Method Article
Integration of Brain Tissue Saturation Monitoring in Cardiopulmonary Exercise Testing in Patients with Heart Failure
In This Article
Summary
This protocol integrated near-infrared spectroscopy into conventional cardiopulmonary exercise testing to identify the involvement of the cerebral hemodynamic response in exercise intolerance in patients with heart failure.
Abstract
Cerebral hypo-oxygenation during rest or exercise negatively impacts the exercise capacity of patients with heart failure with reduced ejection fraction (HF). However, in clinical cardiopulmonary exercise testing (CPET), cerebral hemodynamics is not assessed. NIRS is used to measure cerebral tissue oxygen saturation (SctO2) in the frontal lobe. This method is reliable and valid and has been utilized in several studies. SctO2 is lower during both rest and peak exercise in patients with HF than in healthy controls (66.3 ± 13.3% and 63.4 ± 13.8% vs. 73.1 ± 2.8% and 72 ± 3.2%). SctO2 at rest is significantly linearly correlated with peak VO2 (r = 0.602), oxygen uptake efficiency slope (r = 0.501), and brain natriuretic peptide (r = -0.492), all of which are recognized prognostic and disease severity markers, indicating its potential prognostic value. SctO2 is determined mainly by end-tidal CO2 pressure, mean arterial pressure, and hemoglobin in the HF population. This article demonstrates a protocol that integrates SctO2 using NIRS into incremental CPET on a calibrated bicycle ergometer.
Introduction
Cardiopulmonary exercise testing (CPET) has been applied in patients with heart failure with reduced ejection fraction (HF) for multiple aims, including the quantification of cardiopulmonary fitness, prognosis, diagnosing causes of exercise limitations, and exercise prescriptions1,2,3. During testing, hemodynamic variables and data derived from automatic gas exchange are monitored and analyzed. Cerebral tissue oxygen saturation (SctO2) monitoring has value for grading prognosis and disease severity4,5.
Near-infrared spectroscopy (NIRS) uses infrared light to penetrate the skull and estimate brain tissue oxygenation continuously and non-invasively6. Since oxyhemoglobin and deoxyhemoglobin have different light absorption spectra and are the primary chromophores that absorb light, their concentrations can be measured using light transmission and absorption6,7. However, background light absorbers also scatter light and may influence the measurement8. This study adopted a spatially resolved NIRS to measure SctO2 from rest to peak exercise9. Four wavelengths were emitted to compensate for wavelength-dependent scattering losses and eliminate background interference, thus enhancing accuracy10.
SctO2 represents the proportion of oxygen delivery vs. consumption in cerebral tissue. Cerebral desaturation is associated with disrupted cerebral blood flow (CBF), decreased arterial oxygen concentration, and increased cerebral tissue oxygen consumption11. Other than cardiac output insufficiency, advanced HF causes cerebral hypoperfusion during exercise by indirectly inducing cerebral vasoconstriction via diminishing arterial partial pressure of carbon dioxide (PaCO2) through hyperventilation12.
The clinical significance of cerebral oxygenation in HF was revealed by Chen et al.4. First, SctO2 was significantly decreased in the HF group compared with healthy controls. SctO2 is not only diminished at rest but also declined further during exercise. It is not observed in the healthy group. Second, SctO2rest and SctO2peak were correlated with VO2peak, brain natriuretic peptide (BNP), and oxygen uptake efficiency slope (OUES), all of which are established prognostic markers. Therefore, SctO2rest and SctO2peak are very likely to be prognostic and reflect disease severity in HF patients. Another study by Koike et al. suggested that the change in cerebral oxyhemoglobin measured at the forehead from rest to peak exercise was significantly lower in non-survivors compared to that in survivors of patients with coronary artery disease5. Hence, cerebral oxygenation may be employed to stratify the disease severity and prognosis of patients with HF.
Protocol
The following protocol was approved by the ethics committee in Chang Gung Memorial Hospital, Linkou, Taiwan. The exercise test was carried out in an air-conditioned laboratory with an atmospheric temperature of 22-25 °C, pressure of 755 to 770 Torr, and relative humidity of 55-65%. Before each test, the gas analyzer was calibrated following the manufacturer's instructions using room air and a gas mixture of known concentration (FO2: 0.12; FCO2: 0.05; N2 as balance). The turbine flow meter of the system was calibrated by the 2-point method with 0.2 L/s and 2 L/s by an automatically-pumping system.
1. Preparation: Placement of sensors and recorders
- Clean the forehead twice with an alcohol pad to remove sweat and dirt from the skin.
- Place NIRS sensors on the forehead bilaterally. Use a large sensor in which the distance between emitter and detector is 5 cm. The estimated measuring depth is 2.5 cm. Ensure that the sensors are securely attached.
- Attach patches of electrocardiography to the anterior chest, bilateral acromioclavicular joints, and lower back.
- Have the patient sit on the bicycle ergometer.
- Place the armband of the sphygmomanometer.
- Instruct the patient to wear the mask for the gas analysis. Make sure that no gas leaks through the brim of the mask.
- Place the sensors of the pulse oximeter on the patient's ear lobe and index finger.
2. CPET and SctO2 monitoring
- Tell the patient to rest for at least 2 min to obtain a stable baseline value, including SctO2 and respiratory exchange ratio.
- Have the patient complete the warm-up stage at a work rate of 10 W for 1 min on the cycle ergometer.
- Increase the rate by 10 W/min and ask the patient to pedal at around 60 rpm until failing to keep up with a cadence >50 rpm despite strong encouragement (symptom-limited exercise testing).
- Average the SctO2 value every second automatically from data scanned at the frequency of 100 Hz.
- Measure the blood pressure every 2 min automatically by the sphygmomanometer.
- Analyze the gas component breath by breath, including VO2 and end-tidal carbon dioxide pressure (PETCO2).
- Have the patient complete the recovery stage at a work rate of 0 W for 2-6 min.
Results
Thirty-four HF patients and 17 healthy controls were enrolled at Linkou Chang Gung Memorial Hospital, Taiwan. Each subject underwent cardiopulmonary exercise testing that incorporated SctO2 monitoring by NIRS. Briefly, SctO2 (rest; peak) values were significantly lower in the HF group (66.3 ± 13.3%; 63.4 ± 13.8%,) than in the control (73.1 ± 2.8%; 72 ± 3.2%) group (Figure 1). In the HF group, SctO2 at rest (SctO2rest) and peak SctO2 (SctO2peak) were linearly correlated with brain natriuretic peptide (BNP), VO2peak, and OUES (r of -0.561 to 0.677, p < 0.001) (Figure 2). Notably, SctO2rest was determined by the partial pressure of PETCO2 at rest (PETCO2rest), hemoglobin, and mean arterial pressure at rest (MAPrest) (adjusted R = 0.681, p < 0.05 on stepwise linear regression) (Table 1). The main findings are illustrated in Figure 3.
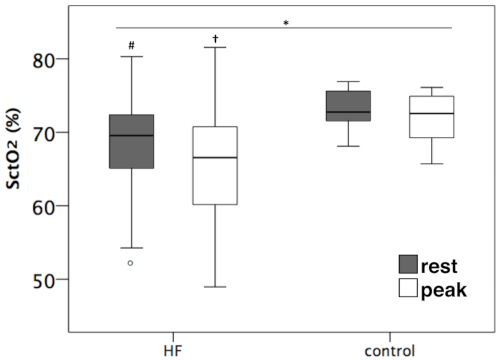
Figure 1: Box plots of SctO2rest and SctO2peak in HF and control groups. Both SctO2 values at rest and peak exercise were significantly lower in the HF group than in the control group. Adapted from Chen et al.4. * p < 0.05, HF vs. control, repeated measure ANOVA. # p < 0.05, SctO2rest HF vs. control, paired t-test. † p < 0.05, SctO2peak HF vs. control, paired t-test. SctO2rest: cerebral tissue oxygen saturation at rest; SctO2peak: cerebral tissue oxygen saturation at peak exercise. Please click here to view a larger version of this figure.
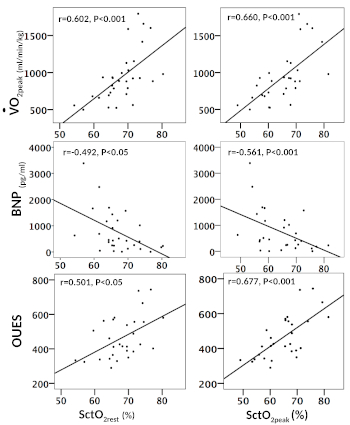
Figure 2: Scatter plots of SctO2rest and SctO2peak versus VO2peak, BNP, and OUES. SctO2rest (left panel) and SctO2peak (right panel) values were linearly correlated with VO2peak, BNP, and OUES. Adapted from Chen et al.4 SctO2: cerebral tissue oxygen saturation; VO2: oxygen consumption; BNP: brain natriuretic peptide; OUES: oxygen uptake efficiency slope. Please click here to view a larger version of this figure.

Figure 3: Illustration of the possible prognostic value of cerebral desaturation and its physiological basis in patients with HF. SctO2, especially at peak exercise, was correlated with VO2peak, BNP, and OUES. SctO2rest was determined by PETCO2rest, hemoglobin, and MAPrest, while the main determinant of SctO2peak was VCO2peak. Please click here to view a larger version of this figure.
| ß | t | P(ß) | R | ΔR2 | F | ||
| Model 1 | 0.593 | 0.352 | 14.679* | ||||
| PETCO2rest | 0.593 | 3.831 | 0.001 | ||||
| Model 2 | 0.639 | 0.056 | 19.257* | ||||
| PETCO2rest | 0.552 | 3.757 | 0.001 | ||||
| Hb | 0.314 | 2.14 | 0.042 | ||||
| Model 3 | 0.681 | 0.056 | 25.009* | ||||
| PETCO2rest | 0.517 | 3.804 | 0.001 | ||||
| Hb | 0.331 | 2.451 | 0.022 | ||||
| MAPrest | 0.323 | 2.398 | 0.024 | ||||
| PETCO2, the end-tidal partial pressures of CO2; Hb, hemoglobin; MAP, mean arterial pressure | |||||||
| * p < 0.05; the p-value indicates the overall significance of the linear regression model | |||||||
| P(ß): p-value for ß; R and ΔR2 are adjusted values | |||||||
Table 1: Stepwise regression of SctO2rest in the HF group. Adapted from Chen et al.4. SctO2: cerebral tissue oxygen saturation. HF: heart failure.
Discussion
Cerebral oxygenation monitored noninvasively and continuously by NIRS has been applied in various scenarios, including cardiovascular surgery13 and brain functional analyses such as those that estimate neural activity14. This protocol integrated NIRS into conventional CPET to identify the involvement of the cerebral hemodynamic response in exercise intolerance in patients with HF. It increases the value of exercise testing in determining prognosis and disease severity.
Cardiac dysfunction was considered the main cause of exercise intolerance in patients with HF15. Nonetheless, clinical studies demonstrated that inotropic or vasodilatory agents failed to increase exercise capacity16, and the association between resting cardiac function and peak oxygen consumption is weak17. Accordingly, cardiac dysfunction is not the sole cause of exercise intolerance in patients with HF.
The decreased cerebral perfusion and oxygenation during exercise have been demonstrated in patients whose cardiac output fail to increase normally18,19, suggesting that the cerebral hypoperfusion is partially caused by the blunted cardiac output increase during exercise. Reduced frontal cortex oxygenation impaired the force-generating capacity of the peripheral working muscle, thus limit the exercise performance20. Moreover, the suppressed cerebral hemodynamics during exercise is associated with ventilatory abnormality, which reduces the functional capacity of patients with HF21. Furthermore, SctO2 is correlated with peak VO2 and OUES as well as BNP, all of which are well-recognized markers for HF severity and prognosis4.
Exertional cerebral hypoperfusion21 is caused by cardiac output insufficiency as well as exertional hyperventilation, which reduces alveolar PCO2 and the subsequent PaCO2, a response that may further induce cerebral vasoconstriction during exercise22,23,24. A previous study showed that PaCO2 is positively linearly correlated with a CBF of 15-60 mmHg25. In fact, it is the main physiologic determinant of SctO24. SctO2 is also affected by hemoglobin and MAP4, influencing arterial oxygen concentration and cerebral perfusion, respectively26,27. One may argue that anemia leads to increased mean optical path length and might influence the validity of SctO2 measurement by NIRS. A previous study has already demonstrated that SctO2 measured by phase-resolved spectroscopy did not alter significantly in response to the change of hemoglobin concentration in a cardiac surgery28.
Despite the high reproducibility and validity of NIRS measurements in the resting state, the validity of this device in the HF population during exercise has not been established. Nonetheless, the different combinations of end-tidal O2 and CO2 were simulated in a previous validation study, which is in part similar to exercise status29. The increase or decrease of skin blood flow at peak exercise in patients with HF might overestimate or underestimate the true value of cerebral oxygenation at the forehead30,31. No matter what, the fact that low SctO2 measured by NIRS on the forehead is a potentially negative prognostic factor based on the present result, has been established, except that the measured SctO2 value not only represents cerebral oxygenation at frontal lobe, but also skin blood flow at forehead to a certain degree. Besides, extracranial melanin may absorb light and thus attenuate the signal, although SctO2 was calculated from the concentration of oxy- and deoxyhemoglobin and is affected less by skin melanin8. Time-resolved spectroscopy - NIRS may solve the above problem to some extent. However, standard NIRS is rather easier for clinical application. Finally, a longitudinal study is required to confirm the prognostic value of SctO2 in patients with HF.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The patient who participated in exercise testing is deeply appreciated. This research was supported by National Science Council, Taiwan (NMRPG3G6231/2/3), Chang Gung Memorial Hospital (Grant No. CMRPG3G0601/2), and Healthy Aging Research Center, Chang Gung University and the Taiwan Ministry of Education's Higher Education Deep Plowing Program (Grant Numbers EMRPD1H0351 and EMRPD1H0551).
Materials
| Name | Company | Catalog Number | Comments |
| Bicycle ergometer | Ergoline, Germany | Ergoselect 150P | |
| Cardiopulmonary exercise testing gas analysis | Cardinal-health Germany | MasterScreen CPX | |
| Finger pulse oximetry | Nonin Onyx, Plymouth, Minnesota | Model 9500 | |
| Sphygmomanometer | SunTech Medical, UK | Tango |
References
- Balady, G. J., et al. Clinician's Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 122 (2), 191-225 (2010).
- Corra, U., et al. Cardiopulmonary exercise testing in systolic heart failure in 2014: the evolving prognostic role: a position paper from the committee on exercise physiology and training of the heart failure association of the ESC. European Journal of Heart Failure. 16 (9), 929-941 (2014).
- Malhotra, R., Bakken, K., D'Elia, E., Lewis, G. D. Cardiopulmonary Exercise Testing in Heart Failure. JACC Heart Fail. 4 (8), 607-616 (2016).
- Chen, Y. J., et al. Cerebral desaturation in heart failure: Potential prognostic value and physiologic basis. PloS One. 13 (4), e0196299 (2018).
- Koike, A., et al. Clinical significance of cerebral oxygenation during exercise in patients with coronary artery disease. Circulation Journal. 72 (11), 1852-1858 (2008).
- Madsen, P. L., Secher, N. H. Near-infrared oximetry of the brain. Progress in Neurobiology. 58 (6), 541-560 (1999).
- Wahr, J. A., Tremper, K. K., Samra, S., Delpy, D. T. Near-infrared spectroscopy: theory and applications. Journal of Cardiothoracic and Vascular Anesthesia. 10 (3), 406-418 (1996).
- Fischer, G. W. Recent advances in application of cerebral oximetry in adult cardiovascular surgery. Seminars in Cardiothoracic and Vascular Anesthesia. 12 (1), 60-69 (2008).
- Benni, P. B., MacLeod, D., Ikeda, K., Lin, H. M. A validation method for near-infrared spectroscopy based tissue oximeters for cerebral and somatic tissue oxygen saturation measurements. Journal of Clinical Monitoring and Computing. 32 (2), 269-284 (2018).
- Strangman, G., Boas, D. A., Sutton, J. P. Non-invasive neuroimaging using near-infrared light. Biological Psychiatry. 52 (7), 679-693 (2002).
- Ide, K., Secher, N. H. Cerebral blood flow and metabolism during exercise. Progress in Neurobiology. 61 (4), 397-414 (2000).
- Immink, R. V., Secher, N. H., van Lieshout, J. J. Cerebral autoregulation and CO2 responsiveness of the brain. American Journal of Physiology: Heart and Circulatory Physiology. 291 (4), H2018 (2006).
- Chan, M. J., Chung, T., Glassford, N. J., Bellomo, R. Near-Infrared Spectroscopy in Adult Cardiac Surgery Patients: A Systematic Review and Meta-Analysis. Journal of Cardiothoracic and Vascular Anesthesia. 31 (4), 1155-1165 (2017).
- Sakudo, A. Near-infrared spectroscopy for medical applications: Current status and future perspectives. Clinica Chimica Acta. 455, 181-188 (2016).
- Crimi, E., Ignarro, L. J., Cacciatore, F., Napoli, C. Mechanisms by which exercise training benefits patients with heart failure. Nature Reviews: Cardiology. 6 (4), 292-300 (2009).
- Pina, I. L., et al. Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation. 107 (8), 1210-1225 (2003).
- Franciosa, J. A., Park, M., Levine, T. B. Lack of correlation between exercise capacity and indexes of resting left ventricular performance in heart failure. American Journal of Cardiology. 47 (1), 33-39 (1981).
- Koike, A., et al. Cerebral oxygenation during exercise and exercise recovery in patients with idiopathic dilated cardiomyopathy. American Journal of Cardiology. 94 (6), 821-824 (2004).
- Koike, A., et al. Cerebral oxygenation during exercise in cardiac patients. Chest. 125 (1), 182-190 (2004).
- Amann, M., et al. Arterial oxygenation influences central motor output and exercise performance via effects on peripheral locomotor muscle fatigue in humans. Journal of Physiology. 575 (Pt 3), 937-952 (2006).
- Fu, T. C., et al. Suppression of cerebral hemodynamics is associated with reduced functional capacity in patients with heart failure. American Journal of Physiology: Heart and Circulatory Physiology. 300 (4), H1545-H1555 (2011).
- Myers, J., et al. The lowest VE/VCO2 ratio during exercise as a predictor of outcomes in patients with heart failure. Journal of Cardiac Failure. 15 (9), 756-762 (2009).
- Wasserman, A. J., Patterson, J. L. The cerebral vascular response to reduction in arterial carbon dioxide tension. Journal of Clinical Investigation. 40, 1297-1303 (1961).
- Ross, A., Marco, G., Jonathan, M. Ventilatory Abnormalities During Exercise in Heart Failure: A Mini Review. Current Respiratory Medicine Reviews. 3 (3), 179-187 (2007).
- Herholz, K., et al. Regional cerebral blood flow in man at rest and during exercise. Journal of Neurology. 234 (1), 9-13 (1987).
- Karlman Wasserman, J. E. H., Sue, D. Y., Stringer, W. W., Whipp, B. J. . Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications. , 285-299 (2011).
- Pott, F., et al. Middle cerebral artery blood velocity during rowing. Acta Physiologica Scandinavica. 160 (3), 251-255 (1997).
- Yoshitani, K., et al. Measurements of optical pathlength using phase-resolved spectroscopy in patients undergoing cardiopulmonary bypass. Anesthesia and Analgesia. 104 (2), 341-346 (2007).
- MacLeod, D. I., Ikeda, K., Cheng, C., Shaw, A. Validation of the Next Generation FORE-SIGHT Elite Tissue Oximeter for Adult Cerebral Tissue Oxygen Saturation. Anesthesia and Analgesia. 116 (SCA Suppl), (2013).
- Davie, S. N., Grocott, H. P. Impact of extracranial contamination on regional cerebral oxygen saturation: a comparison of three cerebral oximetry technologies. Anesthesiology. 116 (4), 834-840 (2012).
- Ogoh, S., et al. A decrease in spatially resolved near-infrared spectroscopy-determined frontal lobe tissue oxygenation by phenylephrine reflects reduced skin blood flow. Anesthesia and Analgesia. 118 (4), 823-829 (2014).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved