Cardiac Exam III: Abnormal Heart Sounds
Przegląd
Source: Suneel Dhand, MD, Attending Physician, Internal Medicine, Beth Israel Deaconess Medical Center
Having a fundamental understanding of normal heart sounds is the first step toward distinguishing the normal from the abnormal. Murmurs are sounds that represent turbulent and abnormal blood flow across a heart valve. They are caused either by stenosis (valve area too narrow) or regurgitation (backflow of blood across the valve) and are commonly heard as a "swishing" sound during auscultation. Murmurs are graded from 1 to 6 in intensity (1 being the softest and 6 the loudest) (Figure 1). The most common cardiac murmurs heard are left-sided murmurs of the aortic and mitral valves. Right-sided murmurs of the pulmonary and tricuspid valves are less common. Murmurs are typically heard loudest at the anatomical area that corresponds with the valvular pathology. Frequently, they also radiate to other areas.
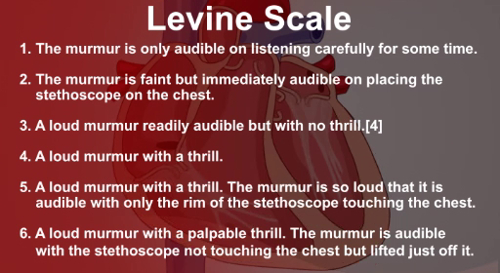
Figure 1. The Levine scale used to grade murmur intensity.
In addition to the two main heart sounds, S1 and S2, which are normally produced by the closing of heart valves, there are two other abnormal heart sounds, known as S3 and S4. These are also known as gallops, because of the "galloping" nature of more than two sounds in a row. S3 is a low-pitched sound heard in early diastole, caused by blood entering the ventricle. S3 is a sign of advanced heart failure, although it can be normal in some younger patients. S4 is heard in late diastole and represents ventricular filling due to atrial contraction in the presence of a stiff ventricle. S4 is also heard in heart failure and left ventricular hypertrophy.
Procedura
1. Murmurs
- Position the patient at a 30- to 45-degree angle on the examination table.
- When auscultating a murmur, ask the patient to breathe in and out, as it can provide a vital diagnostic clue. Right-sided murmurs (pulmonary and tricuspid) are best heard on inspiration, as blood flows into the right ventricle when intrathoracic pressure decreases. Conversely, left-sided murmurs are heard best on expiration.
- Categorize murmurs according to the following criteria: intensity (loudness), pitch (e.g., high or low, harsh or blowing), configuration (e.g., crescendo-decrescendo), location, and timing in the cardiac cycle (e.g., early systolic/diastolic).
- Remember that not all murmurs are abnormal, and that systolic murmurs can be benign in younger people.
- Also remember that each murmur is usually loudest at the anatomical area that corresponds with the valvular pathology.
- Aortic stenosis: Auscultate with the diaphragm of the stethoscope on the aortic area, with the patient in supine position. Aortic stenosis is a harsh-sounding ejection systolic or crescendo-decrescendo murmur that occurs during systole, as the blood passes across the stenotic aortic valve. This murmur classically radiates to the carotid arteries and can be heard in the carotid area of the neck.
- Aortic regurgitation: Auscultate with the diaphragm of the stethoscope at the lower left sternal border, close to the tricuspid area, with the patient leaning forward. The murmur of aortic regurgitation is a soft-blowing early diastolic decrescendo murmur. It can be associated with a number of other physical examination findings (described in step 5 below).
- Mitral regurgitation: Place the diaphragm of the stethoscope on the mitral area. This murmur is a blowing pansystolic (or holosystolic) murmur. It classically radiates toward the axilla. Mitral valve prolapse can also be associated with a "mid-systolic click" sound.
- Mitral stenosis: Auscultate with the bell of the stethoscope in the mitral area. It is a low-frequency rumbling mid-diastolic murmur and can be accentuated by laying the patient on his/her left side. Mitral stenosis is a very rare murmur that is almost always the result of prior rheumatic fever.
- Right-sided murmurs: Remember that murmurs associated with the tricuspid and pulmonary valves are rare. Pulmonary stenosis, tricuspid regurgitation, and hypertrophic cardiomyopathy manifest as systolic murmurs. Tricuspid regurgitation occurs in association with longstanding lung disease, such as emphysema or pulmonary hypertension. Pulmonary regurgitation and tricuspid stenosis are diastolic murmurs. Congenital heart disorders, such as patent ductus arteriosus (PDA), can also cause loud murmurs. In the case of PDA, a continuous "machinery-like" murmur is auscultated.
2. Gallops (S3 and S4)
- Auscultate for S3 and S4 in the mitral and tricuspid areas with the bell of the stethoscope pressed lightly on the patient's chest, and the patient lying on his/her left side.
3. Splitting of heart sounds:
The second heart sound can be "split" when the closure of the aortic and pulmonary valves do not occur together. The splitting of S2 during inspiration is normal and is known as physiological splitting (P2 occurs after A2). Fixed splitting can be heard with an atrial septal defect. If the splitting occurs during expiration, it is known as paradoxical splitting, which occurs when there is a prolonged left ventricular phase, such as in left bundle branch block or hypertrophic cardiomyopathy.
- Ask the patient to breathe in and out, and auscultate over the second intercostal space at the left sternal edge.
- Note at which phase of respiratory cycle the splitting occurs.
4. Rubs:
A pericardial friction rub, as seen in pericarditis, resembles a rubbing sound of two surfaces rubbing or grating against each other.
- Auscultate at the lower left sternal edge with the patient leaning forward.
5. Note if the following signs of valvular pathology are present:
- Quincke's pulse: seen in aortic regurgitation, resulting in alternating blanching and flushing of the nail bed.
- Corrigan's pulse, also known as Watson's water hammer pulse: a collapsing pulse that occurs in aortic regurgitation.
- de Musset's sign: a "bobbing" movement of the head, as seen with aortic regurgitation.
- Blood pressure: a small gap between the systolic and diastolic blood pressure (narrow pulse pressure), frequently found in aortic stenosis. A wide pulse pressure is characteristic of aortic regurgitation.
Wniosek i Podsumowanie
The ability to recognize and distinguish between the different cardiac murmurs develops with time and practice. The first step is to identify normal from abnormal. When a murmur is heard, an examiner should think about the following questions: What part of the cardiac cycle does it occur in - systolic or diastolic? Where is the murmur loudest? Where does the murmur radiate to? Is it loudest on inspiration or expiration?
An examiner should make sure the environment is quiet and that there is ample time to hear the murmur. Loud murmurs are often heard across the precordium, in which case, ascertaining where it is loudest and where it radiates to is crucial. Whenever a murmur is heard, the clinician should get into the habit of going through this systematic approach in order to correctly diagnose the underlying pathology.
Przejdź do...
Filmy z tej kolekcji:

Now Playing
Cardiac Exam III: Abnormal Heart Sounds
Physical Examinations I
91.1K Wyświetleń

General Approach to the Physical Exam
Physical Examinations I
115.3K Wyświetleń

Observation and Inspection
Physical Examinations I
92.9K Wyświetleń

Palpation
Physical Examinations I
82.5K Wyświetleń

Percussion
Physical Examinations I
99.3K Wyświetleń

Auscultation
Physical Examinations I
60.1K Wyświetleń

Proper Adjustment of Patient Attire during the Physical Exam
Physical Examinations I
82.9K Wyświetleń

Blood Pressure Measurement
Physical Examinations I
106.9K Wyświetleń

Measuring Vital Signs
Physical Examinations I
113.6K Wyświetleń

Respiratory Exam I: Inspection and Palpation
Physical Examinations I
155.7K Wyświetleń

Respiratory Exam II: Percussion and Auscultation
Physical Examinations I
211.3K Wyświetleń

Cardiac Exam I: Inspection and Palpation
Physical Examinations I
175.2K Wyświetleń

Cardiac Exam II: Auscultation
Physical Examinations I
139.0K Wyświetleń

Peripheral Vascular Exam
Physical Examinations I
67.7K Wyświetleń

Peripheral Vascular Exam Using a Continuous Wave Doppler
Physical Examinations I
38.4K Wyświetleń
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone