Method Article
Guide Wire Assisted Catheterization and Colored Dye Injection for Vascular Mapping of Monochorionic Twin Placentas
W tym Artykule
Podsumowanie
Vascular mapping of monochorionic (MC) twin placentas after birth provides a means for detailed demonstration of vascular connections between the twins’ circulations. Imbalance of these connections is thought to play a pivotal role in the development of complications of MC twinning including twin-to-twin transfusion syndrome.
Streszczenie
Monochorionic (MC) twin pregnancies are associated with significantly higher morbidity and mortality rates than dichorionic twins. Approximately 50% of MC twin pregnancies develop complications arising from the shared placenta and associated vascular connections1. Severe twin-to-twin syndrome (TTTS) is reported to account for approximately 20% of these complications2,3. Inter-twin vascular connections occur in almost all MC placentas and are related to the prognosis and outcome of these high-risk twin pregnancies. The number, size and type of connections have been implicated in the development of TTTS and other MC twin conditions. Three types of inter-twin vascular connections occur: 1) artery to vein connections (AVs) in which a branch artery carrying deoxygenated blood from one twin courses along the fetal surface of the placenta and dives into a placental cotyledon. Blood flows via a deep intraparenchymal capillary network into a draining vein that emerges at the fetal surface of the placenta and brings oxygenated blood toward the other twin. There is unidirectional flow from the twin supplying the afferent artery toward the twin receiving the efferent vein; 2) artery to artery connections (AAs) in which a branch artery from each twin meets directly on the superficial placental surface resulting in a vessel with pulsatile bidirectional flow, and 3) vein to vein connections (VVs) in which a branch vein from each twin meets directly on the superficial placental surface allowing low pressure bidirectional flow. In utero obstetric sonography with targeted Doppler interrogation has been used to identify the presence of AV and AA connections4. Prenatally detected AAs that have been confirmed by postnatal placental injection studies have been shown to be associated with an improved prognosis for both twins5. Furthermore, fetoscopic laser ablation of inter-twin vascular connections on the fetal surface of the shared placenta is now the preferred treatment for early, severe TTTS.
Postnatal placental injection studies provide a valuable method to confirm the accuracy of prenatal Doppler ultrasound findings and the efficacy of fetal laser therapy6. Using colored dyes separately hand-injected into the arterial and venous circulations of each twin, the technique highlights and delineates AVs, AAs, and VVs. This definitive demonstration of MC placental vascular anatomy may then be correlated with Doppler ultrasound findings and neonatal outcome to enhance our understanding of the pathophysiology of MC twinning and its sequelae. Here we demonstrate our placental injection technique.
Protokół
1. Preparation of the placenta
- The placenta should be acquired from the delivery room as soon as possible after delivery to minimize clot formation, desiccation and overall deterioration of the tissue.
- Care should be taken to ensure that the placenta is not exposed to formalin or other fixatives.
- Standard BSL2 precautions for human tissue should be maintained and personnel should wear a mask, gown, gloves and shoe covers.
- Place the placenta in a large plastic or metal bowl that has precut holes to allow for the drainage of fluid. This bowl should be placed inside a larger stainless steel bowl to prevent spillage.
- Wash the placenta with warm saline.
- For better placental visualization, use Metzenbaum scissors to excise the inter-twin amniotic membranes being sure not to injure the placenta itself. Leave a ½ cm cuff of inter-twin membrane in place. (Figure 1A).
2. Catheterization of the placental vessels
- Identify the cords of the respective twins. The obstetricians usually identify each twin by the number of clamps placed on each cord. Be sure to confirm which cord supplied the presenting twin (twin A).
- One at a time, keeping track of which cord is which, transect each cord just below the clamps (Figure 1B). Gently milk clot out from the vessels (Figure 1C). At the cut edge of the cord there will be one vein and at least one, usually two, arteries. Arteries are identified by their relatively smaller diameter (compared to the vein) and surrounding muscular cuff (Figure 1D).
- Use a standard radial arterial line guide wire, 0.46 mm diameter and 80 cm long (Arrow, Reading PA, USA), with a soft tip to gain access to an arterial orifice on the cut edge of twin A's cord (Figure 1E).
- The guide wire should be placed a minimum of 3 cm into the vessel. Gentle counter tension on the nonvascular portion of the cut edge of the cord using a Kelly clamp greatly facilitates advancement of the wire. Minor turning of the cord to straighten the tortuous vessels may help with wire advancement. Care should be taken to avoid false passages.
- Using the Seldinger technique, thread a 20 cm long 0.6-1.19 mm inner diameter polyethylene catheter (Intramedic, Batavia IL, USA) with a bluntly beveled distal end over the wire into the artery (Figure 1F). Care must be taken not to dislodge the wire while advancing the catheter. Remove the wire after catheter is seated at least 3 cm into the vessel.
- Alternatively, some groups have had success without use of a guidewire and direct cannulation of the umbilical vessels with umbilical artery catheters. Although, this technique works well in our hands the use of a guidewire has decreased the time it takes us to complete the procedure.
- Attach an 18 G blunt tip needle (BD Biosciences, Franlik Lakes, NJ, USA) to the proximal end of the tubing. Ensure proper placement of the catheter by injecting a small amount of saline into the vessel and observing clearing of distal arteries. Gentle finger sweeps on the vessels while injecting saline may help facilitate movement of any residual clots.
- Carefully repeat steps 2.3 to 2.6 for the vein of twin A with attention to avoid dislodging the arterial catheter.
- Tie a piece of umbilical tape 1 cm distal to the cut edge around the cord and catheters. Ensure a tight seal to avoid back flow.
- Repeat step 2.3 to 2.9 for the cord of twin B (the non-presenting twin) such that there are catheters in an umbilical artery and vein of each twin secured with umbilical tape and both circulations have been infused with saline (Figure 2).
3. Injection of colored dye into the placental vessels
- Pathology dye, barium suspensions, gelatin or other viscous colored dyes can be used to visualize the placental vasculature. Choose four contrasting colors with which to inject the arteries and veins of twins A and B. The colors for the artery and vein for each twin should be readily distinguishable. Superficial anastomoses should be detectable by dye mixing and the formation of a different (blended) easily detectable color.
- Use a 3ml syringe to hand inject the artery of twin A with dye at low pressure. Gently sweep with one or two fingers along the vessels in the direction of dye flow to ensure filling of the entire vascular tree. If a superficial vascular anastomosis is identified, manual occlusion of the feeding vessel can be employed to allow the rest of the higher resistance vascular bed to fill (Figure 3A).
- Use a separate 3ml syringe to hand inject the artery of twin B (Figure 3B).
- Repeat steps 3.2 and 3.3 for the venous injections.
- If dye leaks from an injured vessel, repair should be performed with a fine suture and a needle driver. Take care not to suture ligate the whole vessel.
- Using a high-resolution digital camera take an image after each injection. After all injections are complete, remove the specimen from the bowls, place against a color neutral background and re-image (Figure 4). Document the number and type of connections seen between the twins' circulations.
4. Representative Results:
Artery to artery anastomoses (AAs) have been shown to be "protective" as they are associated with a significant decreased risk of TTTS and with improved outcomes for both twins5. Figure 4 demonstrates an injected MC twin placenta. An AA had been prospectively identified by in utero Doppler ultrasound. This finding was confirmed by the mixing of twin A arterial (yellow) and twin B arterial (blue) dye in a communicating arterial structure (green, arrow). An AV anastomosis with artery from twin A (yellow) and vein from twin B (orange) is also demonstrated (arrow head). Figure 5 and 6 depict photographs of two other placental specimens we injected.

Figure 1. (A) The amniotic membrane is carefully removed from the fetal surface of the shared MC placenta with Metzenbaum scissors. (B) A clean edge of the umbilical cord of twin A is exposed by proximal transection with Metzenbaum scissors. (C) Clot is milked from the cord by manual compression. (D) The umbilical arteries (arrowheads) and vein (arrow) of twin A are identified. (E) After placement of a Kelly clamp on the avascular portion of the cut surface of the cord for traction, a guide wire is placed in the umbilical artery of twin A and gently advanced through the tortuous vessel. (F) A small catheter is then advanced over the guidewire into the vessel lumen using the Seldinger technique.

Figure 2. Catheters have been placed in one umbilical artery and in the umbilical vein of each twin. These catheters are secured in place with umbilical tape ties around the entire cord. The correct positioning of each catheter has been confirmed and intraluminal clots have been cleared by the injection of warmed normal saline.
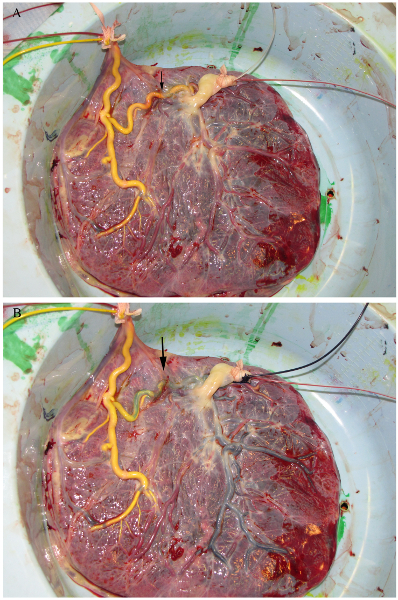
Figure 3. (A) The arterial circulation of twin A is injected with yellow dye. Contrast clearly passes across the vascular equator into the arterial circulation of twin B. (B) The arterial circulation of twin B is injected with blue dye. Admixing of the yellow dye and blue dye results in green dye within the demonstrated AA anastomosis (arrow).
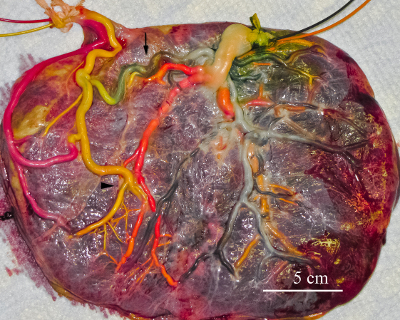
Figure 4. The vein of twin A (red) and the vein of twin B (orange) have been injected. The AA anastomosis (arrow) and an AV anastomosis, with flow directed from twin A toward twin B, (arrowhead) are delineated.
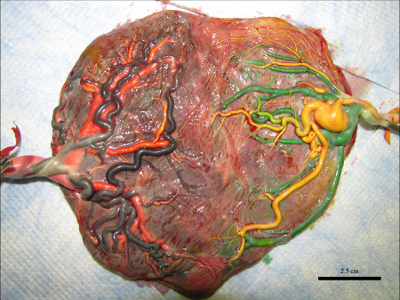
Figure 5. Example of MC twin placenta that underwent laser therapy after postnatal injection. The donor twin's artery and vein are in yellow and green respectively. The recipient artery and vein are in blue and orange respectively. No residual connections between the circulations were detected.

Figure 6. Example of MC twin placenta after injection. The left sided twin's artery and vein are in yellow and red respectively. The right-sided twin's artery and vein are in blue and orange respectively. An AA (arrowhead) and VV (arrow) are visible on the placental surface.
Dyskusje
Vascular mapping of MC twin placentas by dye injection is a valuable procedure for assessing complicated, clinically-treated cases and for further enhancing our understanding of MC twinning. Coordination with the obstetric team to ensure expeditious acquisition of an intact placental specimen is crucial. Desiccation or prolonged storage of the tissue prior to injection may lead to vessel injury and extravasation of dye. Fixation of the placenta must be avoided, because cross-linked blood clots will block perfusion of intravascular dye. A critical and difficult step in this procedure is cannulation of the umbilical arteries and veins. These vessels, in particular the arteries, are fragile and tortuous. We have found that using a compliant guide wire greatly facilitates successful cannulation and prevents puncture and creation of a false lumen. "Straightening" tortuous arteries by rotating the entire cord on its long axis also facilitates placement of wires and catheters. If a perforation does occur, the cord can be re-transected proximal to the perforation. The ability to re-transect the cord, however, is obviously limited by the length of cord. We recommend a minimum 3 cm stump of cord to ensure sufficient length to secure the catheters. Furthermore, catheterization of only one umbilical artery is feasible because of the anastomosis of Hyrtl between the two arteries near the base of the cord. Placement of the arterial catheter distal to this anastomosis will result in inadequate arterial tree filling. After wire placement, catheters are placed into the vessels using the Seldinger technique. Other potential pitfalls include using catheters too large to fit in a preterm placental artery and the inadvertent advancement of the wire causing vessel perforation. These pitfalls can be avoided by obtaining thinner catheters and wires as well as having an assistant immobilize the wire as the catheter is advanced.
Before saline is used for "clearing", small amounts of saline should be injected to confirm correct intraluminal catheter placement. If wire placement is difficult and only a small length of vessel is entered, temporarily placing the catheter over the wire and injecting 500 uL of saline may clear a path and straighten the vessel allowing for wire advancement. Care must be taken not to inject fluid into the extravascular space, as this will compress the vessels making cannulation even more difficult. Some authors have suggested that air injection is a suitable method for delineating inter-twin connections7. We feel this technique does not sufficiently illustrate placental vascular anatomy in a reliable, reportable and measurable way.
Vascular mapping of placental vessels in MC twin pregnancies is of great value in enhancing our understanding of MC twin complications and in assessing the efficacy and sequelae of fetal intervention with laser ablation. In addition to reports such as this demonstrating vascular connections on the fetal surface of the shared MC placenta, some investigators have used angiography,8 casting9 and post-injection sectioning10 to confirm and further characterize the angioarchitecture. The use of radiopaque dyes and high-resolution computer tomography with 3D reconstruction may also be of use in the future. The method we describe in this paper uses a simple Seldinger technique that is applicable to cannulating any vessel. The technique is efficient and reliable; its increased use will play a critical role in understanding and caring for complicated MC twin pregnancies.
Ujawnienia
No conflicts of interest declared.
Materiały
| Name | Company | Catalog Number | Comments |
| Perforated plastic bowl | QuickMedicalMedical Equipment and Supplies | Polarware PA75 | Perforations can be made with a drill |
| Stainless steel bowl | Narang Medical Limited | HH517 | |
| Normal Saline | Fisher Scientific | 50983204 | |
| 0.6-1.9 mm ID polyethylene tubing | Intramedic | 7436 | |
| Arterial line guide wire (0.46 mm) | Arrow International | PW-18080 | Soft tip |
| 18 G Blunt Needles | BD Biosciences | 305180 | |
| Umbilical Tape | QC supply | 140895 | |
| Metzenbaum scissors | Cole-Parmer | EW-10921-04 | |
| Kelly clamp | Cole-Parmer | EW-10918-20 | |
| 3 ml syringe | Covidien | 1180300555 | |
| Pathology Dye | Bradley Products | 7365-x | |
| Digital Camera | Panasonic | Lumix-TZ50 |
Odniesienia
- Rand, L., Lee, H. Complicated monochorionic twin pregnancies: updates in fetal diagnosis and treatment. Clin Perinatol. 36, 417-430 (2009).
- Sebire, N., Talbert, D. Twin-to-twin transfusion syndrome results from dynamic asymmetrical reduction in placental anastomoses: a hypothesis. in Placenta. , (2001).
- Machin, G. A., Keith, L. G. . An atlas of multiple pregnancy: biology and pathology. , (1999).
- Machin, G. A., Feldstein, V. A., van Gemert, M. J., Keith, L. G., Hecher, K. Doppler sonographic demonstration of arterio-venous anastomosis in monochorionic twin gestation. Ultrasound Obstet Gynecol. 16, 214-217 (2000).
- Denbow, M. L., Cox, P., Taylor, M., Hammal, D. M., Fisk, N. M. Placental angioarchitecture in monochorionic twin pregnancies: Relationship to fetal growth, fetofetal transfusion syndrome, and pregnancy outcome. American Journal of Obstetrics and Gynecology. 182, 417-426 (2000).
- Taylor, M. J. O. Doppler detection of arterio-arterial anastomoses in monochorionic twins: feasibility and clinical application. Human Reproduction. 15, 1632-1636 (2000).
- Bermúdez, C. Placental types and twin-twin transfusion syndrome. American Journal of Obstetrics and Gynecology. 187, 489-494 (2002).
- Lewi, L. Intertwin anastomoses in monochorionic placentas after fetoscopic laser coagulation for twin-to-twin transfusion syndrome: is there more than meets the eye. Am J Obstet Gynecol. 194, 790-795 (2006).
- Wee, L. Y. Characterisation of deep arterio-venous anastomoses within monochorionic placentae by vascular casting. Placenta. 26, 19-24 (2005).
- Paepe, M. E. D. e., Burke, S., Luks, F. I., Pinar, H., Singer, D. B. Demonstration of placental vascular anatomy in monochorionic twin gestations. Pediatr Dev Pathol. 5, 37-44 (2002).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone