Method Article
Neuromuscular Ultrasound of the Median Nerve at the Carpal Tunnel
In This Article
Summary
The present protocol describes a technique for the standardization of median nerve ultrasound in cases of suspected carpal tunnel syndrome.
Abstract
The use of neuromuscular ultrasound greatly enhances the evaluation of carpal tunnel syndrome as an adjunct diagnostic tool as it provides dynamic and structural information about the median nerve and its surrounding anatomy. Neuromuscular ultrasound aids in diagnostic accuracy (when used with electrodiagnostic testing) and offers etiologic information as a non-invasive, painless, cost-effective, and radiation-free imaging technology that can be easily carried out at the bedside for immediate interpretation. Neuromuscular ultrasound has the limitation of subjectivity, and the need for training and experience will affect the interpretation of results. This article describes a basic practical guide to visualizing the median nerve using neuromuscular ultrasound in a step-by-step manner to aid in the evaluation of carpal tunnel syndrome. Even though the use of ultrasound in the assessment of median nerve entrapment has been long established, there has been no recognized standard protocol. The present protocol aims to provide clear and concise instructions to describe a standard technique to visualize the median nerve through diagnostic ultrasound.
Introduction
Neuromuscular ultrasound (NMUS) is an increasingly popular method that may be used in conjunction with electrodiagnostic and clinical information in order to diagnose, prognosticate, and guide injection procedures in patients with neuromuscular conditions1. Anatomical structures such as nerves, muscles, bones, and tendons can be identified with high-resolution ultrasound that can refine a diagnosis and provide structural etiology when present. Visualizing the median nerve in the carpal tunnel space-the site of the most common entrapment neuropathy-is one of the most mainstream uses of neuromuscular ultrasound. The rationale for this technique is based on evidence that NMUS is an accurate procedure that may help localize median nerve pathology and guide procedural interventions1,2,3,4. A recent expert consensus found that using both neuromuscular ultrasound and electrodiagnostic study for median nerve pathology is the superior method as opposed to either method alone5. The consensus also describes patient scenarios where the addition of median nerve ultrasound is advantageous for non-localizing or normal electrodiagnostic in the setting of clinical carpal tunnel symptoms, atypical electrodiagnostic, failed CTS surgery, and carpal tunnel syndrome due to a structural abnormality5.
General advantages to the use of NMUS include that it is a non-invasive bedside test that is low cost compared to other diagnostic options, well-tolerated, and can provide important morphologic information that is not uncovered when using other modalities. NMUS evaluation has been shown to be a useful tool in redirecting management strategies in patients6,7,8,9,10,11,12,13.
While there is currently no standard technique for visualization of the median nerve in the carpal tunnel space with ultrasound, there are widely accepted recommendations on how to approach imaging. Through the described procedure, the goal is to establish a clinical reference that clinicians may use to obtainconsistent, high-quality images and measurements. Limitations to this technique include having the proper equipment, including a high-frequency (15 to 22 MHz) linear array transducer used to evaluate the median nerve in two distinct planes. Another limitation to this technique will be proper clinical experience, as it is important to understand the anatomical positioning of the transducer prior to evaluating the nerve, so that correct interpretation of the landmarks is achieved. The present protocol describes the steps of clinical imaging of the median nerve and evaluation of median nerve entrapment.
Protocol
The protocol follows the guidelines of the Wake Forest School of Medicine Research and Ethics committee, and informed written consent was obtained following IRB approval prior to imaging. Any patient with carpal tunnel syndrome who had abnormal nerve conduction studies of the median nerve was appropriate for ultrasound imaging. Individuals with no symptoms of carpal tunnel and normal nerve conduction studies were excluded from the study. A high-end multi-purpose ultrasound machine, equipped with a 15 MHz linear array transducer (see Table of Materials) was used in the present study.
1. Visualizing the median nerve at the distal wrist crease (DWC)
- Ask the patient to sit facing the examiner with their palms upward, fingers semi extended, resting on a pillow or flat surface, and forearms semi flexed at 90°. If the patient cannot sit upright for extended periods, place them in the supine position.
- Ensure the ultrasound machine is turned on, apply a generous amount of gel to the transducer, and position it at the DWC. Hold the probe at the base and keep it perpendicular to the nerve's long axis, maintaining the wrist in a neutral position when beginning scanning.
- Before scanning, check the settings to ensure that there is optimum contrast between the nerve and the surrounding structures by adjusting the gain. Keep the focal point position at the level of the median nerve and the depth to a minimum to allow for better imaging of the median nerve.
NOTE: Continue to adjust these settings while tracing the path of the median nerve. - Begin the scan proximally and distally to find the point of maximal enlargement of the median nerve at the DWC, which approximates the carpal tunnel inlet where the median nerve lies anterior to the flexor tendons and is at the level of the pisiform bone and scaphoid (radial landmark) (Figure 1A) to obtain a cross-sectional view of the median nerve.
- Continue to scan the surrounding structures to evaluate for potential anatomical abnormalities such as bifid nerves, ganglion cysts, lipomas, etc.
2. Evaluation of the median nerve at the DWC
- Obtain a cross-sectional area (CSA) measurement at the site of maximal nerve enlargement in mm2 by using the trace tool as the preferred measuring modality. If not available, then use the elliptical measuring tool on the ultrasound machine and compare this measurement to the local reference values.
NOTE: This may be more accurate than using a specific anatomical landmark to obtain a measurement14. When the transducer is angled perpendicular to the nerve instead of parallel, it minimizes the overestimation of the cross-sectional area and helps avoid anisotropy or changes in echogenicity by changing the angle of the transducer. - Check the measurement of the inner epineural hyperechoic rim of the median nerve to avoid over measurement of the median nerve (Figure 2A).
- Assess median nerve mobility by asking the patient to flex and extend their fingers and wrist while holding the transducer in place in the transverse view.
NOTE: Mobility of the nerve is qualitatively graded based on the range of movement of the nerve in relation to the surrounding flexor tendons15. A diseased nerve will demonstrate little to no mobility. - Note the echotexture of the nerve, as a normal nerve is hypoechoic and surrounded by echogenic connective tissue.
- Press the color doppler flow button of the ultrasound machine to evaluate the blood flow in the median nerve at the wrist.
3. Visualizing the median nerve in the forearm
- Continue to center the median nerve in the ultrasound screen and slowly move the transducer proximally from the wrist to the distal 1/3 of the forearm, keeping the median nerve within sight at approximately halfway up the forearm (Figure 1B).
NOTE: In this location, the median nerve takes on a more triangular appearance and lies deep to the flexor digitorum superficialis muscles and superficial to the flexor digitorum profundus muscle (Figure 2C). - Turn the transducer 90 degrees and align with the third digit and the thenar crease to obtain a sagittal view of the median nerve (Figure 1C). Note the appearance of any focal narrowing or enlargement (Figure 2B).
4. Evaluation of the median nerve in the forearm
- Obtain a cross-sectional area measurement at the forearm in mm2 by using the ultrasound machine's trace or elliptical measuring tool and compare this measurement to local reference values. Ensure measurement of the inner epineural hyperechoic rim of the median nerve.
NOTE: This measurement is gathered to calculate a wrist/forearm ratio which can be useful if the CSA is normal or borderline in the wrist.

Figure 1: Visualizing the median nerve. (A) The patient is seated for median nerve ultrasound, and the ultrasound probe is in the cross-sectional wrist view. (B) The patient is sitting for median nerve ultrasound, and the ultrasound probe is in the cross-sectional forearm view. (C) The ultrasound probe is in the sagittal view, with the probe flipped in the long access orientation. Please click here to view a larger version of this figure.
Results
Typical appearance of a peripheral nerve on the ultrasound
Peripheral nerves consist of hypoechoic (dark) nerve fascicles surrounded by a thick hyperechoic rim of the epineurium. Each nerve fascicle is also surrounded by a thin layer of hyperechoic perineurium, giving rise to a honeycomb appearance in the peripheral nerve in the cross-sectional view (Figure 2A). In the sagittal view, peripheral nerves demonstrate an uninterrupted fascicular pattern with alternating hypoechoic and hyperechoic bands (Figure 2B).
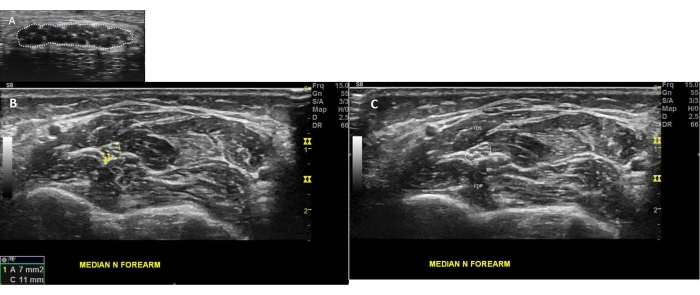
Figure 2: Typical appearance of a peripheral nerve on the ultrasound. (A) The normal median nerve (MN) cross-sectional area at the wrist is outlined with the trace tool. Note the appearance of fascicles within the MN and the honeycomb appearance. (B) The (MN) is seen in the cross-sectional view at the level of the forearm. (C) The (MN) is visualized at the forearm in the cross sectional view. note the Flexor digitorum superficialis (FDS) superficial to the MN and the flexor digitorum profundus (FDP) deep to the MN. Please click here to view a larger version of this figure.
Common ultrasound findings in median nerve entrapment
When a nerve is entrapped, such as in median nerve compression at the wrist in carpal tunnel syndrome (CTS), a typical finding is nerve enlargement as measured by the CSA, which usually occurs proximal to the site of compression at the carpal tunnel inlet around the DWC. One proposed mechanism for this is an inflammatory and/or vascular process that contributes to nerve enlargement. This is evident by the fact that corticosteroid injections peripheral to an enlarged nerve can reduce the size16. In CTS, the CSA of the median nerve at the DWC is used as a diagnostic parameter which is considered Class I evidence2. The cutoff to represent an enlarged median nerve (MN) is greater than 12 mm2, as well as a wrist to forearm ratio of greater than 1:4 (max CSA at DWC/max CSA in the middle of the forearm), both of which have been shown to be sensitive for the diagnosis of CTS3,17. Aside from cross-sectional area, an entrapped nerve may exhibit changes in nerve echogenicity, shape, fascicle size, and vascularity18. Hypoechogenicity of the median nerve is less well characterized, although often seen in CTS15. Additionally, there are reports of decreased nerve mobility in CTS with dynamic testing19. A healthy median nerve dives deep to flexor tendons with wrist and finger movement, but this movement is reduced in CTS. When the nerve moves laterally but does not dive deep, it is graded as slightly decreased mobility. When the nerve does not move in either plane, it is graded as severely reduced mobility20. There are also reports of increased nerve vascularity; as detected with Doppler ultrasound in CTS21, patients with increased nerve vascularity may experience better surgical outcomes22,23.
It must be noted that there are no standard values for these additional parameters, and the recent consensus statement recommends obtaining the median nerve cross-sectional area at a minimum2,5. The other parameters need further study but may contribute valuable clinical information. Cysts, tumors, or aberrant muscles can cause nerve entrapment; thus, it is imperative to evaluate the surroundings of the median nerve to assess for anatomical explanations for the entrapment.
Common anatomical variants to be expected include bifid median nerves (10%-15%) and persistent median arteries that runs through the carpal tunnel (5%-10%)4 (Figure 3). This 60-year-old patient has been a truck driver for the past 40 years, with chronic numbness and tingling of the first three digits on the left hand. Median nerve ultrasound shows the characteristic finding of median nerve compression at the wrist. In CTS, bifid median nerves and persistent median arteries are not more common, but they are important to identify especially when considering a perineural injection. Anatomic abnormalities contributing to CTS include traumatic neuromas, Schwannomas, lipofibromatous hamartomas, tenosynovitis, ganglion cysts, assessor muscles, hematoma, scar tissue, and other iatrogenic lesions23,24,25,26,27. These structures can be visualized with neuromuscular ultrasound and change clinical management.
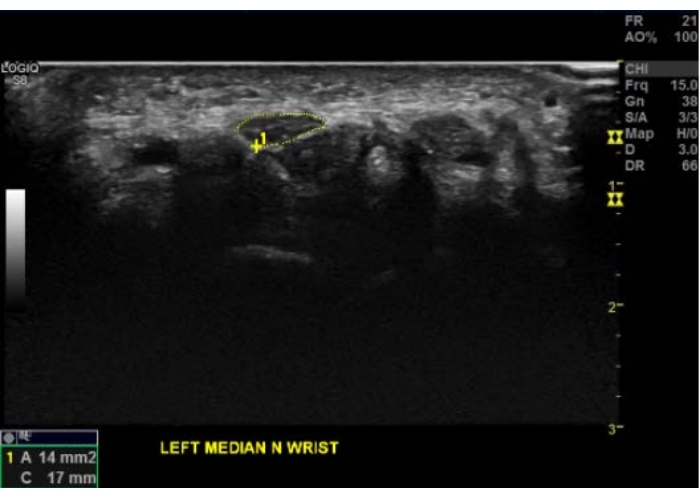
Figure 3: Common ultrasound findings in median nerve entrapment. Compression of the median nerve results in enlargement of the cross-sectional area with associated hypoechogenicity, as depicted in this cross-sectional view at the DWC. Note the typical appearance of a compressed median nerve with a flattened, hypoechoic appearance. The manual trace tool outlines the cross-sectional area in yellow of the inner epineural rim of the left median nerve. This cross-sectional area is taken at the DWC and is 14 mm2, considered a focal enlargement at the wrist consistent with carpal tunnel syndrome. Note the underlying flexor tendons beneath the median nerve. Please click here to view a larger version of this figure.
Discussion
As ultrasound visualization is a subjective process and operator dependent, it is critical to follow an organized approach in order to accurately determine parameters, including cross-sectional area, mobility, echogenicity, and vascularity. The most important steps include holding the probe perpendicular to the nerve while the patient is in the correct position. In addition, visualizing the nerve throughout its course proximally and distally to the area of entrapment allows for discovering further pathology or other structures that may contribute to the patient's symptoms. If the sonographer loses track of the nerve, moving the probe back to the DWC or to the site where the sonographer last reliably saw the nerve is beneficial. Occasionally it is necessary to increase the depth parameter on the ultrasound machine as the median nerve travels into the forearm. When done properly, ultrasound of the median nerve has been shown to assess CTS in a non-invasive manner28 reliably.
Regarding the described technique for median nerve visualization, the limitations include the absence of a standardized guideline for imaging, which can lead to variations in measurement parameters. Additionally, when evaluating the measurements of the CSA, one must consider potential comorbidities. A retrospective study from 2017 reviewing the results of over 670 patients assessed in the Duke EMG lab found that hypothyroidism patients have a marginally larger CSA compared to those without hypothyroidism (12.45 mm2 vs. 12.15 mm2, p = 0.013); they also noted there was no difference found in the patient with and without diabetes29.
The described method for median nerve visualization with ultrasound can be easily utilized in clinical practice to diagnose carpal tunnel syndrome. However, the technique is operator and machine-dependent, and measurements can be altered by age, body mass index, race, and ultrasound machine; all are limitations to this technique. Therefore, it is necessary to establish reference values by each laboratory before using neuromuscular ultrasound to diagnose CTS. It is imperative that the imaging is performed by clinicians experienced with the technique to ensure the accuracy of the measurements. The sonographer should familiarize themselves with their machine and the standardized protocol30. More studies are required to establish a reference range for nerve parameters, including palm-CSA, mobility, echogenicity, and vascularity. Future studies need to focus on morphological changes in the median nerve before and after any intervention to utilize NMUS as a prognostication tool for CTS intervention.
As demonstrated in this article, there is already clinical value in peripheral nerve ultrasound of the median nerve as an accessible, efficient, radiation-free diagnostic and prognostication tool for CTS intervention and management. Formal standardization of the technique will help broaden the utility of neuromuscular ultrasound for CTS.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We would like to thank the staff of the Wake Forest Baptist Health Neuromuscular department for their support and assistance.
Materials
| Name | Company | Catalog Number | Comments |
| GE CARES LOGIQ insite exc ultrasound Machine | any | 6066032WX0 | |
| High-frequency (12 to 18 MHz) linear array transducer | GE | ||
| Ultrasound Gel | Aquasonic |
References
- Kamel, S. R., et al. Ultrasound-guided insulin injection for carpal tunnel syndrome in type 2 diabetes mellitus patients. Clinical Rheumatology. 38 (10), 2933-2940 (2019).
- Cartwright, M. S., et al. Evidence-based guideline: neuromuscular ultrasound for the diagnosis of carpal tunnel syndrome. Muscle & Nerve. 46 (2), 287-293 (2012).
- Iyer, V. Role of ultrasonography in severe distal median nerve neuropathy. Journal of Clinical Neurophysiology. 36 (4), 312-315 (2019).
- Padua, L., et al. Contribution of ultrasound in the assessment of nerve diseases. European Journal of Neurology. 19 (1), 47-54 (2012).
- Pelosi, L., et al. Expert consensus on the combined investigation of carpal tunnel syndrome with electrodiagnostic tests and neuromuscular ultrasound. Clinical Neurophysiology. 135, 107-116 (2022).
- Kuo, T. T., et al. Assessment of median nerve mobility by ultrasound dynamic imaging for diagnosing carpal tunnel syndrome. PloS One. 11 (1), 0147051 (2016).
- Padua, L., et al. Ultrasound as a useful tool in the diagnosis and management of traumatic nerve lesions. Clinical Neurophysiology. 124 (6), 1237-1243 (2013).
- Padua, L., et al. Contribution of ultrasound in the assessment of nerve diseases. European Journal of Neurology. 19 (1), 47-54 (2012).
- Pelosi, L., Leadbetter, R., Mulroy, R. Utility of neuromuscular ultrasound in the investigation of common mononeuropathies in everyday neurophysiology practice. Muscle & Nerve. 63 (4), 467-471 (2021).
- Chompoopong, P., Preston, D. C. Neuromuscular ultrasound findings in carpal tunnel syndrome with symptoms mainly in the nondominant hand. Muscle & Nerve. 63 (5), 661-667 (2021).
- Fantino, O. Role of ultrasound in posteromedial tarsal tunnel syndrome: 81 cases. Journal of Ultrasound. 17 (2), 99-112 (2014).
- Dietz, A. R., et al. Nerve ultrasound identifies abnormalities in the posterior interosseous nerve in patients with proximal radial neuropathies. Muscle & Nerve. 53 (3), 379-383 (2016).
- Herraets, I. J. T., et al. Nerve ultrasound for diagnosing chronic inflammatory neuropathy: a multicenter validation study. Neurology. 95 (12), 1745-1753 (2020).
- Herraets, I. J. T., et al. Nerve ultrasound improves detection of treatment-responsive chronic inflammatory neuropathies. Neurology. 94 (14), 1470-1479 (2020).
- Roll, S. C., Case-Smith, J., Evans, K. D. Diagnostic accuracy of ultrasonography vs. electromyography in carpal tunnel syndrome: a systematic review of literature. Ultrasound in Medicine & Biology. 37 (10), 1539-1553 (2011).
- Cartwright, M. S., et al. Median nerve changes following steroid injection for carpal tunnel syndrome. Muscle & Nerve. 44 (1), 25-29 (2011).
- Hobson-Webb, L. D., Massey, J. M., Juel, V. C., Sanders, D. B. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clinical Neurophysiology. 119 (6), 1353-1357 (2008).
- Tai, T. -. W., Wu, C. -. Y., Su, F. -. C., Chern, T. -. C., Jou, I. -. M. Ultrasonography for diagnosing carpal tunnel syndrome: a meta-analysis of diagnostic test accuracy. Ultrasound in Medicine & Biology. 38 (7), 1121-1128 (2012).
- Nakamichi, K., Tachibana, S. Restricted motion of the median nerve in carpal tunnel syndrome. Journal of Hand Surgery. 20 (4), 460-464 (1995).
- Cartwright, M. S., Walker, F. O. Neuromuscular ultrasound in common entrapment neuropathies. Muscle & Nerve. 48 (5), 696-704 (2013).
- Mallouhi, A., Pülzl, P., Trieb, T., Piza, H., Bodner, G. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. American Journal of Roentgenology. 186 (5), 1240-1245 (2006).
- El Miedany, Y., El Gaafary, M., Youssef, S., Ahmed, I., Nasr, A. Ultrasound assessment of the median nerve: a biomarker that can help in setting a treat to target approach tailored for carpal tunnel syndrome patients. Springerplus. 4, 13 (2015).
- Hobson-Webb, L. D., Padua, L. Ultrasound of focal neuropathies. Journal of Clinical Neurophysiology. 33 (2), 94-102 (2016).
- Elsaidi, G. A., Wiesler, E. R. Lipofibromatous hamartoma of the median nerve: case presentation of MRI, ultrasound, electrodiagnostic, histologic, and surgical findings. American Journal of Orthopedics. 33 (10), 514-516 (2004).
- Therimadasamy, A., Peng, Y. P., Putti, T. C., Wilder-Smith, E. P. V. Carpal tunnel syndrome caused by gouty tophus of the flexor tendons of the fingers: sonographic features. Journal of Clinical Ultrasound. 39 (8), 463-465 (2011).
- Gonzalez, N. L., Hobson-Webb, L. D. Neuromuscular ultrasound in clinical practice: A review. Clinical Neurophysiology Practice. 4, 148-163 (2019).
- Walker, F. O., et al. Indications for neuromuscular ultrasound: Expert opinion and review of the literature. Clinical Neurophysiology. 129 (12), 2658-2679 (2018).
- Petrover, D., Bellity, J., Vigan, M., Nizard, R., Hakime, A. Ultrasound imaging of the thenar motor branch of the median nerve: a cadaveric study. European Radiology. 27 (11), 4883-4888 (2017).
- Billakota, S., Hobson-Webb, L. D. Standard median nerve ultrasound in carpal tunnel syndrome: A retrospective review of 1,021 cases. Clinical Neurophysiology Practice. 2, 188-191 (2017).
- Mota, S. J., et al. . Peripheral nerve ultrasound-anatomy and technique for diagnosis and procedures. , (2014).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved