Method Article
Combined Endoscopic and Transoral Approach for Total Maxillectomy
In This Article
Abstract
The technique of maxillectomy has been revised since it was first described in the 1820s. During the past decade, the endoscopic approach has been widely practiced for resecting maxilla. Compared with the traditional approaches, the combined endoscopic and transoral approach has many advantages such as avoiding facial incisions and postoperative scars and better visualization of the surgical margin. However, this technique is complicated to master and possess several challenges. Here, we demonstrate this approach step-by-step to show how to perform a total maxillectomy. We also reported nine cases with malignant tumors originating from the maxilla, and for all of them total maxillectomy was performed with combined endoscopic and transoral approach. Our data showed that the combination of the endoscopic and transoral approach could be used to resect the total maxilla successfully, though the tumor extended to the infratemporal and pterygopalatine fossa should be treated very carefully to avoid its spread in the local area. Furthermore, besides denture, other reconstruction methods should be attempted to improve the postoperative quality of life after the total maxillectomy.
Introduction
The squamous cell carcinoma from the maxillary sinus reports the highest incidence among the tumor developments within the sinonasal compartment1. Besides squamous cell carcinoma, the pathological patterns of maxillary tumors also include various histological types, such as adenocarcinomas, melanoma, and esthesioneuroblastoma, etc.2. Since the symptoms in the early phases are dormant and nonspecific, most of the patients diagnosed with malignant tumor originating from the maxilla are in an advanced stage during the time of diagnosis. This makes the maxillary malignant tumors one of the worst in comparison with other head and neck tumors.
The therapeutics options for the patients with malignant tumors involves maxilla surgeries combined with radiotherapies, and in some cases chemotherapies3,4,5. Many approaches of maxillectomy have been developed to resect the maxilla since it was first demonstrated in 18266. Recently, the maxillectomy can be divided into an approach with and without a skin incision. Among these approaches, lateral rhinotomy and midfacial degloving are still practiced in total maxillectomy. However, the drawbacks of these procedures include leaving a facial scar, and difficulties in treating the lesion located at or beyond the posterior margin of the maxilla due to the restricted field of visualization, limited working space, and significant bleeding of these areas7. Compared to these traditional approaches. A combined endoscopic and transoral approach has been presented for total maxillectomy without facial incision8,9. This approach, taking advantage of the better visualization of the endoscopy, might lead to the better magnification of the operative field, especially for the surgical margins, resulting in potentially similar scales of resection but with less morbidity8. In addition, no facial scars are left with this approach, which might accelerate its application for the total maxillectomy in the future. However, the technique is complicated to master and possesses several challenges. Therefore, we present a step-by-step visual protocol of a combined endoscopic and transoral approach, which may help in shortening the learning curve of this approach.
Protocol
This procedure was approved by the Institutional Review Board of the Eye and ENT Hospital, Fudan University, China. A written informed consent was obtained from all the enrolled patients.
1. Preparation for the surgery
- Before the surgery, examine the patients with anterior rhinoscopy, 4 mm endoscopy, computed tomography (CT), and Magnetic Resonance Imaging (MRI) scans to confirm the maxillary bone was invaded by the tumor and that a total maxillectomy is required. Make the surgical plan based on the location of the tumor.
- On the day of the operation, place the patient on the operating table and then give general anesthesia. Place the anesthesia intubation into the mouth on the opposite side of the tumor to facilitate to perform the following transoral approach.
- Tilt the operating table to a 30° angle (to the dorsal elevated position) and place the patient's head in a neutral position (neither flexed nor extended).
- Soak the gauze piece with iodine, then sterilize the gingivobuccal sulcus with the gauze piece.
2. Surgical procedure
- Soak 8 gauzes (6 cm x 60 cm) in a mixture of 20 mL of 1% tetracaine and 4 mL of 0.1% adrenaline. To shrink the nasal mucosa, put several pieces of soaked gauze into each nasal cavity for 5 min.
- Cut off the middle turbinate and then perform a routine ethmoidectomy and sphenoidectomy. Widen the osteum of the frontal and maxillary sinuses on the side of the lesion by the quadcut and curved sinus blades powered by the dynamic planning system.
NOTE: To reduce bleeding, the above-mentioned procedures could also be carried out with plasma. - Cut off the inferior turbinate and remove the mucosa layer on the lateral wall of the nasal cavity with the mayo scissors and the plasma.
- Drill the frontal process and the lacrimal bone with the trans-nasal skull base bur and expose the naso-lacrimal duct and lacrimal sac. Then, cut off the naso-lacrimal duct and perform the lacrimal sac incision with the blade and make sure that the mucosal flaps are laid out on the lateral nasal wall.
- Wipe off the medial wall of the maxilla with the trans-nasal skull base bur from the level of maxillary palatal process inferiorly, to the level of inferior wall of orbit superiorly, to the piriform aperture forwardly, and to the palate bone posteriorly.
- Remove the perpendicular plate of the palatine bone from the medial side to the lateral side with the trans-nasal skull base bur. Expose the palatine canal and cauterize the greater and lesser palatine arteries with the monopolar electrocoagulation.
NOTE: In this step, the conchal crest can be used as a landmark to differentiate the perpendicular plate of the palatine bone and the medial pterygoid plate. - Locate the sphenopalatine foramen, which is posterior to the ethmoidal crest. Introduce the Kerrison punch into the foramen and remove the posterior wall of the maxillary sinus anterior to the pterygopalatine fossa.
- Use a needle connected to a 5 mL syringe to immerse the gingival buccal groove in several milliliters of a mixed solution of 20 mL of 0.9% NaCl and 0.05 mL of 0.1% adrenaline in the subperiosteal planes on the side of the tumor from the level of the central incisor to the level of the third ipsilateral molar.
- Make the incision in the gingivobuccal sulcus with the blade or the monopolar electrocoagulation; start from the central incisor to the third ipsilateral molar (Figure 1A).
- Dissect of the soft tissues subperiosteally with the suction elevator, electrocoagulation, and plasma along the anterior wall of the maxillary sinus until the infraorbital rim is exposed (Figure 1B).
NOTE: The infraorbital nerve should be preserved if it was not involved by the malignancy. Whether the infraorbital nerve was involved in the tumor was identified based on the MRI and CT scan pre-surgery and confirmed during the surgery. - Separate the soft tissue from the underneath bone to the pyriform aperture level medially, to the zygomaticomaxillary fissure level laterally, and to the mandibular tubercles posteriorly.
- Retract and protect the facial soft tissue superiorly with the mastoid retractor. Wipe off the anterior wall of the maxilla with the trans-nasal skull base bur. Remove the residual bone of the piriform aperture.
- Try to keep the periostea and mucosa in the maxillary sinus intact when wiping off the anterior bony wall of the maxilla, which could reduce the bleeding. To achieve this goal, change the trans-nasal skull base bur to the carborundum drill at this step.
NOTE: After wiping off the anterior bony wall of the maxilla, the periostea and mucosa will be seen under it. The periostea and mucosa should be very obvious, if it is not involved by the tumor.
- Try to keep the periostea and mucosa in the maxillary sinus intact when wiping off the anterior bony wall of the maxilla, which could reduce the bleeding. To achieve this goal, change the trans-nasal skull base bur to the carborundum drill at this step.
- Then, remove the posterior lateral wall of the maxillary sinus by the trans-nasal skull base bur and the carborundum drill. If the infratemporal fossa was not involved by the tumor, the periostea covering it should be kept intact in this step.
- Medially, separate the connection of the vertical and the horizontal process of the palate bone by abrading the pyramidal process with the carborundum drill. Laterally, separate the maxillary tuberosity from the lateral pterygoid plate with the carborundum drill.
- Use the carborundum drill to remove to the lateral and the malar process to remove the superior and the inferior orbital walls, respectively.
- Pull out the ipsilateral central incisor. Make a hole between the soft palate and hard palate with the electricoagulation at the midline of the hard palate. Pull the fretsaw through the hole and make a sagittal incision along the hard palate from posterior to anterior (Figure 1C,D).
NOTE: In this step, the upper lip should be retracted upward and carefully protected. - Separate the hard palate from the soft palate with the Metzenbaum scissors. Then take out the maxilla from the mouth.
- Put the warm gauze (40 °C) into the operative region immediately for several minutes to stop the bleeding. Then control the bleeding by electrogoagulation.
- Rinse the surgical cavity with 40 °C warm water.
- Fix the denture to reconstruct of the hard-palatal defect. Return the facial soft tissue to the normal position.
- Cover the surface of the surgical margin with gelatin sponge. Then, pack the nasal cavity with iodoform gauze and inflation sponge.
3. Procedure and assessment after surgery
- Take out the gauze and sponge 4 days after surgery. Then, examine through enhanced CT or MRI immediately.
NOTE: Get rid of the denture before the MRI examination. - Review the patient 2 weeks after the surgery to check and clean the surgical field. Then, review the patient according to the NCCN guidelines10.
Results
In this study, we presented the details of the surgical protocol to resect the total maxillectomy with a combined endoscopic and transoral approach. We also included nine cases who were diagnosed with malignant tumors that originated from maxillary sinus and were treated in the Eye and ENT hospital of Fudan University. The combined endoscopic and transoral approach on all the patients was performed and clear surgical margins were achieved in all the patients. The patients' mean age was 47.9 years (with a range of 18-69 years). Five patients were male, and the other four were female. The stage of the tumors was assessed and recorded according to the 8th TNM edition11. In addition, the pathological diagnosis, surgical approach, the treatment strategy, and the current situation is presented in Table 1.
A representative CT scan of a patient before and after surgery is shown in Figure 2. The quality-of-life scores (QOL) of the six patients after surgery was assessed according to the University of Washington Quality of Life version 4 Questionnaire12,13. The scores of pain, appearance, activity, recreation, swallowing, chewing, speech, taste, saliva, mood, and anxiety are shown in Figure 3, and data is expressed as mean ± SE.
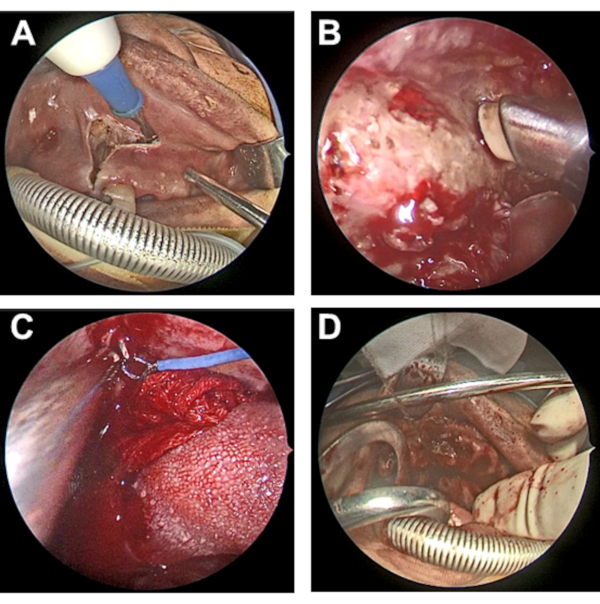
Figure 1: Intraoperative endoscopic photographs. (A) The incision was made in the gingivobuccal sulcus with the monopolar electrocoagulation. (B) Dissection of the soft tissues subperiosteally with the plasma along the anterior wall of the maxillary sinus. (C) Pull the fretsaw through the hole, which was between the soft palate and hard palate. (D) the incision was made sagittally along the hard palate from posterior to anterior. Please click here to view a larger version of this figure.
Table 1: Characteristics of patients treated with a combined endoscopic and transoral approach. The demographic and clinical characteristics are summarized. There are 5 males and 4 females ranging in age from 12 to 69 years (average, 47.9). Of these patients, 8 (89%) presented with stage T4 disease, and 1 (11%) with stage T3 disease. Lymphatic metastasis and distant metastases were detected in three and one patient(s), respectively1. Two patients died due to the recurrence of the tumor in situ2; one patient died due to the distant metastasis; M = male; F = female; CT = chemotherapy; RT = radiotherapy; NR = no recurrence; LR = local recurrence; DM = distant metastasis; NERD = no evidence of recurrent disease; DWD = died with the disease; MS = maxillary sinus; PPF = pterygopalatine fossa; PPS = parapharyngeal space; ITF = infratemporal fossa. Please click here to download this Table.

Figure 2: A presentative CT scan of a patient before and after surgery. The CT images of one presentative patient are shown. The tumor invaded the right frontal, ethmoidal, maxillary sinuses, and the maxilla before surgery (A,B). Postoperative images showed that the tumor has been totally resected and the denture used to reconstruct the hard palate was in position (C,D). Please click here to view a larger version of this figure.

Figure 3: The quality of life of patients after total maxillectomy. (A) The University of Washington-QOL (UW-QOL) scores were utilized to assess the QOL after surgery. The domains were scored on a scale ranging from 0 (worst) to 100 (best), focusing on the past 7 days. (Pain: 91.7 ± 12.9; Appearance: 70.8 ± 18.8; Activity: 62.5 ± 13.7; Recreation: 54.2 ± 10.2; Swallowing: 68.3 ± 22.3; Chewing: 8.3 ± 20.4; Speech: 30.0 ± 0.0; Taste: 58.3 ± 28.6; Saliva: 63.3 ± 16.3; Mood: 66.7 ± 20.4; Anxiety: 75.0 ± 12.2). (B) In addition, we asked the patients to choose three of these domains that were the most important to them. Three patients rated appearance as the most important domain, four reported swallowing was important to them, five cared about chewing, while everyone reported speech was the single most important factor to them. Please click here to view a larger version of this figure.
Discussion
In this work, we demonstrated an endoscopic approach to resect the total maxilla. Our results showed that this approach was effective and safe to achieve its goal, which is consistent with previous cadaveric8 and clinical studies9. Nine patients with malignant tumor originated from maxillary sinus were treated with this endoscopic approach. All of their information was recorded, and the length of their follow-up ranged from 2 months to 32 months. During the follow-up period, six of them were alive without recurrence, two of them had local recurrence and died in the fourth and ninth months after surgery, respectively, and one of them died due to progressive cachexia without local recurrence.
In this study, all of the patients were diagnosed at an advanced stage, and the lesions in seven patients had extended to the infratemporal fossa, pterygopalatine fossa, or even the cavernous sinus. Besides total maxillectomy, most of the lesions beyond the maxilla were also resected with endoscopy successfully. However, there were still two patients with local recurrence after surgery, one was recurrent at the foramen rotundum, another was at the soft tissue in the infratemporal fossa, and these recurrent sites are consistent with the report of Deganello et al.14. This reminded us of the fact that the lesions located in these areas should be treated more radically.
Health-related quality of life has been increasingly applied as an important outcome parameter of surgery, it refers to the patients' physical, emotional, and social health15. The maxilla is located in the center of the face, and it plays an important role in bearing the maxillary teeth, transmitting masticatory forces, giving support to the orbit, and attaching the muscles of facial expression16, so the resection of the maxilla will lead to the patient's esthetics and functional disfigurement. To review the impact of the total maxillectomy by the combined endoscopic and transoral approach and our reconstruction method on the patients' QOL, the UW-QOL version 4 questionnaire, which is a comprehensive questionnaire and had been used in head and neck cancer patients, was investigated retrospectively in our study. Three patients died during the follow-up, therefore, the questionnaires were responded by six patients. As shown in Figure 3A,B, the procedure of the surgery and the construction method had a significant impact on the patients' chewing and speaking functions while the patients reported that these two domains were the most important domains to them. In our opinion, this might be because most of the patients had lesions in the infratemporal fossa; to resect these lesions, we have to sacrifice the medial pterygoid muscle and lateral pterygoid muscle sometimes, which will influence the chewing and speaking inevitably. In addition, we only used denture to reconstruct the defects in our cases, that would leave a huge cavity and would impact the speech function of the patients. One of the disadvantages of the combined endoscopic and transoral approach is it limited the transplantation of the pedicle flap in the surgical area. Recently, some other reconstruction procedures such as free flaps and three-dimensional printing techniques appear to be helpful to reach the vital functional and aesthetic reconstruction consequences17,18,19,20. What needs to be pointed out is that, in this work, the QOL was investigated after the denture was used to reconstruct the defects. Thus, we couldn't evaluate the influence of the surgery itself on the patients' QOL and compare it with other total maxillectomy procedures.
There are some tips in the combined endoscopic and transoral approach based on our experience. First, the plasma is extremely useful in this approach. The cutting and hemostasis function of the plasma make it possible to resect and stop the bleeding in the meantime, which will not only reduce the bleeding but also make the anatomical sign easier to be confirmed. Second, the bone and the periosteum should be resected separately, especially for the posterior lateral wall of the maxillary sinus. If the periosteum is not invaded by the tumor, it should be saved to avoid the injury of the contents of the pterygopalatine fossa and infratemporal fossa. To achieve this, the fine emery diamond should be used instead of the rough diamond when the resection is close to the periosteum. Third, before packing, we apply 40 °C warm water to douche the surgical field to check whether there are any potential bleeding points.
To sum up, the combined endoscopic and transoral approach can be applied for total maxillectomy, which can be further extended to resect the tumor in the pterygopalatine fossa and infratemporal fossa using higher visualization potential of endoscopy. However, the facial incision should be performed if the tumor has invaded the facial skin, which is the contraindication of the combined approach. Furthermore, other reconstruction techniques besides denture should also be tried to improve the patients' QOL after surgery.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was sponsored by the Shanghai Municipal Commission of health and Family Planning (201740187), Shanghai Science and Technology Committee Foundation (19411950600 and 19441900300), Research Units of New Technologies of Endoscopic Surgery in Skull Base Tumor (2018RU003, Chinese Academy of Medical Sciences), New Technologies of Endoscopic Surgery in Skull Base Tumor: CAMS Innovation Fund for Medical Sciences (CIFMS) (2019-I2M-5-003), National Nature Science Foundation of China for Young Scholars (81300810), Natural Science Foundation of Shanghai (20ZR1410000), National Natural Science Foundation of China (81970856).
Materials
| Name | Company | Catalog Number | Comments |
| Carborundum drill | Medtronic, Inc. | REF15BA60D | |
| Curved sinus blade | Medtronic, Inc. | REF1884006 | 11 cm x 4 mm |
| Dynamic planing system | Medtronic, Inc. | REF1898001 | |
| Electrocoagulation | Shanghai Hutong Electronics. Co.,Ltd | GD350-B5 | |
| Epinephrine | Shanghai Harvest Pharmaceutical Co., Ltd | 10170405 | |
| Fret Saw Wire Instruments | Shanghai Medical Instruments (Group) Ltd., Corp. Surgical Instruments Factory | N30030 | |
| Gauze | Ningbo Shenyuan Medical Material Co., Ltd | 6 cm x 60 cm | |
| Mastoid Retractor | Shanghai Medical Instruments (Group) Ltd., Corp. Surgical Instruments Factory | NH6F090 | Lengh: 16 cm |
| Mayo scissors | Shanghai Medical Instruments (Group) Ltd., Corp. Surgical Instruments Factory | J22040 | Lengh: 16 cm |
| Metzenbaum scissors | Shanghai Medical Instruments (Group) Ltd., Corp. Surgical Instruments Factory | JC2514 | Lengh: 25 cm |
| Nasal Endoscopy | Karl Storz-Endoskope | 7230 AA | |
| Plasma (EVAC 70 Xtra HP With integrated Cable) | Smith & Nephew | EIC5874-01 | |
| Quadcut blade | Medtronic, Inc. | REF1884380HR | 4.3 mm |
| Suction Elevator | Zhejiang Tian Song Medical Products Co., Ltd | B2117.1 | Width: 4 mm |
| Tetracaine | Eye & ENT Hospital of Fudan University | 180130 | |
| Trans-Nasal Skull Base Bur | Medtronic, Inc. | REFTN45RCD | 13 cm x 4.5 mm |
References
- Santos, M. R., et al. Squamous cell carcinoma at maxillary sinus: clinicopathologic data in a single Brazilian institution with review of literature. International Journal of Clinical and Experimental Pathology. 7 (12), 8823-8832 (2014).
- Turner, J. H., Reh, D. D. Incidence and survival in patients with sinonasal cancer: a historical analysis of population-based data. Head & Neck. 34 (6), 877-885 (2012).
- Choi, E. C., et al. Surgical outcome of radical maxillectomy in advanced maxillary sinus cancers. Yonsei Medical Journal. 45 (4), 621-628 (2004).
- Hanna, E. Y., et al. Induction chemotherapy for advanced squamous cell carcinoma of the paranasal sinuses. Archives of Otolaryngology-Head and Neck Surgery. 137 (1), 78-81 (2011).
- Kovacs, A. F., Eberlein, K., Hulsmann, T. Organ preservation treatment using TPF-a pilot study in patients with advanced primary and recurrent cancer of the oral cavity and the maxillary sinus. Oral and Maxillofacial Surgery. 13 (2), 87-93 (2009).
- Sisson, G. A., Toriumi, D. M., Atiyah, R. A. Paranasal sinus malignancy: a comprehensive update. The Laryngoscope. 99 (2), 143-150 (1989).
- Kreeft, A. M., et al. Preoperative imaging and surgical margins in maxillectomy patients. Head & Neck. 34 (11), 1652-1656 (2012).
- Rivera-Serrano, C. M., Terre-Falcon, R., Duvvuri, U. Combined approach for extensive maxillectomy: technique and cadaveric dissection. American Journal of Otolaryngology. 32 (5), 417-421 (2011).
- Liu, Z., et al. Combined transoral and endoscopic approach for total maxillectomy: a pioneering report. Journal of Neurological Surgery. Part B, Skull Base. 74 (3), 160-165 (2013).
- Pfister, D. G., et al. Head and neck cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network. 18 (7), 873-898 (2020).
- Brierley, J. D., et al. . TNM classification of malignant tumours. 8th Edition. , (2017).
- Akinmoladun, V. I., Akinyamoju, C. A., Olaniran, F. O., Olaopa, O. I. Maxillectomy and quality of life: experience from a nigerian tertiary institution. Nigerian Journal of Surgery. 24 (2), 125-130 (2018).
- Rogers, S. N., et al. The addition of mood and anxiety domains to the University of Washington quality of life scale. Head & Neck. 24 (6), 521-529 (2002).
- Deganello, A., et al. Endoscopic-assisted maxillectomy: Operative technique and control of surgical margins. Oral Oncology. 93, 29-38 (2019).
- Weinberger, M., Oddone, E. Z., Samsa, G. P., Landsman, P. B. Are health-related quality-of-life measures affected by the mode of administration. Journal of Clinical Epidemiology. 49 (2), 135-140 (1996).
- Baliarsing, A. S., Kumar, V. V., Malik, N. A., B, D. K. Reconstruction of maxillectomy defects using deep circumflex iliac artery-based composite free flap. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 109 (3), 8-13 (2010).
- Moya-Plana, A., et al. Reconstruction of maxillectomy and midfacial defects using latissimus dorsi-scapular free flaps in a comprehensive cancer center. Oral Oncology. 99, 104468 (2019).
- Jang, W. H., et al. Mirror image based three-dimensional virtual surgical planning and three-dimensional printing guide system for the reconstruction of wide maxilla defect using the deep circumflex iliac artery free flap. The Journal of Craniofacial Surgery. 30 (6), 1829-1832 (2019).
- Kim, S. E., Shim, K. M., Jang, K., Shim, J. H., Kang, S. S. Three-dimensional printing-based reconstruction of a maxillary bone defect in a dog following tumor temoval. In Vivo. 32 (1), 63-70 (2018).
- Largo, R. D., Garvey, P. B. Updates in head and neck reconstruction. Plastic and Reconstructive Surgery. 141 (2), 271-285 (2018).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved