Method Article
Murine Aortic Crush Injury: An Efficient In Vivo Model of Smooth Muscle Cell Proliferation and Endothelial Function
In This Article
Summary
Restenosis following cardiovascular procedures (bypass surgery, angioplasty, or stenting) is a significant problem reducing the durability of these procedures. An ideal therapy would inhibit smooth muscle cell (VSMC) proliferation while promoting regeneration of the endothelium. We describe a model for simultaneous assessment of VSMC proliferation and endothelial function in vivo.
Abstract
Arterial reconstruction, whether angioplasty or bypass surgery, involves iatrogenic trauma causing endothelial disruption and vascular smooth muscle cell (VSMC) proliferation. Common murine models study small vessels such as the carotid and femoral arteries. Herein we describe an in vivo system in which both VSMC proliferation and endothelial barrier function can be simultaneously assessed in a large vessel. We studied the infrarenal aortic response to injury in C57BL/6 mice. The aorta was injured from the left renal vein to the aortic bifurcation by 30 transmural crushes of 5-seconds duration with a cotton-tipped applicator. Morphological changes were assessed with conventional histology. Aorta wall thickness was measured from the luminal surface to the adventitia. EdU integration and counter staining with DAPI and alpha-actin was used to demonstrate VSMC proliferation. Activation of ERK1/2, a known moderator of intimal hyperplasia formation, was determined by Western Blot analysis. The effect of inflammation was determined by immunohistochemistry for B-cells, T-cells, and macrophages. En face sections of endothelium were visualized with scanning electron microscopy (SEM). Endothelial barrier function was determined with Evans Blue staining. Transmural injury resulted in aortic wall thickening. This injury induced VSMC proliferation, most prominently at 3 days after injury, and early activation of ERK1/2 and decreased p27kip1 expression. Injury did not result in increased B-cells, T-cells, or macrophages infiltration in the vessel wall. Injury caused partial endothelial cell denudation and loss of cell-cell contact. Injury resulted in a significant loss of endothelial barrier function, which returned to baseline after seven days. The murine transmural blunt aortic injury model provides an efficient system to simultaneously study both VSMC proliferation and endothelial barrier function in a large vessel.
Introduction
Restenosis following cardiovascular procedures (bypass surgery, angioplasty, or stenting) is a significant problem reducing the durability of these procedures. All revascularization procedures are plagued by restenosis. Present strategies to prevent restenosis (drug-eluting stents and drug-coated balloons) inhibit both vascular smooth muscle cell (VSMC) and endothelial cell proliferation (EC). Consequently, these interventions prevent VSMC mediated restenosis, but also prevent the regeneration of the endothelium. Without an intact endothelium, patients are required to be on potent antiplatelet agents to decrease the risk of in situ thrombosis at the risk of bleeding complications. An ideal therapy would inhibit VSMC proliferation while promoting regeneration of the endothelium. Thus, there is a need to simultaneously study VSMC proliferation and endothelial barrier function in vivo.
Presently, there are several mouse models of restenosis 1. These models include carotid ligation and femoral artery wire injury 2. Aortic models include stent placement 3, balloon injury 4, and aortic allograft 5. All of the present models are limited. Carotid ligation generates a flow-mediated neointimal lesion and does not have endothelial injury. Additionally, both carotid and femoral arteries have many fold fewer cell layers than human vessels, limiting their translational value. The mouse aorta which is approximately 1.3 mm in diameter, is the only vessel that approximates a clinically relevant (coronary) human artery (3).
Despite the translational potential of murine aortic models of disease, current models have limitations. These models require advanced microsurgical skills and specialized equipment such as angioplasty balloons and stents. Herein, we present a novel, reproducible technique to simultaneously induce VSMC proliferation and disrupt endothelial barrier function.
Protocol
Ethics Statement: The protocols for animal handling were approved by the Institutional Animal Care and Use Committee (IACUC) of the University of Maryland (protocol number 0416009) and conducted according to AAALAC-International standards.
1. Surgical Procedure
- Anesthetic Technique
- Sterilize all instruments used in survival surgery with steam sterilization at 121 °C for 30 min.
- Induce anesthesia via an induction tank with 100% O2 and 2.5% isoflurane delivered via precision vaporizer. Post-induction, discontinue the isoflurane and flush the chamber with O2. Maintain anesthesia with 1.5-2% isoflurane via face mask and 1 L/min O2 by inhalation.
- Attach both the induction chamber and the face mask to a charcoal scavenger for waste gas adsorption to protect personnel. Ensure an adequate anesthetic plane by demonstrating that there is no response to noxious stimuli (toe pinch).
- Create an operative field consisting of a surgical tray with isothermal pad to provide thermal support during surgery. An additional isothermal pad will provide thermal support to animals in their recovery cage.
- Animal Preparation
- Carry out the following investigation on 10-12 weeks old male C57BL/6 mice.
- Remove the hair on the ventral abdominal surface of the animal from the sternum to the inguinal region with a depilatory agent or an electrical clipper with a number 40 blade.
- In case of depilatory agent, apply this compound to the surgical area for 2-3 min and then remove it with cotton. We use a commercially available compound of calcium hydroxide and sodium hydroxide.
- Prep the area over the shoulder with 70% alcohol and subcutaneously inject carprofen (5 mg/kg) with a 25 gauge or smaller bore needle. This treatment will provide postoperative analgesia for the animal.
- Transfer the animal to the surgical field and position in dorsal recumbency.
- Prepare the surgical site by scrubbing 8-12% providone-iodine with a clean cotton applicator or cotton gauze. Then rinse the skin twice with 70% alcohol.
- Place ocular lubricant in both eyes to reduce the incidence of corneal desiccation. Cover the surgical site with a sterile drape.
- Operative Technique
- Make a median abdominal laparotomy incision approximately 2-2.5 cm in length with a scalpel beginning immediately caudal the xiphoid process and extending towards the pelvis.
- Mobilize the small bowel and duodenum and reflect laterally to the right. Roll up a strip of sterile cotton gauzed and soaked with sterile saline for injection to allow packing of the viscera to improve exposure.
- With the small intestine mobilized to the right side of the abdomen, expose the retroperitoneum and expose the abdominal aorta from the left renal vein to the aortic bifurcation (Figure 1).
- With a sterile cotton-tipped applicator, deliver 30 consecutive crushes, each five seconds in duration.
- Remove the packing and allow the viscera to return to their native position.
- Close fascia with a running 4-0 absorbable monofilament suture (polydioxanone). Skin is closed with a running 6-0 non-absorbable monofilament suture (nylon).
- Recovery and Post-Procedure Care
- After the procedure, place the animal in a recovery cage with clean bedding on an isothermal pad to continue thermal support until the animal is able to ambulate normally. Do not leave the animal unattended until it demonstrates the ability to maintain sternal recumbency.
- Monitor the animal every hour for the first 4 h after surgery. Once the animal is ambulating normally return it to the assigned husbandry room. The animal will not be housed in the company of another animal until it has fully recovered.
- Monitor the animal twice daily for the first 72 h after surgery and at least 3 times a week thereafter. Monitoring includes weighing the animal three times a week.
- Administer carpofen (5 mg/kg) subcutaneously twice daily for the first 72 h after surgery.
2. Procurement of Tissue
- Method of Euthanasia
- Euthanize the animals at predetermined time points.
- Induce anesthesia via an induction tank with 100% O2 and 2.5% isoflurane delivered via precision vaporizer.
- To study the integrity of the endothelium, Administer Evans Blue dye to the animal.
NOTE: Evans Blue is a negatively charged azo dye with a high binding affinity for albumin and can only stain blood vessels in the absence of an intact endothelium6. - For endothelial integrity studies, at the time of euthanasia, perfuse the animals with 5 mL of 0.3 % Evans Blue dye followed by 5 mL PBS at physiological pressure for 5 min. The animal is maintained in a surgical plane of anesthesia during the perfusion procedure.
- To study the integrity of the endothelium, Administer Evans Blue dye to the animal.
- After achieving a deep anesthetic plane, open the chest with a sternotomy. Make a laceration in the right atrium to allow drainage of blood from the animal and access the left ventricle is accessed with a 21 G needle and inject phosphate buffered saline (PBS) until the effluent from the right atrium is clear.
- After perfusion with PBS, enter the abdomen through a midline incision.
- Once again, mobilize the small intestine to the right side of the abdomen exposing the infrarenal aorta, sharply dissect the aorta from adjacent tissues and excise it from the left renal vein to the aortic bifurcation.
- Store the excised aorta in a 4% paraformaldehyde solution until tissue processing occurs.
- For endothelial integrity studies, open the aorta longitudinally and pin it to a wax sheet exposing the entirety of the luminal surface6. Carry out a qualitative assessment of endothelial integrity by the degree of staining with Evans Blue dye6.
- For other histologic assays, section the aorta transversely and embed it in optimal cutting temperature (OCT) compounds as dictated by the histological method to be used 7.
Results
Transverse sections aorta embedded in OCT were sectioned, and stained with hematoxylin and eosin then counter stained with Verhoeff-Van Gieson (VVG) stain to identify the internal and external elastic lamina 7. Crush injury induced aortic wall thickening compared to the aortas of animals treated with a sham procedure (laparotomy and small bowel mobilization alone). Wall thickness, as assessed by the distance from adventitia to the lumen, was greatest three days after injury (42.2 ± 1.7 µm vs. 22.1 ± 1.1 µm for laparotomy alone) (Figure 2A-B). Injury resulted in the cells having a more rounded appearance and an irregular contour of the luminal surface (Figure 2C).
Increased wall thickening of the injured aorta is at least in part mediated by increased proliferation of medial vascular smooth muscle cells. To prove that wall thickening is due to increased proliferation as opposed to cell hypertrophy, we used an EdU proliferation assay. In this assay, the thymidine analogue 5-ethynyl-2'-deoxyuridine (EdU) is administered intravenously to the mouse 24 h prior to euthanasia. EdU is incorporated into DNA during synthesis. EdU is detected by a click reaction (copper-catalyzed azide-alkyne cycloaddition using green-fluorescent dye) 8. Sham mice exposed only to laparotomy had no observed fluorescence in any layer of the aorta. Conversley, mice subjected to aortic injury demonstrated fluorescence in both the media and intima of the aorta (Figure 3).
Aortic wall thickening after crush injury activates cell signaling pathways implicated in restenosis in humans. The mitogen-activated protein kinase (MAP Kinase) ERK1/2 is one of the principle mediators of intimal hyperplasia formation In response to stimulation from a mitogen, ERK1/2 is phosphorylated and activated 9,10. Data from our laboratory have also demonstrated that the cyclin-dependant kinase inhibitor p27kip1 is decreased in response to mitogenic stimuli in the vessel wall12. Mice were euthanized at 1, 3, 7 days, and 1 month after aortic crush injury. The infrarenal aorta was isolated and protein expression of ERK1/2, phospho-ERK1/2 (the activated form of ERK1/2), and the cyclin dependent kinase inhibitor p27kip1 were determined by Western blot analysis (Figure 4A). No change was observed in total ERK1/2 protein expression over time. However, three days after injury, phospho-ERK1/2 (Pi-ERK1/2) expression was over 200% greater than baseline Pi-ERK1/2 expression. p27kip1 expression decreased at early time points and reached a nadir of approximately 20% of baseline seven days after injury. Both Pi-ERK1/2 and p27kip1 expression approximated baseline levels one month after injury (Figure 4B). Thus the observed thickening of the aortic wall is at least in part due to increased medial proliferation.
The aortic injury model allows simultaneous assessment of both medial smooth muscle proliferation and endothelial barrier function. Scanning electron microscopy (SEM) was used to characterize the effect of the crush injury on the morphology of the endothelium. The luminal surface of the aorta is lined by a confluent, endothelium that prevents adhesion of blood-born cells and molecules (Figure 5A, Scale bar = 100 µm). In contrast, crush injury results in disruption of endothelial cells and partial denudation of the endothelium (Figure 5B, Scale bar = 100 µm). As seen at higher magnification, disruption of the endothelium results in adhesion of particles consistent in size and shape with platelets. Adhesion of these particles occurs throughout the entire zone of injury, and is not limited to areas of gross denudation observed at lower magnification (Figure 5C, Scale bar = 50 µm). The morphology of the adherent particle is best observed at higher magnification. These particles are consistent with platelets and fibrin (Figure 5D, Scale bar = 10 µm).
In addition to endothelial morphology, the barrier function of the endothelium can be assessed with this model of vascular injury. The azo dye Evans Blue cannot permeate the normal, intact endothelium of the murine aorta. Damage to the barrier function of the endothelium allows staining of the basement membrane with Evans Blue. Mice treated to a laparotomy alone (sham) maintained the barrier function of the endothelium and these aortas were white. Crush injury resulted in a diffuse loss of endothelial barrier function and these aortas stained dark blue. The intensity of staining with Evans Blue was decreased three days after crush injury, and full barrier function was restored on week after injury (Figure 6A). Endothelial barrier function can be further quantitated by weighing the samples and homogenizing in 10-fold volume of 50% trichloroacetic acid solution. Diluting the supernatant in 4-fold ethanol allows for determination of fluorescence intensity (excitation 620 nm and emission 680 nm) as described by Aoki et al.11. The amount of Evans Blue eluted from the infrarenal aorta was over three-fold higher in aortas immediately after injury compared to aortas subjected only to laparotomy (Injured - Day 0). The aorta continued to stain with Evans Blue at one and three days after injury, but less intensely than at the time of injury, suggesting a gradual recovery of endothelial barrier function. One week after injury the injured aorta had equivalent staining as an aorta treated with laparotomy alone (Figure 6B).
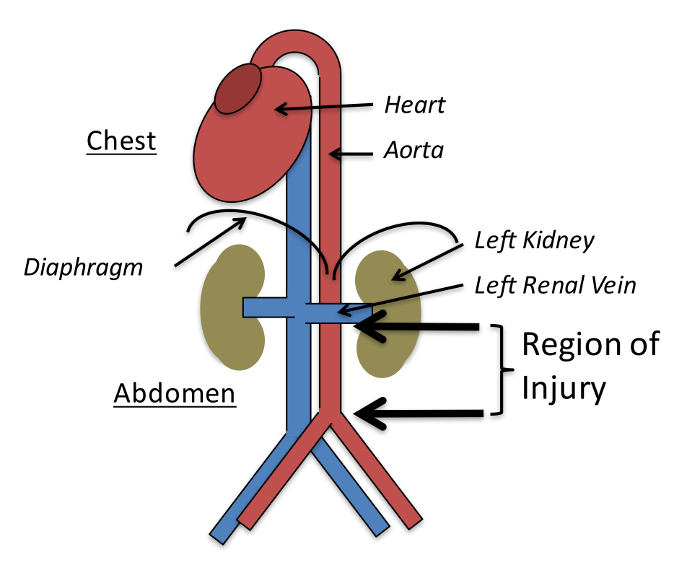
Figure 1: Injury is Created by Bluntly Crushing the Aorta from the Left Renal Vein to the Aortic Bifurcation. Figure adapted with permission from Yu et al., PLoS One 2015 12. Please click here to view a larger version of this figure.
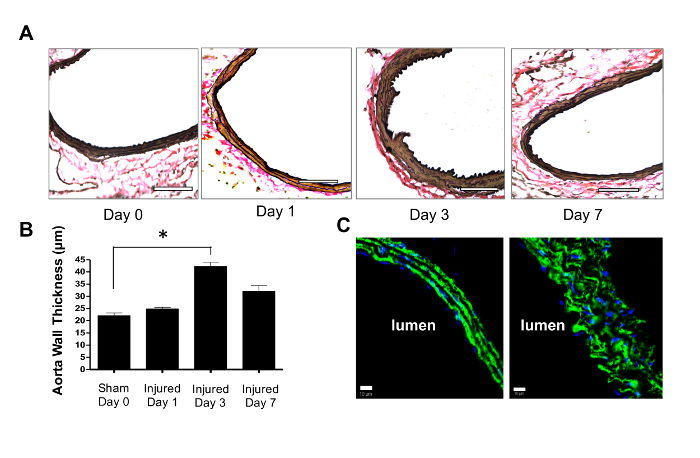
Figure 2: Crush Injury Induces Aortic Wall Thickening. (A) Crush injury induced morphological changes in the aorta. Representative 5 µm cross sections were stained with VVG at 0, 1, 3 and 7 days after injury. Scale bars = 100 µm. (B) Wall thickness was greatest 3 days after injury, 42.2 ± 1.7 µm, and was significantly greater than the aorta of sham animals exposed to laparotomy alone, 22.1 ± 1.1 µm. Statistical significance was determined with the Student's two-tail t-test. * Denotes p <0.05, n = 3. (C) Crush injury induced a rounded appearance of medial VSMCs (stained in green for α-smooth muscle actin) and changing cell orientation. Nuclei were counterstained with DAPI (Blue). Scale bars = 10 µm. Data are presented as means and standard deviations. Please click here to view a larger version of this figure.
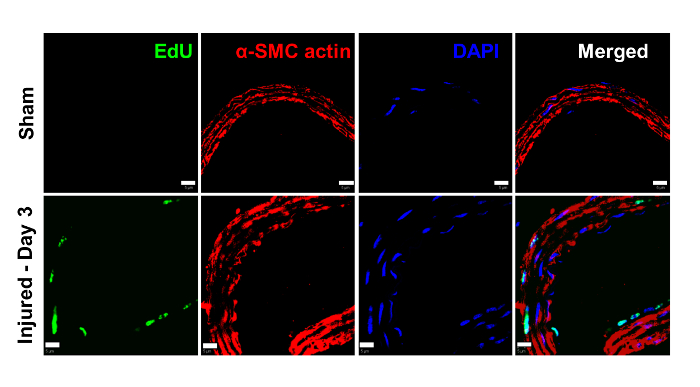
Figure 3: Crush Injury Induces Cell Proliferation in the Aortic Wall. Mice were exposed to either laparotomy alone (sham) or laparotomy with aortic crush injury. Thymidine analogue 5-ethynyl-2'-deoxyuridine (EdU) was administered 24 h prior to euthanasia. EdU is incorporated into DNA during synthesis. EdU is detected by a click reaction (copper-catalyzed azide-alkyne cycloaddition using green-fluorescent dye). There was no detectable EdU (green) in the aortic wall of the sham animals. In the animals subjected to crush injury, EdU stained prominently in the media of the aorta and to a somewhat lesser degree in the intima. Vascular smooth muscle cells were identified by staining with α-smooth muscle actin antibody (red). This finding suggests that the observed wall thickening observed in Figure 2 is due to an increase in cell proliferation. Scale bars = 10 µm. Please click here to view a larger version of this figure.
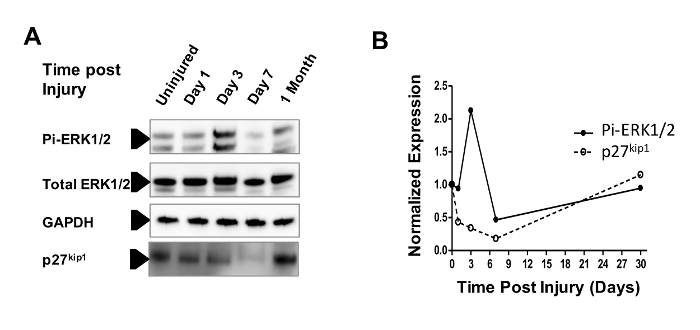
Figure 4: The Mitogen-activated Protein Kinase (MAP Kinase) Pathway is Activated in Response to Crush Injury. (A) The MAP Kinase ERK1/2 is phosphorylated when activated and is associated with intimal hyperplasia and restenosis. Mice were euthanized at 1, 3, 7 days, and 1 month after aortic crush injury. Western blot analysis was used to assess protein expression of total ERK1/2, phospho-ERK1/2, and the cyclin dependent kinase inhibitor p27kip1. Protein expression was normalized to a sham animal treated with laparotomy alone. (B) No change was observed in total ERK1/2 protein expression over time. However, three days after injury, phospho-ERK1/2 (Pi-ERK1/2) expression was over 200% greater than baseline Pi-ERK1/2 expression. p27kip1 expression decreased at early time points and reached a nadir of approximately 20% of baseline seven days after injury. Both Pi-ERK1/2 and p27kip1 expression approximated baseline levels one month after injury. Please click here to view a larger version of this figure.
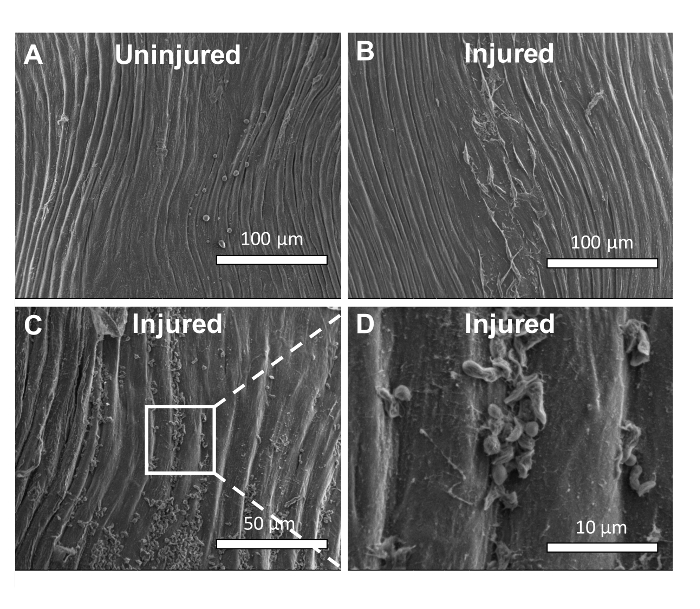
Figure 5. Crush Injury Disrupts Aortic Endothelial Cells. (A) Scanning electron microscopy (SEM) was used to characterize the effect of the crush injury on the morphology of the endothelium. The luminal surface of the normal aorta is lined by a confluent, endothelium that prevents adhesion of blood born cells and molecules. (B) Crush injury results in the disruption of endothelial cells and partial denudation of the endothelium. (C) As seen at higher magnification, disruption of the endothelium results in adhesion of particles consistent in size and shape with platelets. Adhesion of these particles occurs throughout the entire zone of injury, and is not limited to areas of gross denudation observed at lower magnification. (D) At higher magnification, these particles are consistent with platelets and fibrin. Please click here to view a larger version of this figure.

Figure 6: The Blunt Aortic Injury Allows Quantification of Endothelial Barrier Function. (A) Damage to the barrier function of the endothelium allows staining of the basement membrane with Evans Blue dye. Mice treated to a laparotomy alone (sham) maintained the barrier function of the endothelium and these aortas were white. Crush injury resulted in a diffuse loss of endothelial barrier function and these aortas stained dark blue. The intensity of staining with Evans Blue was decreased three days after crush injury, and full barrier function was restored on week after injury. (B) Binding of Evans Blue to the infrarenal aorta was quantitated by eluting Evans Blue from the specimen and quantification by fluorescence intensity. Data are presented as means and standard deviations. The most Evans Blue was eluted from the aorta immediately after crush injury. The at the time of injury, the aorta bound over three-fold times more Evans Blue than the aorta subjected to laparotomy alone. As the aorta was allowed to recover, there was less binding at one and three days after injury. One week after injury, the aorta bound the same amount of Evans Blue as the aortas subjected to laparotomy alone. Statistical significance was determined with the Student's two-tail t-test. * denotes p <0.05, n = 3, NS denotes not significant. Please click here to view a larger version of this figure.
Discussion
We have characterized the effects of a murine aortic injury model that results in medial hyperplasia and endothelial barrier dysfunction. Partial EC detachment along the aorta intima accompanied the loss of cell-cell contact and enhancement of cell protrusions. Correspondingly, endothelial barrier function was significantly impaired, which stimulated the mitogen-sensitive signaling pathways, leading to proliferation of VSMCs and thickening of the vessel wall. The strengths of this model is that it is technically easier to learn and execute than other aortic models of disease and allows for simultaneous assessment of both the proliferative response to injury and endothelial function. The critical step in this protocol is the actual crush injury. Variability in the extent of the crush injury could result in varying degrees of injury and thus variable amounts smooth muscle cell proliferation. One step that reduces this variability in our laboratory is to have one scientist, blinded to the treatment or experimental condition, perform all of the crush injuries.
A limitation of this model is its generalizability to clinically relevant human disease processes. Despite the early robust proliferative response of VSMCs in this model, it does not model the late events of restenosis, i.e. no neointima developed. Decreased inflammatory mediators such as cytokines might regulate this process. This finding could be due to the rapid recovery of the endothelium from a partial injury. Similar to a previously reported vascular crush injury model in rabbits 13, infiltration of immune cells was minor. In the present investigation we evaluated profile of inflammatory cytokines the sham animals and aortic injury animals with the profiler array. However, there was no significant difference in the cytokine profile that would explain the difference in the proliferative response between sham and injured animals (data not shown). The injury described in the present report is temporally limited. Whereas other models of aortic injury and intimal hyperplasia such as the aortic angioplasty model completely denudes the endothelium, the present model only partially denudes the aorta. Complete denudation of the endothelium requires significantly longer to recover and these animals experience the effects of injury for a longer period of time.
This model produces a rapid response of VSMCs and ECs to injury allowing quantification of morphological and biochemical changes in one week. It is more efficient than other models that take 14-28 days before the effect of intervention is evident. This model uses the murine aorta which is the only murine vessel that approximates a clinically relevant human vessel. The significant advantage of this technique compared to other aortic models is that this model is relatively easy to learn, and does not require expensive or difficult to obtain equipment 2,3,4,5. In conclusion, the murine aortic crush injury model provides a technically straightforward, inexpensive, efficient in vivo platform to simultaneously evaluate the response of VSMCs and ECs to vascular injury.
Disclosures
This work was funded by the Department of Veterans Affairs Career Development Award (1IK2BX001553-01) (TSM) and the Vascular Cures E. J. Wylie Scholarship (TSM).
Acknowledgements
We thank Hsia Ru-ching PhD, from the Electron Microscopy Core Facility of University of Maryland School of Medicine, for her technical support in processing the scanning electronic microscopy samples.
Materials
| Name | Company | Catalog Number | Comments |
| Ocular lubricant | Dechra | 17033-211-38 | Pharmaceutical agents |
| Isoflurane | VetOne | 502017 | Pharmaceutical agents |
| Carprofen | Zoetis | 26357 | Pharmaceutical agents |
| Precision vaporizer | Summit Medical | 10675 | Surgical supplies |
| Charcoal scavenger | Bickford Inc. | 80120 | Surgical supplies |
| Isothermal pad | Harvard Apparatus | 50-7053-R | Surgical supplies |
| Sterile cotton-tipped applicator | Fisher Scientific | 23-400-124 | Surgical supplies |
| 4-0 absorbable monofilament suture | Ethicon, Inc | J310 | Surgical supplies |
| 5-0 non-absorbable monofilament suture | Ethicon,Inc | 1666 | Surgical supplies |
| 21-gauge x 1 inch needle | BD Biosciences | 305165 | Surgical supplies |
| 25-gauge x 1 inch needle | BD Biosciences | 305125 | Surgical supplies |
| Dry sterilizer | Cellpoint | 7770 | Surgical supplies |
| Fine scissors | Fine Science Tools | 14058-09 | Surgical instruments |
| Adson forceps | Fine Science Tools | 11006-12 | Surgical instruments |
| Dumont #5 fine forceps | Fine Science Tools | 11254-20 | Surgical instruments |
| Vannas Spring Scissors 3 mm cutting edge | Fine Science Tools | 15000-00 | Surgical instruments |
| Needle driver | Fine Science Tools | 91201-13 | Surgical instruments |
| Scalpel handle #4 | Fine Science Tools | 10004-13 | Surgical instruments |
| Scalpel blades #10 | Fine Science Tools | 10010-00 | Surgical instruments |
| PBS | Lonza | 17-516F | Reagents for tissue processing |
| Evans Blue | Sigma-Aldrich | E2129 | Reagents for tissue processing |
| Paraformaldehyde | Sigma-Aldrich | P6148 | Reagents for tissue processing |
| Modeling wax | Bego | 40001 | Reagents for tissue processing |
| OCT compound | Tissue-Tek Sakura | 4583 | Reagents for tissue processing |
| Mayer's hematoxylin solution | Sigma-Aldrich | MHS16 | Reagents for immunohistological analysis |
| Eosin Y solution alcoholic | Sigma-Aldrich | HT110316 | Reagents for immunohistological analysis |
| Elastin stain kit | Sigma-Aldrich | HT25A | Reagents for immunohistological analysis |
| Click-it Edu Alexa-488 Imaging Kit | Invitrogen | C10337 | Reagents for immunohistological analysis |
| Anti-Erk1/2 antibody | Cell Signaling Technology | 4695 | Reagents for immunohistological analysis |
| Anti-phospho-Erk1/2 antibody | Cell Signaling Technology | 4370 | Reagents for immunohistological analysis |
| Anti-p27kip1 antibody | Cell Signaling Technology | 3698 | Reagents for immunohistological analysis |
| Trichloroacetic acid | Sigma-Aldrich | T9159 | Reagents for immunohistological analysis |
References
- Carmeliet, P. Mechanisms of angiogenesis and arteriogenesis. Nat Med. 6 (4), 389-395 (2000).
- Carmeliet, P., Moons, L., Collen, D. Mouse models of angiogenesis, arterial stenosis, atherosclerosis and hemostasis. Cardiovasc Res. 39 (1), 8-33 (1998).
- Baker, A. B., et al. Heparanase Alters Arterial Structure, Mechanics, and Repair Following Endovascular Stenting in Mice. Circ Res. 104 (3), 380-387 (2009).
- Petrov, L., Laurila, H., Hayry, P., Vamvakopoulos, J. E. A mouse model of aortic angioplasty for genomic studies of neointimal hyperplasia. J Vasc Res. 42 (4), 292-300 (2005).
- Li, J., et al. Vascular smooth muscle cells of recipient origin mediate intimal expansion after aortic allotransplantation in mice. Am J Path. 158 (6), 1943-1947 (2001).
- Radu, M., Chernoff, J. An in vivo assay to test blood vessel permeability. J Vis Exp. (73), e50062 (2013).
- Turbett, G. R., Sellner, L. N. The use of optimal cutting temperature compound can inhibit amplification by polymerase chain reaction. Diagn Mol Pathol. 6 (5), 298-303 (1997).
- Puchtler, H., Waldrop, F. S. On the mechanism of Verhoeff's elastica stain: a convenient stain for myelin sheaths. Histochem. 62 (3), 233-247 (1979).
- Salic, A., Mitchison, T. J. A chemical method for fast and sensitive detection of DNA synthesis in vivo. Proc Natl Acad Sci U S A. 105 (7), 2415-2420 (2008).
- Nelson, P. R., Yamamura, S., Mureebe, L., Itoh, H., Kent, K. C. Smooth muscle cell migration and proliferation are mediated by distinct phases of activation of the intracellular messenger mitogen-activated protein kinase. J Vasc Surg. 27 (1), 117-125 (1998).
- Rzucidlo, E. M. Signaling pathways regulating vascular smooth muscle cell differentiation. Vascular. 17, S15-S20 (2009).
- Aoki, T., Sumii, T., Mori, T., Wang, X., Lo, E. H. Blood-brain barrier disruption and matrix metalloproteinase-9 expression during reperfusion injury: mechanical versus embolic focal ischemia in spontaneously hypertensive rats. Stroke. 33 (11), 2711-2717 (2002).
- Yu, D., et al. MARCKS Signaling Differentially Regulates Vascular Smooth Muscle and Endothelial Cell Proliferation through a KIS-, p27kip1- Dependent Mechanism. PLoS One. 10 (11), e0141397 (2015).
- Banai, S., et al. Rabbit ear model of injury-induced arterial smooth-muscle cell-proliferation - kinetics, reproducibility, and implications. Circ Res. 69 (3), 748-756 (1991).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved