Method Article
Echocardiographic Evaluation of Atrial Communications before Transcatheter Closure
* Wspomniani autorzy wnieśli do projektu równy wkład.
W tym Artykule
Podsumowanie
Transthoracic (TTE) and transesophageal (TEE) echocardiography represent the basic imaging tools for interatrial septum examination. Three dimensional (3D) TEE provides incremental information in the assessment of the interatrial septum. Further advanced echocardiography techniques using speckle tracking echocardiography are applied for sensitive volumetric and functional assessment of the heart chambers.
Streszczenie
Transthoracic (TTE) and transesophageal echocardiography (TEE) is the standard imaging method for atrial septal defect (ASD) and patent foramen ovale (PFO) detection, for patient selection for transcatheter ASD/PFO closure, for intraoperative guidance and for long-term follow-up. The size, shape, location and the number of the atrial communications schould be determined. The accuracy of PFO detection can be improved by using agitated saline together with maneuvers to transiently increase the right atrial (RA) pressure. The appearance of microbubbles in the left atrium (LA) within 3 cardiac cycles after opacification of the RA is considered positive for the presence of an intracardiac shunt. Three dimensional TEE identifies further septal fenestrations and describes the dynamic morphology of ASD/PFO and atrial septal aneurysm. Follow-up evaluations with TTE is recommended at 1, 6, and 12 months after the procedure, with a subsequent evaluation every year. Previous studies showed an increased incidence of atrial arrhythmias early after device closure. Speckle tracking analysis may help to understand functional left atrial remodeling following percutaneous closure and its impact on atrial arrhythmias.
Wprowadzenie
Patent Foramen Ovale (PFO) is not a true tissue deficiency of atrial septum; it is present in about 20-25% of the adult population, and in most cases it does not have any clinical significance (Figure 1). Cryptogenic stroke accounts for ~30% of ischemic strokes and is defined as a condition without an apparent cause at the early inpatient work-up. Patients under 45 years of age represent 10% of stroke burden with as much as 40% defined as cryptogenic. Secondary prevention of stroke using transcatheter closure technique remains paramount in reducing morbidity and mortality1.
Atrial septal defects (ASDs) include different lesions on different atrial septum locations, resulting in shunting. The most common form is ostium secundum ASD, usually optimal for percutan devise closure. ASDs are generally discovered during the workup of right ventricular (RV) dysfunction and/or dilatation, and rarely after a suspected paradoxical embolism or cryptogenic stroke2,3.
Transthoracic (TTE) and transesophageal (TEE) echocardiography is performed for qualitative and quantitative assessment of atrial septum deficiencies. Three dimensional (3D) TEE provides more in depth information of the interatrial septum, and it gives more precise imaging of catheters and the closure device during intraoperative guiding. Postoperative follow up evaluations with TTE should be performed at 1, 6, and 12 months after the procedure, with a subsequent evaluation every year to assess device position, residual shunts, pericardial effusion, changes in size and function of the cardiac chambers and pulmonary circulation. Further advanced echocardiography techniques using speckle tracking echocardiography may help to understand potential functional left atrial remodeling following percutaneous closure and its impact on atrial arrhythmias2.
Protokół
In the following part we describe the protocol steps of clinical and imaging evaluation of atrial communications before transcatheter closure based on international clinical guidelines. These protocols follow the guidelines of the Semmelweis University Regional and Institutional Committee of Science and Research Ethics. Informed written patient consent is needed.
1. Clinical evaluation and workflow of cryptogen stroke and PFO for transcatheter closure
- For the diagnostic work-up of stroke, determine whether the stroke is ischemic or hemorrhagic in origin using computed tomography scan (CT) or magnetic resonance brain imaging (MRI).
- In case of ischemic etiology, perform subsequent CT- or MR-angiography of the head and neck to exclude any intracranial- and cerebral- or extracerebral vascular pathology, which would warrant specific therapy.
- Perform blood work to test for a hypercoagulable state, most importantly an antiphospholipid syndrome or other genetic alterations leading to a coagulation disorder. A patient with hypercoagulability is not a good candidate for closure, as thrombus formation could occur on the surface or near the implanted device in these cases4,5.
- Use inpatient ECG monitoring to rule out atrial fibrillation.
NOTE: Further extended outpatient rhythm monitoring with an ambulatory 24-36-hour Holter, with an external event recorder or even with an insertable monitoring device, should be considered to detect the occurrence of atrial fibrillation, which is silent in a considerable proportion of stroke patients. - Perform a TTE scan to exclude cardioembolic sources other than atrial fibrillation, such as non-compaction cardiomyopathy, dilated cardiomyopathy with severely depressed left ventricular ejection fraction, any intracardiac mass, vegetation or intracavitary thrombus and to assess the morphology of the interatrial septum for the presence of septal aneurysm.
NOTE: The latter can raise the suspicion for the presence of PFO. - For the final work-up step in patient selection for PFO closure, make a multidisciplinary team decision involving the neurologist, the cardiologist and the cerebral imaging specialist.
2. Clinical evaluation and workflow of ASD for transcatheter closure
- Perform preprocedural cardiac MR (CMR) and right heart catheterisation (RHC) to diagnose complex congenital heart disease, where an ASD is only one element of a complex case. In these cases, closure of the ASD is usually part of a complex surgical repair procedure, rather than a transcatheter one.
NOTE: Simple, secundum type ASDs with a volume-overloaded RV due to a pulmonary/systemic flow (Qp/Qs) ratio of >1.5 and not elevated RV pressure are suitable for a single-step transcatheter closure if surrounded by a minimum rim of 5 mm6. Multi-fenestrated defects are often amenable for closure with multiple devices. - Measure pulmonary vascular resistance (PVR) at baseline by RHC when shunting is excessive and there is elevated RV systolic pressure.
- In case of moderately elevated PVR (4-8 Wood units), perform a staged transcatheter closure by implanting a fenestrated closure device first to reduce the amount of initial shunting. Perform full closure after improvement of RV function and a decrease in PVR a couple of months later in a second step. Markedly elevated baseline PVR values above 8 Wood units usually form a contraindication for closure, as this would deteriorate RV function even further.
3. 2D transthoracic echocardiography imaging for the interatrial septum
NOTE: The assessment of interatrial septum is recommended according to the 2015 ASE guidelines2. The patient is lying in the left decubitus position with the left arm placed under the head. Standard parasternal, apical and subcostal views are obtained.
- Use the subxiphoid frontal four-chamber view; it provides good axial resolution to measure the diameter of the defect along its long axis.
- Use the subxiphoid sagittal view to visualize the atrial septum along its superior–inferior axis.
- Use the apical four-chamber view to estimate haemodinamic consequencies of interatrial left to right shunting including RA, RV dilation and RV pressure.
- Use the parasternal short-axis view to measure the aortic and posterior rim of the septal defect.
4. 2D/3D Transthoracic Echocardiography Imaging for the anatomical and functional quantification of heart chambers
NOTE: Assessment of atria is recommended according to the consensus statement from the ASE and EACVI on chamber quantification7.
- Perform conventional volumetric and functional LA measurement.
- Perform advanced echocardiography techniques using speckle tracking. Optimize acquisition frame rates for speckle tracking to provide the highest frame rate per cardiac cycle without significantly decreasing spatial resolution.
- In the 2D LA strain curve, set the zero strain reference at the left ventricular end-diastole. Calculate the LA strain values of each phase as the difference of two of these measurements8. LA function is divided into reservoir, conduit and contraction phase. All considerations made for LA measurements can be applied for RA assessment as well.
- Measure the tricuspid annular plane systolic excursion, the RV fractional area change, the Doppler tissue imaging (DTI) S’ velocity, and the RV ejection fraction from 3D volumetric evaluation. Perform 2D speckle tracking analysis with RV strain parameters for the evaluation of RV systolic function9.
NOTE: RV measurements are highly important in case of hemodynamically significant ASD, when RV function can be impaired and significant pulmonary hypertension can occur. - Obtain electrocardiographically gated full-volume 3D data sets from apical four chamber view for 3D LA, LV and RV volume and function measurement, representing parameters of incremental prognostic value over 2D LA parameters10,11.
- Perform conventional volumetric and functional LV measurements, including LV diastolic function assessment using mitral inflow and annular tissue Doppler imaging.
NOTE: In case of diastolic dysfunction, acute heart failure may develope after ASD closure due to LV volume overload. - Assess LV global longitudinal strain due to its prognostic value.
NOTE: However, circumferential and radial strain can be also assessed12,13.
5. Transesophageal echocardiography imaging for the interatrial septum
- Perform TEE examination in patients clinically suitable for potential percutaneous device closure to assess technical feasibility of the closure as well. Otherwise, perform TTE examination or transcranial doppler (TCD) using agitated saline to prove the presence of an interatrial shunt2,14,15,16. Informed written patient consent is mandatory before TEE examination.
- Position the patient on the left lateralis decubitus in case of preoperative screening TEE and on the back position in case of intraoperative TEE. Ensure that patients fast for at least 4 h and remove dental fixtures.
- Use topical oropharyngeal anesthesia (such as lidocaine) and intravenous sedatives (such as midazolam, typical dose 1-5mg) before screening TEE. The intraoperative guiding TEE is performed usually under general anaesthesia.
- Monitor ECG, blood pressure and oxygen saturation. Furthermore, availability and experience with resuscitation equipment is mandatory.
- Define the number, size and location of defects as well as the surrounding atrial septal tissue (rims) and the presence of atrial septal aneurysm. Determine the hemodynamic consequences of atrial septal defects using conventional 2D TEE views, of which midesophageal bicaval and aortic valve short axis view are the most important (Figure 2).
- Verify communication through the foramen using agitated saline contrast during the Valsalva maneuver, when the right atrial pressure temporarily increases, the overlapping septum primum and secundum opens, and the bubbles can cross the canal of PFO from the right atria to the left atria within 3 cardiac cycles.
NOTE: The amount of crossing bubbles depends on the size of PFO. A large (grade III) shunt is defined when the number of bubbles exceeds 20. - Use 3D TEE acquisition methods mainly from the midesophageal short axis view or the bicaval view. Use the narrow-angled (zoomed) and wide-angled (full volume) mode to obtain additional information on the complex and dynamic anatomy of interatrial septum. Measure the size of atrial septal defect at the atrial end-diastole and end-systole in en face views from either the RA or LA (Figure 3).
- Use intraoperative transesophageal echocardiography to guide all steps of the procedure mainly from midesophageal bicaval and short axis view, including advancing the guidewire through the PFO tunnel or ASD and closure device delivery (Figure 1, Figure 4, Figure 5).
- Perform balloon sizing of the stretched diameter of ASD using fluoroscopy and TEE as well.
NOTE: The maximum size of the closure device is 90% of the atrial septal length; nevertheless, the ratio of the device to defect should not exceed 2:1 (Figure 6). - Before the delivery system detachment, evaluate the presence of the residual shunt evaluation and measure the atrial septal tissue rim and atrial roof to closure device distance using a four chamber, short axis and bicaval TEE view.
6. Postoperative follow-up
- Perform the TTE study before hospital discharge and repeat within 1 month to assess device position, residual shunt and pericardial effusion due to device errosion.
- Perform TTE examination and 12-lead electrocardiography follow up studies at 6, and 12 months, with a subsequent evaluation every year.
- Measure conventional Doppler parameters to evaluate the effect of transcatheter ASD closure on left-sided chambers.
- Measure atrial and ventricular volumetric changes and longitudinal strain parameters are measured in order to track cardiac remodelling (Figure 7, Figure 8). Atrial arrhythmias occur mainly within 1 month after device deployment17.
Wyniki
Clinical evaluation of symptomatic, 41 years old female patient revealed ostium secundum type ASD and floppy atrial septum using TTE and TEE examination
TTE examination showed right ventricular and biatrial enlargement with elevated pulmonary artery systolic pressure. TEE examination was used to estimate the size and shape of ASD using 2D and 3D methods. 2D, 3D native and balloon sizing TEE measurements were compared (Figure 4, Figure 5, Figure 6). In the case of floppy atrial septum, intraoperative balloon sizing is really important, as the fully stretched ASD size in such cases are underestimated even with 3D measurements. According to balloon sizing measurements (23-24 mm of ASD stretched diameter), a 29 mm of diameter ASD closure device was chosen. Following deployment, the presence of interatrial tissue in between the discs, residual shunts and pericardial effusion are evaluated.
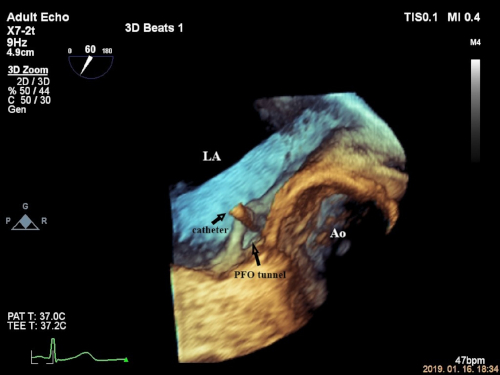
Figure 1. Intraoperative 3D zoom image of catheter while crossing the PFO tunnel. The catheter can elevate the interatrial septum while crossing the PFO tunnel. The 3D zoom image was performed from 60° midesophageal aortic valve short-axis view. LA: left atrium; RA: right atrium; Ao: aorta. Please click here to view a larger version of this figure.
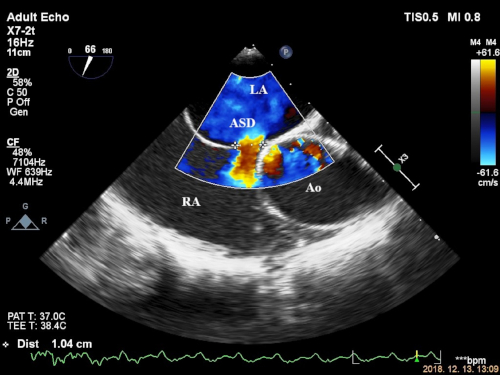
Figure 2. Measurement of ostium secundum ASD using 2D TEE color flow from mid-esophageal short axis view. The 2D TEE image shows 2D color flow technique to measure one dimensional ostium secundum ASD size at the largest size. The 2D TEE image was performed from 60 degree midesophageal aortic valve short-axis view. LA: left atrium; RA: right atrium; Ao: aorta; ASD: atrial septal defect. Please click here to view a larger version of this figure.

Figure 3. Measurement of ostium secundum ASD using 3D zoom” en face” view (same patient of Figure 2). The image demonstrates the importance of 3D aquisition technique when measuring ASD size as the shape of the ASD usually is ovale. The measurement was performed on the same patient of Figure 2. ASD: atrial septal defect. Please click here to view a larger version of this figure.
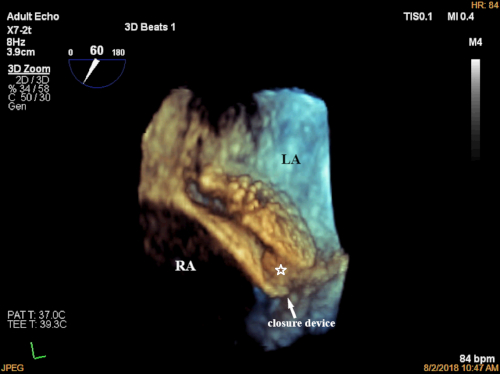
Figure 4. Intraoperative 3D zoom acquisition of PFO closure device approaching the interatrial septum from the left side. The image showes the opening of the left-sided disc of the PFO closure device in the left atrium and its approaching to the interatraial septum. The 3D zoom image was performed from 60 degree midesophageal aortic valve short-axis view. LA: left atrium. Please click here to view a larger version of this figure.

Figure 5. Intraoperative 3D zoom image of fully deployed PFO closure device. 3D image of fully deployed PFO closure device demonstrating the interatrial septum between the the left- and right-sided discs (white asteroid). The 3D zoom image was performed from 60 degree midesophageal aortic valve short-axis view. LA: left atrium; RA: right atrium. Please click here to view a larger version of this figure.

Figure 6. Intraoperative 2D TEE balloon sizing of ASD (same patient of Figure 2 and 3). The image demonstrates the importance of intraoperative balloon sizing In the case of floppy atrial septum as the fully stretched ASD size in such cases are underestimated even with 3D measurements. The measurement was performed on the same patient of Figure 2 and 3. LA: left atrium; RA: right atrium. Please click here to view a larger version of this figure.
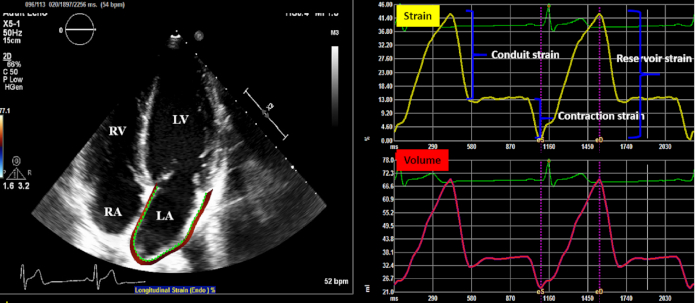
Figure 7. Off-line 2D speckle tracking analysis of left atrium in order to measure volumetric and functional parameters (reservoir, conduit and contraction strain). 2D TTE apical four chamber view was obtained to analyse left atrium. The semi-automated software delineates the endocardial border of the left atrium than volumetric and functional measurements are calculated during the cardiac cycle (left upper and lower panel). The contraction strain can be measured only in sinus rhythm. LA: left atrium; RA: right atrium. Please click here to view a larger version of this figure.
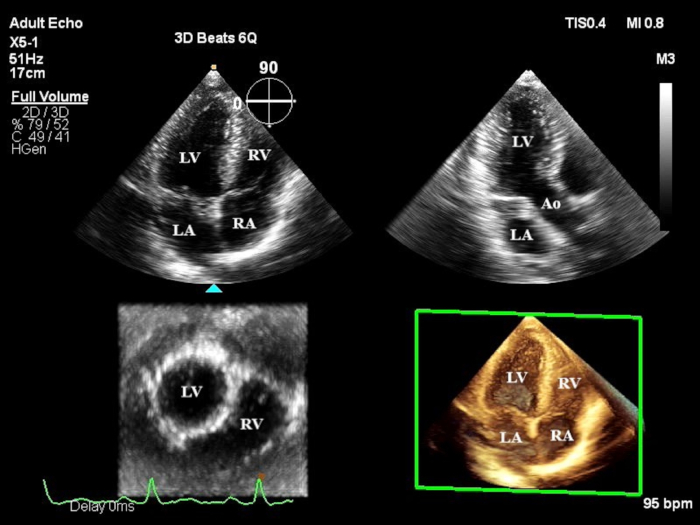
Figure 8. 3D TTE full volume acquisition from apical four chamber view for 3D volumetric and functional analysis. 3D TTE apical four chamber full volume aquisition view was obtained to analyse left atrium 3D volumes and function. LA: left atrium; RA: right atrium; LV: left ventricle; RV: right ventricle. Please click here to view a larger version of this figure.
Dyskusje
Careful patient selection for transcatheter PFO closure represents one of the most challanging steps of the clinical evaluation, as ruling out atrial fibrillation can be difficult. Several trials in the past few years have suggested greater yield with longer term monitoring to detect atrial fibrillation.18 The Cryptogenic Stroke and Underlying Atrial Fibrillation (CRYSTAL-AF) trial detected increased atrial fibrillation rate in the insertable cardiac monitor group (8,9%) compared with standard monitoring techniques (1.4%) by 6 months and this rate climbed up to 12.4% vs 2.0 % by 12 months in cryptogenic stroke patients19. Accordingly, older patients with cryptogenic stroke and comorbidities should be considered for longer term monitoring, such as 30-day monitoring, before scheduling for transcatheter PFO closure. In patients with comorbidities sometimes it is hard to judge the role of the PFO as a cause of cryptogenic stroke or just as a bystander. The externally validated Risk of Paradoxical Embolism clinical score model (RoPE score) can add further certainty, as an 8 or higher value points towards a causative role of PFO in cryptogenic stroke20. Based on RESPECT trial, there is 54% relative risk reduction of recurrent cryptogenic stroke in favor of PFO closure compared with medical therapy alone.
Because direct visualization of the PFO is not feasible in the majority of adults by conventional TTE, TCD can be performed using agitated saline to prove the presence of a shunt. In case of clinical suitability for potential percutan device closure, TEE with Valsalva manoeuvre is needed as a further step to give proof of right-to-left shunting. While TCD has the highest sensitivity for PFO, TEE has the advantage to map the morphology of the septum, the appendage, and the PFO-channel in high detail and helps design a future transcatheter closure.
Advanced echocardiography techniques using 2D and/or 3D methods has incremental impact in diagnosis, decision making and planning for clinical evaluation of transcatheter PFO or ASD closure and intraoperative guiding. 3D TTE/TEE examination of the heart overcomes most of the 2D TTE/TEE limitations avoiding angulation issues and geometric assumptions. Evaluation of PFO and ASD includes the detection and quantification of the size and shape of septal defects, the rims of tissue surrounding the defect and the degree and direction of shunting. Concomitant atrial septal abnormalities should be determined during preoperative examination and reevaluated during intraoperative guiding. It is important to emphasize that the guidewires and catheters might change the biomechanical characteristics of atrial septum, thus undiagnosed concomitant septal abnormalities might be revealed with relevant clinical impact regarding the size and the number of closure devices. Therefore, following the introduction of catheters, time should be dedicated for careful reevaluation of atrial septum using 2D or 3D TEE2,21. However, some centers use safely TTE guidance and fluoroscopy during percutaneous closure of PFO, which shortens the procedural time and prevents the need for general anesthesia or endotracheal intubation.22 Apart from structural assessment of atrial septum, attention should be made on functional parameters of the atria and ventricles to determine indication for transcatheter closure, mainly in case of ASD. Furthermore, transcatheter closure of ASD with significant left to right shunting may change the hemodynamics and the chamber affected with volume overload, thus RV enlargement and dysfunction may influence clinical decision and procedural closure planning to avoid postoperative adverse clinical outcome. It is important to characterize the size and function of the RV and LV, to assess the magnitude of shunting, tricuspid regurgitation, and to calculate the RV systolic pressure. Beyond conventional echocardiography, 2D and 3D speckle tracking provide sensitive functional parameters or cardiac MR and even an invasive right heart catheterisation can be performed if needed.
Ujawnienia
Authors declare no conflict of interest.
Podziękowania
Project no. NVKP 16-1–2016-0017 (’National Heart Program’) has been implemented with the support provided by the National Research, Development, and Innovation Fund of Hungary, financed under the NVKP 16 funding scheme. The research was financed by the Thematic Excellence Programme (2020-4.1.1.-TKP2020) of the Ministry for Innovation and Technology in Hungary, within the framework of the Therapeutic Development and Bioimaging thematic programs of the Semmelweis University.
Materiały
| Name | Company | Catalog Number | Comments |
| TomTec Imaging workstation | TomTec Imaging, Unterschleissheim, Germany | 4D LALV Function analysing software | |
| Ultrasound machine | Philips Epiq CvX | serial number US81881251 | X5-1 and X7 transducers |
| Wiwe external ECG single chanel recorder | Sanat Metal | 5-810-200-1611 | external ECG single chanel recorder |
Odniesienia
- Meier, B., et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. New England Journal of Medicine. 368 (12), 1083-1091 (2013).
- Silvestry, F. E., et al. et al.Guidelines for the Echocardiographic Assessment of Atrial Septal Defect and Patent Foramen Ovale: From the American Society of Echocardiography and Society for Cardiac Angiography and Interventions. Journal of the American Society of Echocardiography. 28 (8), 910-958 (2015).
- Saric, M., et al. Guidelines for the Use of Echocardiography in the Evaluation of a Cardiac Source of Embolism. Journal of the American Society of Echocardiography. 29 (1), 1-42 (2016).
- Krumsdorf, U., et al. Incidence and clinical course of thrombus formation on atrial septal defect and patient foramen ovale closure devices in 1,000 consecutive patients. Journal of the American College of Cardiology. 43 (2), 302-309 (2004).
- Canpolat, U., Gürses, K. M., Sunman, H., Kaya, E. B., Aytemir, K., Oto, A. Embolic stroke due to left atrial thrombus 2 years after PFO closure. Herz. 39 (1), 161-162 (2014).
- Butera, G., et al. Treatment of isolated secundum atrial septal defects: impact of age and defect morphology in 1,013 consecutive patients. American Heart Journal. 156 (4), 706-712 (2008).
- Badano, L. P., et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. European Heart Journal of Cardiovascular Imaging. 19 (6), 591-600 (2018).
- Hayashi, S. Optimal Analysis of Left Atrial Strain by Speckle Tracking Echocardiography: P-wave versus R-wave Trigger. Echocardiography. 32 (8), 1241-1249 (2015).
- Rudski, L. G., et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. Journal of the American Society of Echocardiography. 23 (7), 685-713 (2010).
- Wu, V. C., et al. Prognostic value of LA volumes assessed by transthoracic 3D echocardiography: comparison with 2D echocardiography. Journal of the American College of Cardiology: Cardiovascular Imaging. 6 (10), 1025-1035 (2013).
- Badano, L. P., et al. Left Atrial Volumes and Function by Three-Dimensional Echocardiography: Reference Values, Accuracy, Reproducibility, and Comparison With Two-Dimensional Echocardiographic Measurements. Circulation: Cardiovascular Imaging. 9 (7), (2016).
- Edvardsen, T., et al. The year 2015-16 in the European Heart Journal-Cardiovascular Imaging. Part II. European Heart Journal: Cardiovascular Imaging. 18 (12), 1322-1330 (2017).
- Galderisi, M., et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Europen Heart Journal: Cardiovascular Imaging. 18 (12), 1301-1310 (2017).
- Marriott, K., Manins, V., Forshaw, A., Wright, J., Pascoe, R. Detection of right-to-left atrial communication using agitated saline contrast imaging: experience with 1162 patients and recommendations for echocardiography. Journal of the American Society of Echocardiography. 26 (1), 96-102 (2013).
- Mojadidi, M. K., et al. et al Accuracy of conventional transthoracic echocardiography for the diagnosis of intracardiac right-to-left shunt: a meta-analysis of prospective studies. Echocardiography. 31 (9), 1036-1048 (2014).
- Mojadidi, M. K., Bogush, N., Caceres, J. D., Msaouel, P., Tobis, J. M. Diagnostic accuracy of transesophageal echocardiogram for the detection of patent foramen ovale: a meta-analysis. Echocardiography. 31 (6), 752-758 (2014).
- Staubach, S., et al. New onset atrial fibrillation after patent foramen ovale closure. Catheter and Cardiovascular Interventions. 74 (6), 889-895 (2009).
- Singh, H. S., Katchi, F., Naidu, S. S. PFO Closure for Cryptogenic Stroke: A Review and Clinical Treatment Algorithm. Cardiology in Review. 25 (4), 147-157 (2017).
- Sanna, T., et al. Cryptogenic stroke and underlying atrial fibrillation. New England Journal of Medicine. 370 (26), 2478-2486 (2014).
- Prefasi, D., Martínez-Sánchez, P., Fuentes, B., Díez-Tejedor, E. The utility of the RoPE score in cryptogenic stroke patients ≤50 years in predicting a stroke-related patent foramen ovale. International Journal of Stroke. 11 (1), 7-8 (2016).
- Yamano, M., et al. et al Appropriate selection of echocardiographic guidance for transcatheter atrial septal defect closure. International Journal of Cardiovascular Imaging. 36 (5), 855-863 (2020).
- Oto, A., et al. Transthoracic echocardiography guidance during percutaneous closure of patent foramen ovale. Echocardiography. 28 (10), 1074-1080 (2011).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaPrzeglądaj więcej artyków
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone