Method Article
Combination of Anatomical Plates and Rotator Cuff Reinforcement for Minimally Invasive Treatment of Greater Tuberosity Fractures of the Humerus
* Diese Autoren haben gleichermaßen beigetragen
In diesem Artikel
Zusammenfassung
Here, we present a protocol to utilize anatomical plates alongside rotator cuff reinforcement in a minimally invasive surgery to efficiently treat humerus greater tuberosity fractures, promising quicker healing and improved stability.
Zusammenfassung
Greater tuberosity fractures of the humerus can be challenging to manage due to their complex anatomy and the potential for compromised shoulder function. We present a novel technique for treating greater tuberosity fractures utilizing specialized anatomical plates and rotator cuff reinforcement. The technique involves the use of an anatomically T-shaped plate designed specifically for the greater tuberosity region of the humerus, allowing for precise fixation and stability. Additionally, rotator cuff reinforcement is performed using sutures to enhance structural integrity and promote early mobilization. The simplified process is as follows: After administering anesthesia, a 3 cm incision is made along the lateral aspect of the shoulder to precisely expose the fracture site of the greater tuberosity. A suture of size 5 is skillfully threaded through the tough rotator cuff tendon to securely attach the proximal humerus to the anatomical plate after the greater tuberosity has been reduced. Intraoperative fluoroscopy is utilized to verify the accurate positioning of plates and screws. After ensuring everything is correct, the surgery concludes.
Einleitung
Greater tuberosity fractures of the humerus are a common type of upper limb fracture, often accompanied by joint pain and functional impairment1. Traditional treatment methods are associated with larger incisions and longer recovery periods.We introduce a refined treatment protocol that maximizes patient outcomes and minimizes surgical invasiveness. Stemming from a growing need for efficient fracture management, this technique's rationale is grounded in the principle of expedited patient recovery with minimal postoperative complications. In recent years, the development of minimally invasive techniques has garnered attention2. The application of specialized anatomical plates combined with rotator cuff reinforcement for fixation has become increasingly favored. The technique stands as a superior alternative to traditional methods characterized by their larger incisions and protracted recovery times. Comparative advantages of this approach, as evidenced by previous studies, include diminished tissue trauma, faster rehabilitation, and reinforced stability, crucially reducing the risks associated with anchor pull-out-an issue prevalent in traditional procedures3,4. In current literature, this technique is gaining recognition for its potential to transform the management of humeral fractures. It aligns with the current trend toward minimally invasive surgeries prioritizing functional recovery and patient quality of life. Candidates suitable for this method are those who stand to benefit from a swift return to daily activities and optimal cosmetic outcomes due to minimized scarring.
This article will provide a detailed description of the procedural steps of this technique and highlight its advantages in treating greater tuberosity fractures of the humerus5. This innovative approach offers several distinctive advantages. Firstly, the minimally invasive nature of the procedure translates to reduced tissue trauma and hastened postoperative rehabilitation. This facilitates early engagement in rehabilitative exercises, thereby promoting enhanced functional recovery. Secondly, adding rotator cuff reinforcement makes the fracture fixation more stable, which lowers the risk of anchor pull-out after surgery. Moreover, the diminished extent of postoperative trauma contributes to minimized scar formation, ultimately enhancing patients' quality of life. As technological advancements continue, the application of this minimally invasive treatment modality is poised to gain wider traction in the realm of greater tuberosity fracture management. Our study demonstrates that the utilization of specialized anatomical plates in conjunction with rotator cuff reinforcement presents a novel and effective avenue for addressing greater tuberosity fractures of the humerus. Through its amalgamation of reduced trauma, enhanced stability, and expedited recovery, this technique provides a compelling alternative for patients with these fractures, heralding a new era of optimized treatment strategies.
The inclusion criteria include (i) Diagnosis of isolated greater tuberosity fracture: Patients presenting with radiologically confirmed isolated greater tuberosity fractures suitable for open reduction and internal fixation. (ii) Age: Adult patients aged 18 and above. (iii) Symptomatic fracture: Patients experiencing functional impairment and pain due to the fracture. (iv) Bone quality: Adequate bone quality that is amenable to secure surgical fixation with screws and plates. (v) Conservative treatment failure: Patients who have not achieved satisfactory results with non-surgical treatment methods after a reasonable period. (vi) Patient consent: Willingness and ability to give informed consent for surgery and to comply with postoperative rehabilitation protocols.
The exclusion criteria include (i) Polytrauma cases: Patients with multiple injuries where the patient's overall condition contraindicates surgical intervention. (ii) Pathological fracture: Fracture resulting from primary or metastatic bone tumors. (iii) Poor bone quality: Severe osteoporosis or other metabolic bone diseases that compromise the integrity of fixation. (iv) Systemic infections or local skin infections: Presenting a risk of postoperative infection due to compromised immunity or existing infection at the surgical site. (v) Neurovascular compromise: Pre-existing neurovascular injuries at the surgical site that could be exacerbated by the procedure. (vi) Medical comorbidities: Uncontrolled diabetes, severe cardiovascular, pulmonary, or other systemic diseases that pose an unacceptable anesthetic or surgical risk. (vii) Cognitive impairment: Conditions that impede the patient's understanding and cooperation with surgical and postoperative requirements. (viii) Previous surgery or deformity: Prior surgical procedures or deformities in the affected area that may influence the current surgical approach and outcome. (ix) Patients unable to follow postoperative protocol: Lack of a support system or other socio-economic factors that prevent adherence to postoperative care and rehabilitation instructions.
Protokoll
Written informed consent was obtained from the patients for publication. This surgical protocol adheres to the ethical standards established by our institution's human research ethics committee.
1. Preoperative preparation and anesthetic assessment
- Preoperative preparation
- Prior to the surgery, ensure thorough communication with the patient. Explain the purpose, method, risks, and expected outcomes of the surgery.
- Obtain written informed consent from the patient to ensure their understanding and agreement to undergo the minimally invasive procedure.
- Perform a comprehensive preoperative assessment for the successful treatment of greater tuberosity fractures of the humerus. This assessment process typically involves various imaging techniques, such as computed tomography (CT) scans, X-rays, and magnetic resonance imaging (MRI), to ensure a comprehensive understanding of the fracture and provide essential information for the surgical plan (Figure 1).
- Anesthesia assessment and preparation
NOTE: An anesthesiologist performs anesthesia assessment and preparation.- Prior to the surgery, assess the patient's anesthesia requirements to ensure suitability for general anesthesia.
- Evaluate the patient's respiration, cardiovascular system, and other physiological indicators. Develop a personalized anesthesia plan based on the patient's health condition and the type of surgery.
- Anesthesia induction and maintenance
- Before the commencement of the surgery, administer anesthesia drugs to the patient through a vein to induce a state of unconsciousness. Once the patient loses consciousness, maintain the patient's respiration using a ventilator.
NOTE: In general anesthesia, the patient will not experience pain and will remain unconscious throughout the surgical procedure.
- Before the commencement of the surgery, administer anesthesia drugs to the patient through a vein to induce a state of unconsciousness. Once the patient loses consciousness, maintain the patient's respiration using a ventilator.
2. Minimally invasive surgical procedure and fixation technique
- Perform surgical site preparation and incision:
- Prepare the surgical site with antiseptic solution in a circular motion from the incision site outward.
- Drape the patient, exposing only the operative field. Precisely mark and create a 3 cm incision along the lateral aspect of the shoulder, using a scalpel blade strategically positioned to unveil the fracture site of the greater tuberosity.
NOTE: This incision facilitates optimal visualization of both the proximal humerus and the insertion point of the rotator cuff, laying the foundation for seamless reduction and subsequent fixation of the fracture (Figure 2).
- Reduction of greater tuberosity
- Pass nonabsorbable sutures of size 5 through the rotator cuff tendon at 2 cm intervals using a suture passer or needle driver. Reduce the greater tuberosity fracture by drawing sutures.
- Execute the reduction of the greater tuberosity fracture with meticulous attention, ensuring impeccable alignment of the fractured segments.
NOTE: The selection of a fitting anatomical plate is imperative; its strategic placement on the proximal humerus primes the area for the upcoming fixation process. This step demands precision and an unwavering commitment to achieving anatomical congruency.
- Rotator cuff reinforcement and fixation
- Select a fitting anatomical plate sized appropriately for the patient's humerus. Position the plate on the lateral aspect of the humerus using image guidance (Figure 3A).
- Secure the plate with screws of the correct length, typically ranging from 25-45 mm. Tie the sutures over the plate to secure the cuff to the plate (Figure 3B).
NOTE: The integrity of this fixation is paramount, as it directly influences the robustness of the eventual fracture union. Each suture, meticulously placed, serves as a guardian of stability, ushering in the potential for a steadfast recovery.
- Intraoperative fluoroscopy
- Position the fluoroscope to capture AP (anteroposterior) and lateral views of the operative site. Assess the reduction, plate, and screw positioning, adjusting as necessary to achieve proper anatomical alignment (Figure 4).
- Anesthesia monitoring
- Throughout the surgical procedure, continuously monitor the patient's vital signs to ensure that indicators such as blood pressure, heart rate, and respiration remain within safe ranges.
- Adjust the dosage of anesthesia drugs to maintain the patient's stable condition.
- Anesthesia conclusion and recovery
- After the surgery, gradually cease the administration of anesthesia drugs, allowing the patient to awaken from the state of unconsciousness.
- Transfer the patient to a recovery room, where skilled medical professionals will continue to monitor the patient's vital signs. This ensures a smooth awakening process and a gradual return to consciousness.
3. Postoperative care and rehabilitation plan
- Postoperative care and rehabilitation
- Upon the completion of the surgical procedure, the journey towards recovery commences. Suture the incision meticulously to ensure effective hemostasis and promote optimal wound healing.
- Postoperatively, guide the patient through a tailored rehabilitation plan orchestrated by healthcare professionals well-versed in the nuances of upper limb recovery.
- Early mobilization and range of motion
- Encourage early mobilization of the affected limb within the confines of medical guidance.
NOTE: Gentle, controlled movements aimed at preserving joint mobility and preventing stiffness play a pivotal role in the early stages of recovery.
- Encourage early mobilization of the affected limb within the confines of medical guidance.
- Gradual strength and functionality restoration
- As the healing progresses, emphasize gradual strength-building exercises tailored to the individual's progress. Collaborate with physical therapists to devise a regimen that strikes a balance between challenging the recovering limb and ensuring its safety.
- Follow-up and progress assessment
- Regular follow-up appointments enable the healthcare team to monitor the patient's progress and make necessary adjustments to the rehabilitation plan.
NOTE: Radiological assessments can gauge the degree of fracture healing and guide the next steps of the recovery journey.
- Regular follow-up appointments enable the healthcare team to monitor the patient's progress and make necessary adjustments to the rehabilitation plan.
- Patient education and empowerment
- Engage the patient in comprehensive education regarding their recovery process. Empower them with knowledge about expected milestones, potential challenges, and the crucial role they play in their own recovery.
NOTE: Informed patients are more likely to adhere to rehabilitation plans and contribute actively to their healing journey. The innovative approach of utilizing specialized anatomical plates in conjunction with rotator cuff reinforcement presents promising long-term outcomes. Beyond fracture healing, the potential for enhanced joint function and improved quality of life serves as an impetus for patients to commit to their rehabilitation journey.
- Engage the patient in comprehensive education regarding their recovery process. Empower them with knowledge about expected milestones, potential challenges, and the crucial role they play in their own recovery.
Ergebnisse
A patient meeting the above-described inclusion criteria underwent the minimally invasive technique for treating a fracture of the humeral greater tuberosity. Preoperative three-dimensional (3D) CT reconstruction shows a fracture of the humeral greater tuberosity (Figure 1). After administrating anesthesia, a 3 cm incision along the lateral aspect of the shoulder is precisely marked (Figure 2). The surgeon incises the skin along with the marker using a scalpel and separates subcutaneous tissue to unveil the fracture site of the greater tuberosity. Nonabsorbable sutures are passed through the rotator cuff tendon using a suture passer or needle driver. The greater tuberosity fracture is reduced by drawing sutures. A fitting anatomical plate is selected appropriately for the patient's humerus and positioned on the lateral aspect of the humerus (Figure 3A). The sutures are tied over the plate to secure the cuff to the plate (Figure 3B). Intraoperative fluoroscopy captures clear anteroposterior (AP) and lateral views of the operative site showing the fracture reduction, plate, and screw placement (Figure 4A,B).

Figure 1: Preoperative radiological images of greater tuberosity fractures of the humerus. In the image, the affected greater tuberosity is clearly depicted as fractured with evident displacement. Please click here to view a larger version of this figure.

Figure 2: Diagram of the surgical incisions. The transverse dashed line denotes the acromion. The vertical dashed line marks the surgical incision. Please click here to view a larger version of this figure.
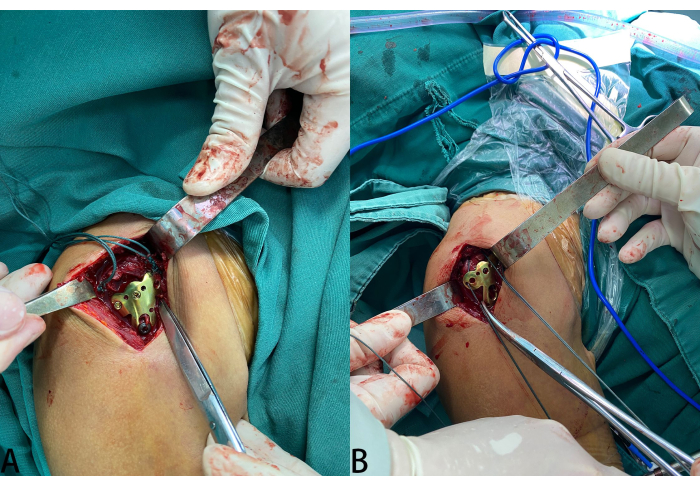
Figure 3: Surgical steps for rotator cuff reinforcement and fixation illustrative diagram. (A) Image depicting the sequential surgical steps involved in rotator cuff reinforcement and fixation. (B) Image highlighting the passage of size 5 sutures through the rotator cuff tendon and their secure attachment to the anatomical plate. Please click here to view a larger version of this figure.

Figure 4: Radiographs of fracture reduction and anatomical plate placement. (A) AP and (B) lateral radiographs showcasing the successful reduction of the greater tuberosity fracture and the precise placement of the anatomical plate on the proximal humerus. The alignment of fracture ends and the stable fixation achieved are evident. Please click here to view a larger version of this figure.
Diskussion
The incorporation of specialized anatomical plates coupled with rotator cuff reinforcement has revolutionized the management of greater tuberosity humerus fractures, offering a minimally invasive alternative that promulgates improved healing and functionality6,7,8. Critical steps in this innovative procedure include precise preoperative imaging to evaluate the fracture pattern, careful incision placement to minimize tissue damage, and meticulous plate positioning to ensure optimal fracture reduction and stability. The use of intraoperative fluoroscopy is key for accurate hardware placement, while the reinforcement of the rotator cuff is essential to prevent postoperative mobilization and expedite rehabilitation. It is important to take into consideration that the lower edge of the incision is in close proximity to the axillary nerve, and precautions should be implemented to prevent any potential nerve damage.
Modifications and troubleshooting are integral components of refining this technique. Surgeons have tailored the approach to account for variability in fracture patterns and patient anatomy by customizing plate shapes and employing different reinforcement materials. In cases where standard plates do not provide sufficient stability, custom 3D-printed plates may offer a solution9. Additionally, the technique's learning curve necessitates training to prevent complications such as screw misplacement or inadequate reduction. Troubleshooting includes the intraoperative assessment and potential repositioning of the hardware to ensure anatomical alignment10.
Nonetheless, the technique has its limitations. While minimally invasive, it is not free from risk. Potential complications include infection, nerve damage, and hardware failure, which may be more prevalent in osteoporotic bone or complex fractures11. There is also the limitation of the approach in significantly comminuted fractures where the rotator cuff itself may be severely injured, complicating the reinforcement aspect12.
The significance of this technique lies in its departure from traditional, more invasive methods. By reducing the surgical footprint and the associated soft-tissue damage, patients benefit from shorter recovery times, less pain, and decreased incidence of postoperative stiffness compared to traditional open methods13. These advantages are critical as they provide an enhanced pathway for patient recovery in both short-term and long-term scenarios.
In terms of future applications, ongoing research is focusing on integrating biologic therapies to augment healing and patient-specific instrumentation tailored by preoperative 3D models14. By assimilating innovative imaging techniques and virtual surgical planning, surgeons could further refine the precision of this technique. This could herald a new era of personalized orthopedic care that not only streamlines surgical procedures but also drastically improves patient-specific outcomes15.
The meticulous evolution of this minimally invasive technique stands as a testament to the progressive nature of orthopedic surgery, continuously striving for treatments that optimize healing, enhance functionality, and improve the quality of life for patients experiencing greater tuberosity fractures.
The application of specialized anatomical plates combined with rotator cuff reinforcement for minimally invasive treatment of greater tuberosity fractures of the humerus is an innovative and effective approach. By reducing trauma, providing stable fixation, and promoting early recovery, this method has the potential to improve postoperative pain and function, offering a better choice for the treatment of greater tuberosity fractures of the humerus.
Offenlegungen
The authors declare no conflicts of interest.
Danksagungen
None
Materialien
| Name | Company | Catalog Number | Comments |
| Anesthesia monitor | Drager | USRN-0094 | N/A |
| C-arm | GE | B3SS1700060 | Intraoperative fluoroscopy |
| ETHIBOND Excel polyester suture size 5 | Johnson&johnson | 130705031046294 | N/A |
| Fentanyl citrate injection | Renfu Pharmaceutical | 31D090113 | anesthesia drugs |
| Injection of Remifentanil Hydrochloride | Renfu Pharmaceutical | 30A11011 | anesthesia drugs |
| Marker pen | Deli Group Co., Ltd. | 6921734968258 | N/A |
| Needle deriver | Shanghai Medical Devices Co., Ltd. Surgical Instrument Factory | J32100 | N/A |
| Patient monitor | Drager | SQC19090042HA | N/A |
| Povidone-iodine | Hangzhou Minsheng Pharmaceutical Co., Ltd. | 532310292 | antiseptic solution |
| Propofol emulsion injection | Xi'an Libang Pharmaceutical Co., Ltd. | 12312072I | anesthesia drugs |
| Proximal humerus locking compression plate(T) | WEGO | MB66G | It is used for avulision fracture of the greater tuberosity of humerus. |
| Rocuronium bromide injection | Emeishan Tonghui Pharmaceutical Co., Ltd. | 23112001 | anesthesia drugs |
| Surgical blade | Hangzhou Huawei Medical Supplies Co., Ltd. | 20152020713 | N/A |
Referenzen
- Kong, L. P., Yang, J. J., Wang, F., Liu, F. X., Yang, Y. L. Minimally invasive open reduction of greater tuberosity fractures by a modified suture bridge procedure. World J Clin Cases. 10 (1), 117-127 (2022).
- George, M. S. Fractures of the greater tuberosity of the humerus. J Am Acad Orthop Surg. 15 (10), 607-613 (2007).
- Lee, W. Y., et al. Open reduction and stable internal fixation using a 3.5-mm locking hook plate for isolated fractures of the greater tuberosity of the humerus: A 2-year follow-up study using an innovative fixation method. Clin Orthop Surg. 13 (3), 293-300 (2021).
- Popp, D., Schöffl, V., Strecker, W. Osteosynthesis of displaced fractures of the greater tuberosity with the bamberg plate. Oper Orthop Traumatol. 28 (5), 392-401 (2016).
- Zeng, L. Q., et al. A new low-profile anatomic locking plate for fixation of comminuted, displaced greater tuberosity fractures of the proximal humerus. J Shoulder Elbow Surg. 30 (6), 1402-1409 (2021).
- Marinescu, R., Popescu, D. 3D prints are not a panacea, but definitely support orthopedic surgery. 2020 International Conference on e-Health and Bioengineering (EHB). , (2020).
- Marinescu, R., Popescu, D., Laptoiu, D. A review on 3D-printed templates for precontouring fixation plates in orthopedic surgery. J Clin Med. 9 (9), 2908 (2020).
- Godin, J. A., Katthagen, J. C., Fritz, E. M., Pogorzelski, J., Millett, P. J. Arthroscopic treatment of greater tuberosity avulsion fractures. Arthrosc Tech. 6 (3), e777-e783 (2017).
- Wixted, C. M., Peterson, J. R., Kadakia, R. J., Adams, S. B. Three-dimensional printing in orthopaedic surgery: Current applications and future developments. J Am Acad Orthop Surg Glob Res Rev. 5 (4), 00230 (2021).
- Koljonen, P. A., Fang, C., Lau, T. W., Leung, F., Cheung, N. W. Minimally invasive plate osteosynthesis for proximal humeral fractures. J Orthop Surg. 23 (2), 160-163 (2015).
- Falez, F., et al. Minimally invasive plate osteosynthesis in proximal humeral fractures: One-year results of a prospective multicenter study. Int Orthop. 40 (3), 579-585 (2016).
- Thaeter, M., Kobbe, P., Verhaven, E., Pape, H. -. C. Minimally invasive techniques in orthopedic trauma. Curr Trauma Rep. 2, 232-237 (2016).
- Sohn, H. S., Jeon, Y. S., Lee, J., Shin, S. J. Clinical comparison between open plating and minimally invasive plate osteosynthesis for displaced proximal humeral fractures: A prospective randomized controlled trial. Injury. 48 (6), 1175-1182 (2017).
- Smith, B., Goldstein, T., Ekstein, C. Biologic adjuvants and bone: Current use in orthopedic surgery. Curr Rev Musculoskelet Med. 8 (2), 193-199 (2015).
- Andrés-Cano, P., Calvo-Haro, J., Fillat-Gomà, F., Andrés-Cano, I., Perez-Mañanes, R. Role of the orthopaedic surgeon in 3d printing: Current applications and legal issues for a personalized medicine. Rev Esp Cir Ortop Traumatol (Engl Ed). 65 (2), 138-151 (2021).
Nachdrucke und Genehmigungen
Genehmigung beantragen, um den Text oder die Abbildungen dieses JoVE-Artikels zu verwenden
Genehmigung beantragenThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Alle Rechte vorbehalten