Method Article
Arthroscopic Management of Massive Irreparable Rotator Cuff Tears: Whole Rotator Cable Reconstruction Using Proximal Biceps Tendon Autograft
In This Article
Summary
Massive irreparable rotator cuff tears (MIRCTs) pose significant clinical challenges due to their complex pathology and limited treatment options. This study introduces whole rotator cable reconstruction (WRCR) using proximal biceps tendon autograft as a novel surgical technique for MIRCTs.
Abstract
Massive irreparable rotator cuff tears (MIRCTs) are not uncommon in clinical practice, significantly impacting shoulder function and daily activities. Extensive tear size, tendon contracture, and fat infiltration within the rotator cuff pose significant challenges for both patients and clinicians. This type of tear is a key area of interest and a challenge in research and treatments. Current treatment options include conservative management, debridement, partial repair, superior capsule reconstruction (SCR), tendon transfers, and reverse total shoulder arthroplasty (RTSA). However, clinical outcomes vary widely.
The rotator cable (RC) exhibits a perpendicular orientation with respect to the superior rotator cuffs, thereby forming an arc-shaped attachment to the proximal humerus, and it plays an essential role in maintaining the rotator cuff's force couple. The attachments of both anterior and posterior RC play a crucial role in facilitating overhead movements. When complete tension-free coverage of the footprint cannot be attained, whole rotator cable reconstruction (WRCR) presents as an alternative approach for MIRCTs. We utilized autologous tendon harvested from the proximal biceps tendon for arthroscopic WRCR. The proposed technique offers distinct advantages: autologous tissue utilization eliminates immunogenicity; simplified harvesting reduces operative complexity; and minimized anchor usage enhances cost-effectiveness. In this study, 12 patients underwent WRCR, with significant improvements in shoulder function and pain relief observed during a 1 year follow-up.
Introduction
Massive rotator cuff tears (MRCTs) are defined as tears involving at least two tendons or tears wider than 5 cm. Approximately 20% of primary rotator cuff tears and 80% of recurrent tears fall into this category1,2. The documented rate of treatment failure for MRCTs is approximately 40%3. In some cases, MRCTs are deemed irreparable due to muscle atrophy, fat infiltration, and severe tendon contracture, making low-tension anatomical repair impossible4,5. Some investigators have reported the incidence of MIRCTs up to 30%6,7. Due to the increasing prevalence of shoulder pain among elderly patients and the escalating demands of daily activities and exercise, as well as the unique characteristics of MIRCTs, its treatment necessitates a highly intricate and crucial decision-making process.
Current therapeutic strategies for MIRCTs encompass a spectrum of interventions ranging from conservative management to advanced surgical techniques such as superior capsular reconstruction (SCR) and reverse total shoulder arthroplasty (RTSA) 8. The appropriate treatment depends on a comprehensive evaluation of various factors. Reconstructing the rotator cuff is considered the primary treatment for elderly patients with low demand and non-shoulder osteoarthritis9.
The rotator cable (RC), spanning from the supraspinatus anterior margin to the infraspinatus posterior border, functions as a biomechanical suspension system that preserves coronal plane force equilibrium within the rotator cuff complex10. Evidence indicates that the combined technique of rotator cuff repair and anterior cable reconstruction utilizing the proximal biceps tendon achieves satisfactory functional and anatomical outcomes in patients with massive retracted anterosuperior L-shaped rotator cuff tears11. In a previous study, anterior rotator cable reconstruction was successfully achieved using a V-shaped hamstring allograft for the management of MIRCTs, demonstrating favorable biomechanical functionality12.
Posterior cable insertion has been reported to play a crucial role as a connecting structure among the Teres minor (TM), infraspinatus (ISP), and supraspinatus (SSP). As a result, complete rupture of the entire cable can lead to significant impairment of shoulder function in patients13. Previous study was conducted to investigate the efficacy of suture-based cable reconstruction in partially repairing the rotator cuff14. Drawing on prior research, we adopt the whole rotator cable reconstruction (WRCR) technique to treat MIRCTs.Theoretically, this technique offers greater potential to restore optimal coronal plane equilibrium and is more likely to enhance the patient's shoulder function when the rotator cuff cannot be completely repaired without applying tension.
Protocol
This study adhered to the guidelines set by the Ethics Committee of the 909th Hospital, Xiamen University School of Medicine. Informed consent was obtained from all participants. The study included 12 patients (7 females and 5 males) aged 50 to 70 years.
1. Preoperative preparation
- Set the following inclusion criteria: patients with a preliminary diagnosis of MIRCT by magnetic resonance imaging (MRI) and Hamada type 2 or type 1 MIRCT15, aged between 50 and 70, and those with treatment failure after standard conservative treatment.
NOTE: Confirm MIRCT under arthroscopy if tension-free sutures cannot adequately cover the footprint. - Set the following exclusion criteria: patients with a history of previous shoulder surgery; those with grade 4 fatty infiltration16; injury involving more than half of the tendon of the long head of the biceps brachii or absence of the tendon; patients with intolerance to general anesthesia; and those with irreparable anterior or posterior rotator cuff tears that could not restore the horizontal force couple balance.
2. Arthroscopy surgical procedures
- Anesthesia and patient positioning
- Perform the surgery under general anesthesia with a brachial plexus block. Place the patient on their side. Cushion all bony prominences with sponge pads to prevent pressure ulcers. Assess the degree of adhesion in the shoulder joint and manually release the joint.
- Immobilize the operative arm using a foam traction sleeve. Apply a 3-6 kg traction force using a simple traction frame. Tilt the torso back at an angle of 30°, maintain the abduction of the operative arm at 60°, and set flexion at 30°. Mark anatomical landmarks and portal positions prior to disinfection using iodine tincture and alcohol (Figure 1).
- Establishing the arthroscopic approaches
- Create a standard posterior portal. Make a 0.5 cm skin incision using an 11 G blade.
- Insert a 30° arthroscope toward the rotator interval. Target the anterior light spot through an incision along the lateral coracoid process. Observe the shoulder cavity contents, evaluate the biceps long head tendon, and release the rotator interval if adherent.
- Enter the subacromial space via the posterior arthroscopic approach. Establish anterolateral and lateral approaches 4 cm beyond the lateral acromion border (Figure 2).
- Evaluation of the subacromial space
- Observe the subacromial space from the posterior portal and insert a shaver through the anterolateral approach to debride thickened bursa and adhesive tissues. Use a radiofrequency probe for hemostasis and mark the anterolateral acromion if hyperplasia or impingement is observed. Debride subacromial soft tissues with hyperplasia using an arthroscopic shaver, and remove subacromial spurs with a Burr.
- Reassess rotator cuff tears from the lateral portal, including tear pattern, extension, fatty atrophy, retraction, and location. Evaluate the biceps long head tendon. Proceed with WRCR if MIRCTs cannot be restored to the footprint without tension after release (Figure 3).
- Preparation of the long head tendon of the biceps
- Use a radiofrequency probe to meticulously dissect and fully expose the distal end of the long head of the biceps tendon, ensuring clear visualization of the surrounding structures. Carefully transect the tendon at the insertion using a Basket Punch, and maintain 6-7 cm tendon length throughout (Figure 4).
- Braid the long head tendon using four No. 2 Orthocord braided composite sutures at both ends and the center (Figure 5).
- Release of the rotator cuff and preparation of the footprint
- Carefully freshen the footprint on the bone surface using a burr. Create a 'U'-shaped groove extending from the cartilage margin to the distal end of the greater tubercle, positioned at the original anterior and posterior cable locations (Figure 6).
NOTE: Retracted rotator cuff tissues should be thoroughly released to prevent suprascapular nerve injury. If present, torn subscapular tendons should be repaired using anchor sutures.
- Carefully freshen the footprint on the bone surface using a burr. Create a 'U'-shaped groove extending from the cartilage margin to the distal end of the greater tubercle, positioned at the original anterior and posterior cable locations (Figure 6).
- Whole rotator cable reconstruction
- Place two 4.5 mm anchors (each loaded with two #2 sutures). Position the first anchor at the anterior edge of the 'U'-shaped groove along the cartilage rim; then, place the second anchor at the posterior edge of the groove. Carefully pull the woven long head tendon into the subacromial space, and secure the tendon at the distal end of the 'U'-shaped groove using two footprint anchors. Ensure both ends of the long head of the biceps tendon are securely anchored within the distal portion of the 'U'-shaped groove (Figure 7).
- Select the white suture from the cartilage margin anchor and pass the white suture through the long head tendon to ensure a secure hold. Tie the white suture using an SMC knot to firmly secure the tendon within the bone groove. Ensure even tension and proper seating of the tendon in the groove. Do not cut the sutured tail, leave it for the subsequent suturing of the retracted rotator cuff.
- Using a suture shuttle, sequentially pass the sutures from the cartilage margin anchor and the braided sutures at the center of the long head of the biceps tendon through the retracted rotator cuff tissue. With the assistance of a full-loop knot manipulator, secure the repair with an SMC knot. Utilize a cannula to manage the sutures and prevent tangling throughout the procedure. (Figure 8).
- Assess suturing with an arthroscopic probe hook. Add anchors or composite sutures for reinforcement to close the glenohumeral joint and subacromial space, if needed.
NOTE:The number of anchors or composite sutures required to reinforce the suture should be determined based on the intraoperative situation. This is illustrated in the case presented in the video.
- Suture of the incision
- Perform radiofrequency ablation for hemostasis. Drain fluid from the subacromial space. Suture the incision with a 3-0 silk braided suture.
3. Rehabilitation and follow-up
- Instruct patients to wear an abduction brace for six weeks postoperatively. Allow wrist and elbow movement starting postoperative day 1. Initiate passive shoulder movements at 3 weeks, active movements at 6 weeks, and muscle strength training at 12 weeks. Permit full activity, including contact sports at 6 months.
- Encourage patients to ambulate on postoperative day 2.
- Change dressings every 3 days. Remove stitches 14 days postoperatively.
- Perform shoulder radiography (AP and supraspinatus outlet views) prior to discharge.
- Discharge patients once pain decreases (VAS ≤ 4).
- Schedule follow-up visits at 3 and 6 weeks, 3 and 6 months, and 1 year postoperatively.
- Assess VAS score, shoulder ROM, ASES score, X-ray, and MRI at 6 months, 12 months, and annually thereafter.
Results
WRCR using the proximal biceps tendon autograft was performed in 12 patients between February 2021 and March 2023, with suture repair in four cases of subscapular muscle partial tear; 7 out of 12 patients had adhesions of varying degrees, and all of them underwent manual release after anesthesia. Postoperative complications were not observed. The one-year follow-up revealed significant improvement in shoulder function (P < 0.05) and pain relief (P < 0.05) as compared to those before surgery. The postoperative active range of motion (ROM) significantly increased throughout the follow-up period (Table 1). One patient exhibited Popeye's sign, while two patients experienced retear and three patients presented supraspinatus muscle atrophy. Nevertheless, their postoperative clinical functions were improved.
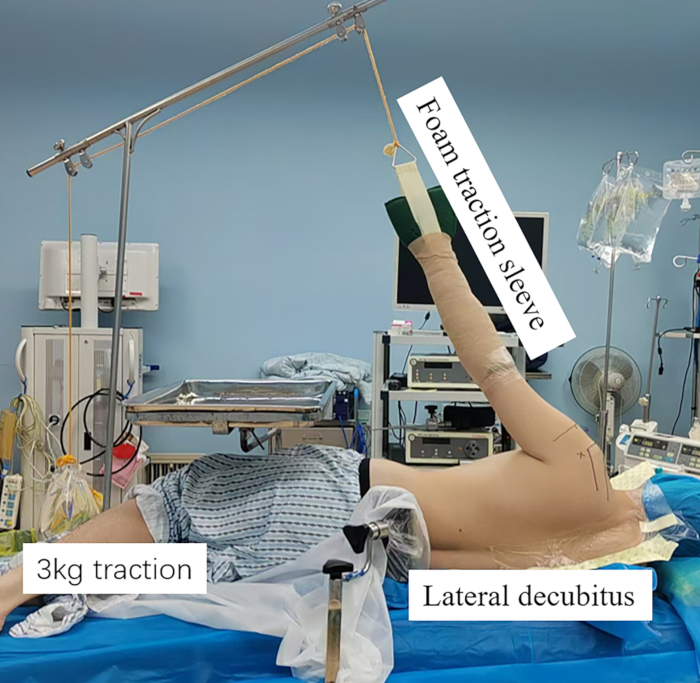
Figure 1: The representative surgical positionfor left rotator cuff tear in a 60-year-old man. The patient was placed in the recumbent position on the side on an operating table with the aid of a pelvic fixator. The left arm to be involved in the operation was fastened in a foam traction sleeve, and a basic traction frame was used to apply a traction force ranging from 3 to 6 kg. Additionally, the torso was tilted back by 30°, and the left arm abduction and flexion angles were set at 60° and 30°, respectively. Please click here to view a larger version of this figure.
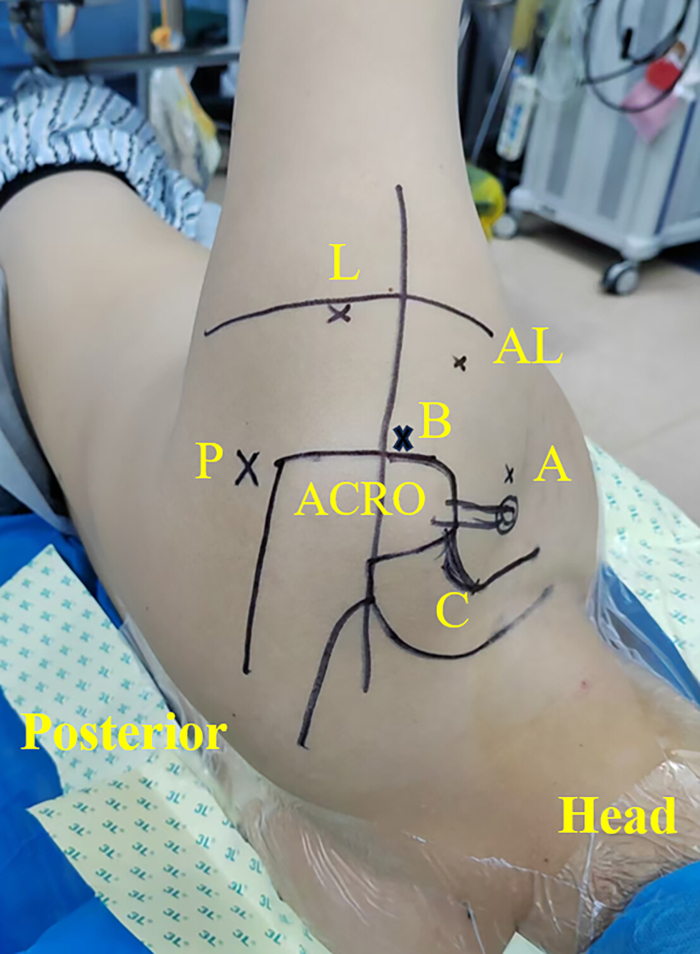
Figure 2: Portal of the left shoulder. Abbreviations: A = anterior portal; B = anterior upper portal; L = lateral portal; AL = accessory anterolateral portal; P = posterior portal; ACRO = bone landmarks acromion; C = distal clavicle. Please click here to view a larger version of this figure.

Figure 3: MIRCT confirmation under arthroscopy. After being released, the evaluation reveals that the massive irreparable rotator cuff tears cannot be anatomically repaired due to excessive tension. (A) Schematic view showing retraction of the torn supraspinatus and infraspinatus tendons. (B) Arthroscopic view from the lateral portal demonstrates a "U"-shaped tear of the supraspinatus and infraspinatus tendons retracted into the glenoid cavity. Abbreviations: SS = supraspinatus; IS = infraspinatus; BT = biceps tendon; SSC = subscapularis; G = glenoid; HH = humeral head. Please click here to view a larger version of this figure.

Figure 4: Tenotomy of the biceps tendon. The distal end of the long head of the biceps tendon is released and mobilized using a radiofrequency probe, followed by transection of both the distal and proximal ends. (A) Schematic view demonstrating the transection of the long head of the biceps brachii tendon at its proximal and distal ends. (B) Arthroscopic transection of the proximal insertion of the long head of the biceps tendon using a basket punch. Abbreviations: SS = supraspinatus; IS = infraspinatus; BT = biceps tendon; SSC = subscapularis; G = glenoid; HH = humeral head. Please click here to view a larger version of this figure.

Figure 5: Braiding of the biceps tendon with four sutures #2 violet braided composite suture at both ends and the center. (A) Schematic illustrating the positions of four braided sutures. (B) Appearance after braided suture repair of the long head of the biceps tendon. Please click here to view a larger version of this figure.

Figure 6: Creation of a bone groove. The groove stretches from the margin of the cartilage to the distal end of the great tubercle, precisely at the location where the anterior and posterior original cable. (A) Schematic illustrating the creation of bone groove using a high-speed burr. (B) Arthroscopic view shows a fresh bone groove. Please click here to view a larger version of this figure.

Figure 7: Secure fastening of the braided biceps tendon using four anchors within the bone grooves. (A) The schematic illustrates the fixation of the long head biceps tendon within a bone groove using four suture anchors positioned at points I, II, III, and IV, creating a cable structure. (B) Arthroscopic view four anchors securely fixed, with the central portion remaining unsutured to the rotator cuff. I/II, footprint anchors; III/IV, #2 sutures anchors. Please click here to view a larger version of this figure.

Figure 8: Surgical repair of the retracted rotator cuff by suturing with a braided biceps tendon, forming the WRCR. (A) Schematic view demonstrates that the long head of the biceps tendon is U-shaped fixed within the bone groove of the greater tuberosity and forms a WRCR after combined suturing with the rotator cuff. (B) Arthroscopic view the formation of WRCR after suturing the supraspinatus tendon, infraspinatus tendon, and long head of the biceps tendon. Under minimal tension, additional anchors or composite sutures for reinforcement to close the glenohumeral joint. Abbreviations: SS = supraspinatus; IS = infraspinatus; SSC = subscapularis; BT = biceps tendon; HH = humeral head. Please click here to view a larger version of this figure.
| Postoperative 1 year | ||
| VAS | 4.58±1.17 | 0.67±0.78 |
| ASES score | 43.30±6.00 | 84.43±4.74 |
| Forward flexion (°) | 101.33±27.77 | 154.08±13.58 |
| Lateral external rotation (°) | 34.83±10.55 | 41.42±10.29 |
| Internal rotation | 7.00±4.00 | 8.83±3.00 |
Table 1: Clinical manifestations of patients before surgery and in the postoperative follow-up. For internal rotation of the back region, the measured values were translated into numerical data: T1 through T12 to 20 through 9, L1 through L5 to 8 through 4, sacrum to 3, buttock to 2, and thigh to 1. At the 1 year follow-up, clinical manifestations, VAS score, and ASES score were improved as compared to those before surgery (P < 0.05).
Discussion
The management of MIRCTs remains a critical challenge in orthopedic surgery, necessitating continued exploration of biomechanically sound reconstruction techniques. The tension-free anatomical restoration of the torn rotator cuff represents the optimal therapeutic approach in our clinical practice. The presence of extensive tears and severe tendon contracture in patients with MIRCTs adversely affects the achievement of tension-free anatomical repair. The available treatments for these patients are limited in their efficacy, and currently, there are no definitive and reliable treatment options8,17. In the present study, the WRCR treatment was employed for MIRCTs patients aged 50-70 years with low demand and a desire for shoulder preservation. After surgery, the shoulder function of these patients was significantly improved as compared to that before surgery, effectively meeting the requirements of daily activities.
When the tension-free footprint cannot be repaired after the complete release of MIRCTs, WRCR can be used in patients without severe degeneration of the tendon of the long head of the biceps.If a tear occurs in either the subscapularis tendon or the teres minor (TM) tendon, it is crucial to prioritize their repair and, if necessary, any partial tears are addressed in the ISP as well. This approach aims to restore horizontal plane equilibrium and minimize the risk of postoperative pseudoparalysis18. The underlying principle of this technique is predicated on the rupture of the RC, rendering anatomical repair of the rotator cuff unfeasible without tension, while simultaneously ensuring that degeneration of the biceps tendon remains within acceptable thresholds. When it is not allowed in cases of biceps tendon injury, alternative approaches such as partial repair, SCR, and other shoulder preservation techniques can be employed.
Among individuals diagnosed with MIRCTs, conservative therapy has a failure rate of 30%, and 30% of patients eventually need surgical intervention, Partial repair has a retear rate of 45% and a reoperation rate of 10%17.Mihata et al.19 employed an autograft of the fascia lata, fixed medially to the superior glenoid rim and laterally to the greater tuberosity. This technique offers static restraint against the superior migration of the humeral head. Currently, Among the grafts frequently utilized in relevant procedures, autologous fascia lata, acellular dermal allograft, and biceps tendon rank prominently20,21,22.The SCR is gaining attraction due to its biomechanical efficacy and favorable early clinical outcomes. The previous technique necessitates the placement of six or seven anchors in both the glenoid and greater tubercle of the humerus, which entails technical intricacy and relatively high costs21,23. The proximal biceps tendon was prioritized as an autograft source due to its anatomical accessibility, negligible immunogenic risk, reduced anchor requirements (4-5 anchors), and favorable cost-benefit profile compared to allograft alternatives.When severe tearing and non-viability of the biceps tendon are identified preoperatively or intraoperatively, surgical alternatives may involve autograft substitution using the semitendinosus tendon or partial harvest of the peroneus longus tendon. In addition, surgical interventions, including superior capsular reconstruction (SCR) and suture-based cable reconstruction14, have been established as viable therapeutic alternatives for these clinical conditions.
It should be noted that this technique is particularly suitable for "U"-shaped lesions. Similarly, it is suggested to be applicable to Collin18 types C and D. The initial step involves repairing the subscapularis tendon anteriorly and the teres minor posteriorly, along with the partially repairable infraspinatus, to restore the anterior and posterior force couple balance. The technique involves the creation of a bone groove at both posterior and anterior insertion sites of the greater tuberosity, facilitating distal fixation of the long head tendon for reconstruction of the whole cable. Microfracture in the greater tuberosity footprint region, promoting healing, corresponds to the rotator cuff crescent located within the "U"-shaped long-head tendon. If tension-free is observed following suturing the supraspinatus and infraspinatus shoulders to the long head tendon, closure of the crescent area can be achieved through double-row fixation, suture-based cable reconstruction.
The use of the proximal long head of the biceps tendon in WRCR is an alternative to MIRCTs, suitable for middle-aged and elderly patients with low demand who desire shoulder preservation.This technique has lower requirements and its cost is less than that of SCR. However, the execution of this procedure requires the expertise of experienced surgeons who possess high-level proficiency in shoulder surgical techniques.However, this was a single-centered study, and further clinical studies are necessary to confirm our technology.
Disclosures
The authors have no conflicts of interest to declare.
Acknowledgements
None.
Materials
| Name | Company | Catalog Number | Comments |
| ACCU-PASS Suture Shuttle | smith&nephew | 7210423 | 45°, left |
| ACCU-PASS Suture Shuttle | smith&nephew | 7210424 | 45°, right |
| Basket Punch | smith&nephew | 7207057 | 3.5 mm |
| Blade | smith&nephew | 72202534 | 4.5 mm |
| Burr | smith&nephew | 7205668 | Straight |
| Camera Control Unit | smith&nephew | 72202334 | NTSC/PAL |
| Camera Head | smith&nephew | 72200561 | NTSC/PAL |
| Diagnostic Cannula | smith&nephew | 72200829 | |
| Diagnostic Cannula Obturator | smith&nephew | 4356 | 100-240 VAC, 50/60 Hz |
| Direct-View Arthroscopes | smith&nephew | 72202087 | |
| DYONICS POWER Footswitch | smith&nephew | 7205399 | |
| DYONICS POWER II Shaver System | smith&nephew | 72200873 | 6.0 mm, double-valve |
| DYONICS RF System | smith&nephew | 72202149 | conical tip |
| DYONICS Shaver Handpiece | smith&nephew | 72200616 | 4.0 mm, 30° |
| Fiber Optic Light Cables and Adaptors | smith&nephew | 7205180 | 4.5 mm |
| FOOTPRINT Ultra PK Suture Anchor | smith&nephew | 72202901 | 4.5mm |
| Full Loop Knot Manipulator | smith&nephew | 72201213 | 4.0 mm x 10 ft |
| Healix advance BR anchor | DePuy Mitek | 222295 | 4.5 mm |
| Light Source | smith&nephew | 72200588 | 500XL |
| ORTHOCORD Violet Braided composite suture | DePuy Mitek | 223104 | #2 |
| Spade Tip Drill | smith&nephew | 72202116 | 3.5 mm |
| Suture Cutter | smith&nephew | 7209492 | |
| Suture Loop Horizontal Grasper | smith&nephew | 72201179 | |
| Suture Loop Vertical Grasper | smith&nephew | 7209494 | |
| Threaded Cannula | smith&nephew | 72200905 | 7.0 mm x 72 mm |
References
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved