracutaneous suture, followed by the application of steri-strips.
- If necessary, insert a Charrière 14 thoracic drainage with 10 mmHg suction. Close the thoracic access by using a resorbable subcutaneous suture and a non-resorbable skin suture, followed by the application of a sterile dressing.
3. Postoperative follow-up
- Monitor for 24-48 h following surgery, with particular attention to any signs of bleeding (such as local swelling, vocal changes, expiratory stridor, or respiratory distress) and hypocalcemia.
- Measure a parathyroid hormone (PTH) level on the first postoperative day to assess for any transient or permanent hypoparathyroidism and administer calcium and calcitriol supplementation as needed.
- Routinely assess the vocal cord function to detect any vocal cord palsy. Provide pain management with paracetamol and metamizol, and avoid nonsteroidal anti-inflammatory drugs (NSAIDs) to minimize the risk of postoperative bleeding.
NOTE: In the case presented, the patient had an uneventful postoperative course and was discharged on the second postoperative day. No vocal cord palsy or hypocalcemia was noted during the postoperative evaluation.
Results
We have adopted this innovative technique since 2021. We always start the resection of retrosternal goiter with a transcervical approach, as the vast majority of retrosternal goiters can be resected this way. If we suspect that a transthoracic approach might be needed, the patient is informed about this possibility, and the thoracic team is notified in advance and ready to step in if necessary.
From January 1, 2021, to December 31, 2023, we performed 481 thyroidectomies at our institution, of which 0.4% (n = 2) required a transthoracic approach. In both cases, a thoracoscopic-assisted transcervical resection was successful. Patients were discharged on the second postoperative day. Postoperative follow-up was uneventful, with no postoperative complications. As a representative example, we present a case of an 84-year-old male with a large retrosternal goiter. Figure 1 shows the CT with venous contrast indicating retrosternal goiter on the transverse (Figure 1A) and coronal planes (Figure 1B). Figure 2 shows the thoracoscopic-assisted transcervical right thyroidectomy with intermittent neuromonitoring of the vagal and recurrent laryngeal nerves.
To our knowledge, no other data on the thoracoscopic-assisted (without mediastinal dissection) approach is available. This is due to the novelty of the technique and the rarity of such procedures (0.3%-4% of thyroidectomies)13.
Testini et al. reported the results of a multicenter analysis of 19,662 thyroidectomies, among which 0.35% (n = 69) involved a transthoracic approach. Retrosternal goiter had higher postoperative morbidity than cervical goiter (35% vs. 23.7%, p < 0.001), and the morbidity was even higher when a transthoracic approach was used (53.5%)13.
Khan et al. reported a comparison from the National Surgical Quality Improvement Program (NSQIP) database between patients undergoing retrosternal goiter resection with a transcervical versus a transthoracic approach. In their analysis, transthoracic approaches were associated with longer lengths of stay (2.4 vs. 1.5 days, p < 0.001), higher rates of unplanned intubation (OR [95% CI] 2.7 [1.17-6.25]), and transfusion (OR [95% CI] 5.56 [2.38-13.0])6.
Thoracoscopic-assisted transcervical resection presents a promising alternative to traditional thoracotomy, sternotomy, or thoracoscopic mediastinal dissection for large retrosternal goiters. This minimally invasive technique might significantly reduce postoperative morbidity, such as surgical site infections and respiratory complications. The avoidance of mediastinal dissection may result in shorter operative times, reduced blood loss, and fewer intraoperative injuries. This effect would be especially beneficial in an elderly and high-risk population. The approach requires a second surgical team experienced in thoracoscopic procedures and the use of a bronchial blocker.
To validate the effectiveness and safety of this technique, larger case series and further studies are warranted. While thoracoscopic-assisted transcervical resection may offer advantages, its applicability might be limited by the size and position of the goiter within the mediastinum, as well as the need for mediastinal lymph node dissection. Careful patient selection and a thorough understanding of the potential limitations are crucial for optimizing outcomes.
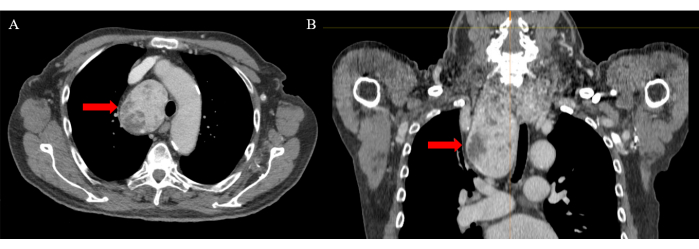
Figure 1: Computed tomography with venous contrast. The red arrow indicates retrosternal goiter on the (A) transverse and (B) coronal planes. Please click here to view a larger version of this figure.

Figure 2: Thoracoscopic-assisted transcervical right thyroidectomy. (A) Thoracoscopic view of the retrosternal goiter. (B) The goiter is pushed through the thoracic inlet (C) while the transcervical resection is performed Please click here to view a larger version of this figure.
Discussion
The great majority of retrosternal goiters can be resected with a transcervical approach13. However, if this is not feasible or in the eventuality of a complication, such as uncontrolled bleeding, the surgeon must be prepared for a bail-out procedure to access the retrosternal part of the goiter. Usually, a thoracotomy or thoracoscopy is used for a retrosternal goiter located in the posterior mediastinum, and a sternotomy is performed for goiter in the anterior mediastinum. Risk factors for thoracic access include malignancy, mediastinal malignant nodes, extension of the goiter below the aortic arch or subcarinal region, history of retrosternal goiter, ectopic thyroid nodule, thyroid tissue density, and goiter located in the posterior mediastinum13,14,15,16.
Sternotomy and thoracotomy are clearly associated with higher postoperative morbidity, up to 30%, including higher transfusion rates, hematoma, hypoparathyroidism, palsy of the recurrent laryngeal nerve, unplanned intubation, and longer hospital stays6,13. It is, however, unclear if part of these complications can solely be explained by the access itself or if they are linked to the anatomical challenges posed by large retrosternal goiters that are not resectable through a transcervical approach. Nevertheless, sternotomy or thoracotomy should be avoided whenever possible without compromising the surgery's safety. Emergent procedures such as thoracoscopic resection or robotic-assisted thoracoscopic resection with mediastinal dissection have been described in case series7,8,9,10,11,12. Although the sample sizes are too small to evaluate their outcomes compared to a transcervical or open thoracic approach, the required mediastinal dissection might still be associated with significant morbidity when compared to the transcervical approach. The present technique offers the advantage of minimally invasive access to the thoracic space with only two trocars and without mediastinal dissection17. The use of a normal endotracheal tube with intermittent desufflation using a bronchial blocker during the thoracoscopic phase is also linked to lower pulmonary complications compared to a double-lumen tube18,19. Further studies are needed to draw conclusions on its associated morbidity. However, lower morbidity than the open thoracic approach might be expected.
Possible limitations of this technique are expected in goiters with a larger anteroposterior dimension than the thoracic inlet, as well as retrosternal goiters localized in the anterior part of the mediastinum. If lymph node metastases are present in the mediastinum, a mediastinal dissection might be necessary. In the present case, no mediastinal lymph nodes were evident on the preoperative imaging.
Disclosures
The authors have no disclosure or conflict of interest.
Acknowledgements
None
Materials
| Name | Company | Catalog Number | Comments |
| 12 mm Balloon Trocar | N/A | N/A | Thoracoscopic part |
| Bipolar Forceps | Symmetry Surgical | https://www.aspensurgical.com/Catalog/Products/open-surgery-instruments | Cervical part |
| Laparoscopic grasper | Thoracoscopic part | ||
| Laparoscopy tower | Karl Storz | https://www.karlstorz.com/us/en/category.htm?cat=1000113577 | Thoracoscopic part |
| LigaSure Impact Open Instrument | Medtronic | https://www.medtronic.com/covidien/en-us/support/products/vessel-sealing/ligasure-impact-sealer-divider.html | Cervical part |
| NIM 3.0 Systems | Medtronic | https://www.medtronic.com/us-en/healthcare-professionals/products/ear-nose-throat/neuromonitoring/nerve-integrity-monitor-3.html | Neuromonitoring |
| Surgical instruments and draping for open surgery | N/A | N/A | Cervical part |
References
- Ríos, A., Rodríguez, J. M., Balsalobre, M. D., Tebar, F. J., Parrilla, P. The value of various definitions of intrathoracic goiter for predicting intra-operative and postoperative complications. Surgery. 147 (2), 233-238 (2010).
- Newman, E., Shaha, A. R. Substernal goiter. J Surg Oncol. 60 (3), 207-212 (1995).
- Knudsen, N., Bülow, I., Jørgensen, T., Laurberg, P., Ovesen, L., Perrild, H. Goitre prevalence and thyroid abnormalities at ultrasonography: a comparative epidemiological study in two regions with slightly different iodine status. Clin Endocrinol (Oxf). 53 (4), 479-485 (2000).
- Knobel, M. An overview of retrosternal goiter. J Endocrinol Invest. 44 (4), 679-691 (2021).
- Bartsch, D. K., Luster, M., Buhr, H. J., Lorenz, D., Germer, C. T., Goretzki, P. E. Indications for the surgical Management of Benign Goiter in Adults. Dtsch Arztebl Int. 115 (1-2), 1-7 (2018).
- Khan, M. N., Goljo, E., Owen, R., Park, R. C. W., Yao, M., Miles, B. A. Retrosternal goiter: 30-day morbidity and mortality in the transcervical and transthoracic approaches. Otolaryngol Head Neck Surg. 155 (4), 568-574 (2016).
- Bhargav, P., Amar, V., Mahilvayganan, S., Nanganandadevi, V. Feasibility of thoracoscopic approach for retrosternal goitre (posterior mediastinal goitre): Personal experiences of 11 cases. J Minim Access Surg. 12 (3), 240-244 (2016).
- Brichkov, I., Chiba, S., Lagmay, V., Shaw, J. P., Harris, L. J., Weiss, M. Simultaneous unilateral anterior thoracoscopy with transcervical thyroidectomy for the resection of large mediastinal thyroid goiter. J Thorac Dis. 9 (8), 2484-2490 (2017).
- Shigemura, N., Akashi, A., Nakagiri, T., Matsuda, H. VATS with a supraclavicular window for huge substernal goiter: an alternative technique for preventing recurrent laryngeal nerve injury. Thorac Cardiovasc Surg. 53 (4), 231-233 (2005).
- Zuo, T., Gao, Z., Chen, Z., Wen, B., Chen, B., Zhang, Z. Surgical management of 48 patients with retrosternal goiter and tracheal stenosis: A retrospective clinical study from a single surgical center. Med Sci Monit. 28, e936637 (2022).
- Wang, S., Xu, S., Liu, B. Resection of huge retrosternal goiter through a novel combined cervical and robot-assisted approach. Artif Organs. 38 (5), 431-433 (2014).
- Amore, D., Cicalese, M., Scaramuzzi, R., Di Natale, D., Curcio, C. Antero mediastinal retrosternal goiter: surgical excision by combined cervical and hybrid robot-assisted approach. J Thorac Dis. 10 (3), E199-E202 (2018).
- Testini, M., et al. Does mediastinal extension of the goiter increase morbidity of total thyroidectomy? A multicenter study of 19,662 patients. Ann Surg Oncol. 18 (8), 2251-2259 (2011).
- McKenzie, G. A. G., Rook, W. Is it possible to predict the need for sternotomy in patients undergoing thyroidectomy with retrosternal extension. Interact Cardiovasc Thorac Surg. 19 (1), 139-143 (2014).
- Coskun, A., Yildirim, M., Erkan, N. Substernal goiter: when is a sternotomy required. Int Surg. 99 (4), 419-425 (2014).
- Mercante, G., et al. CT cross-sectional imaging classification system for substernal goiter based on risk factors for an extracervical surgical approach. Head Neck. 33 (6), 792-799 (2011).
- Nesti, C., Wohlfarth, B., Borbély, Y. M., Kaderli, R. M. Case report: Modified thoracoscopic-assisted cervical resection for retrosternal goiter. Front Surg. 8, 695963 (2021).
- Liu, W., Jin, F., Wang, H. M., Yong, F. F., Wu, Z., Jia, H. Q. The association between double-lumen tube versus bronchial blocker and postoperative pulmonary complications in patients after lung cancer surgery. Front Oncol. 12, 1011849 (2022).
- Palaczynski, P., et al. Systematic review and meta-analysis of efficiency and safety of double-lumen tube and bronchial blocker for one-lung ventilation. J Clin Med. 12 (5), 1877 (2023).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved