Method Article
Clinical Application of Artificial Intelligence Preoperative Planning System Combined with Expert Database Retrieval in Complex Revision Hip Surgery
In This Article
Summary
This study proposes a novel artificial intelligence preoperative planning approach based on expert surgical case database retrieval in revision hip arthroplasty. Additionally, the technique was initially employed in five patients, exhibiting a reduction in operative time and intraoperative hemorrhage.
Abstract
Accurate preoperative planning in revision hip arthroplasty is crucial for achieving successful outcomes. To enhance the intuitive evaluation of acetabular bone defect severity and leverage previous successful experience in revision hip arthroplasty, this study proposes a novel approach based on expert surgical case database retrieval and is initially implemented in clinical application. In this study, five patients who required revision hip arthroplasty were preoperatively planned to employ the expert case database surgical planning system.The patient's imaging data was entered into the system and matched with cases in the expert case database. Based on the expert's surgical experience, a revision surgery plan was recommended. If no suitable case was found, the model and position of the prosthesis were planned based on patient-specific reconstruction results. A total of five patients were enrolled in this study, four males and one female, with a mean age of 50.6 years. The diagnosis was aseptic prosthesis loosening after hip arthroplasty. The mean operative time was 123.2 min, and the mean intraoperative hemorrhage was 672 mL. No intraoperative complications, such as vascular or nerve injury, were observed. In Case 2, for instance, the application of this innovative planning scheme enabled the surgeon to delineate the revision surgery plan for this patient in the preoperative period, thereby reducing the operative time and intraoperative hemorrhage. Furthermore, patients could be apprised of the outcomes of analogous cases in advance. Leveraging a big data analysis approach through our comprehensive case database enables automated identification of matching expert treatment plans throughout the entire process. This particularly benefits inexperienced orthopedic surgeons by providing accurate guidance on surgical strategies to assist them in selecting appropriate prosthetic sizes and mounting positions. Additionally, the matching results can offer patients visualizations depicting predicted postoperative outcomes.
Introduction
The increasing prevalence of primary total hip arthroplasty (THA) has led to a corresponding rise in the necessity for revision arthroplasty due to a number of factors, including aseptic loosening, infection, recurrent dislocation, and periprosthetic fracture1. Compared to primary hip arthroplasty, revision hip surgery is a more technically complex and clinically challenging procedure, with higher mortality rates2, higher healthcare costs3, and greater complication risks4.
In revision hip arthroplasty, the reconstruction of acetabular bone loss and the selection of prosthesis are paramount in determining the success of the surgery. The orthopedic surgeon needs to assess the residual bone stock and the altered anatomy, aiming for adequate initial stability of the newly implanted acetabular cup1. Consequently, precise preoperative planning is crucial to guide available treatment options.
Currently, orthopedic surgeons are responsible for conducting a comprehensive assessment and planning of revision arthroplasty based on preoperative imaging findings and their own surgical experience. Nevertheless, this will present a significant challenge for the inexperienced surgeon.
With the development of artificial intelligence (AI) technology, it has been increasingly used in orthopedic surgery, primarily for image segmentation, diagnosis, and classification of pathologies and implants5. Meanwhile, AI is beginning to achieve initial success in assisting primary THA6. However, intelligent preoperative planning for revision hip arthroplasty remains a blank slate. AI has a promising future in hip revision surgery, particularly in the assessment of bone defects. These defects are unique to each patient, and while they exhibit certain patterns, the traditional Paprosky classification method lacks the precision required to fully characterize them. Nevertheless, AI is capable of extracting more detailed information from image data, offering a promising avenue for enhancing the accuracy and precision of bone defect assessment. We developed a novel AI-assisted preoperative planning system to guide orthopedic surgeons' decisions about revision arthroplasty based on expert surgical case database retrieval.
We first established a novel method for acetabular bone defect reconstruction, quantifying and typing acetabular bone defects. Subsequently, we constructed a hip revision case database by collecting clinical and imaging data on 200 hip revision surgical cases from a senior national expert. The database consists of preoperative computed tomography (CT), preoperative X-Ray, postoperative X-ray, and patient demographics. We can match cases in the database based on the current bone defect characteristics of patients scheduled for surgery and find the most similar case scenarios to provide the surgeon with a preoperative reference. This approach allows the surgeon to have a preoperative idea of the acetabular revision protocol, reducing the intraoperative trial and error time.
Protocol
The study received permission from the Ethics Committee of Luoyang Orthopedic-Traumatological Hospital of Henan Province. Additionally, this study was based on imaging data and would not harm the volunteers or disclose their information. Therefore, by national legislation and institutional requirements, there was no need for participants or their legal guardians/next of kin to sign an informed consent form.
1. Image import
- Import the original CT data of the patient's bilateral total hip. Open the medical image processing software, select Import Data and click Local Data to import the original CT data of the patient. Figure 1 shows the image import interface.
2. Recovery of acetabular bone defect on the affected side
- Determine whether the patient has a unilateral or bilateral lesion. Select the Measurement tool and use the mouse to draw a rectangular box on the image, directly measuring the HU (Hounsfield Unit, HU) value of the hip bone area. Consider metal present when the HU value exceeds 1000 and designate that area as the affected hip joint.
3. Image segmentation and reconstruction
- Select the image data of the patient to plan. Click the Automatic Segmentation option, the CT value of 400 is selected by default for hip bone coarse segmentation.
- Select the Edit button to manually adjust the segmentation results of each part of each layer. Then, select the 3D Reconstruction option to complete the 3D reconstruction calculation of the patient's site. The reconstructed 3D model mainly includes the left/right hip bones and the left/right femur regions. As shown in Figure 2, different parts are displayed with different colors.
4. Acetabular bone defect partition and defect amount calculation
- For patients with unilateral hip surgery, select the 3D Model of the Healthy Side. Use the mirror function to align it with the anatomical structure of the affected side. This will complete the reconstruction of the hip joint restoration model.
- For patients with bilateral hip surgery, open the standard model library and select the Hip Model that is most similar to the patient's anatomy as the restoration model.
- Click the Partition option to divide the 3D model of the hip defect (affected side) reconstructed in step 2 and the 3D model of the hip restored in step 3. Then, click the Difference Operation option to perform the difference operation on the two partitioned hip bone models to calculate the acetabular defect. The hip bone model will be divided into different regions according to Qin's method7, as shown in Figure 3.
NOTE: Due to the focus on 3-Point fixation (rami ischii, rami ossis pubis, and anterosuperior part of the acetabulum) of the acetabular cup within the boundaries of the acetabular wall, the acetabular was divided into 3 equal parts every 120°, defined as the cranial roof, anterior column, and posterior column, excluding the medial wall. To guide surgical procedures, fabricate the sub-layers based on the acetabulum diameter. It was determined that the inner layer must lie between 54 mm and 62 mm and the outer layer must lie between 62 mm and 70 mm for men. The inner layer lie between 50 mm and 58 mm and the outer layer lie between 58 mm and 66 mm for women.
5. Expert hip revision database search - acetabular defect planning
- Open the expert case base and use the calculated acetabular defect volume as described above as input for retrieval. Select the measurement tools to assess the relevant planning parameters on the preoperative and postoperative X-ray films of the retrieved cases and obtain the planning data.
- Open the expert case base and enter the type and amount of hip defect for automatic retrieval. The corresponding cases' information in the database will be obtained, including preoperative and postoperative images of similar cases and the doctor's planning parameters (implant size, position, etc.).
- The search results will be presented in order of similarity from highest to lowest. Let the doctor select the most similar cases. The complete procedure is shown in Figure 4.
- If a similar case cannot be found in the above database, adopt the result of the model reconstruction from step 2, using the center of the intact acetabulum as the center of the acetabular cup. By default, the ante version angle of the acetabular cup is 20°, and the abduction angle is 40° (this rule is clinically defined).
NOTE: After planning, the surgeon is able to anticipate the surgical procedure and prepare the prosthesis and supporting instruments with greater precision. This approach eliminates the possibility of encountering a situation where the correct prosthesis is not available during the operation. Moreover, the recommended solution is employed directly during the operation, obviating the need for alternative solutions, detours, or protracted trial and error processes.
Results
Currently, we applied this method in five cases of patients who underwent revision hip arthroplasty, including four men and one woman. The ages ranged from 42 to 67 years. They were diagnosed as aseptic prosthesis loosening after hip arthroplasty and classified based on the Paprosky classification8. The mean operative time for the five patients was 123.2 min, with a mean intraoperative blood loss of 672 mL. The operative time is the overall time, including femoral stem prosthesis revision. The details of the patients are shown in Table 1, and the reconstruction results are displayed in Figure 5.
Take case two as an example: the patient is a 67-year-old female who underwent a THA 13 years ago. She presented to the hospital in January 2024 with hip pain and dysmobility, which had persisted for 3 years. The diagnosis was prosthesis loosening after THA, Paparosky classification as type IIC, and revision hip arthroplasty was proposed. We imported preoperative CT data of the patient into the system and matched it to that of a 58-year-old male patient seen in November 2017 who exhibited a remarkably similar acetabular bone defect. At that time, the surgical procedure was conducted using the Jumbo cup in conjunction with the compression bone grafting technique, which resulted in complete initial stability, favorable outcomes at the 5-year follow-up, and reliable prosthesis stability. A consistent surgical plan (Jumbo cup with a compression bone grafting technique) was employed for this patient. The process has been shown to reduce the time spent on intraoperative planning, as well as the time spent retrieving and replacing various types of pads and jumbo cups. Consequently, it has been demonstrated to reduce bleeding and the risk of infection. Due to the necessity for simultaneous revision of the stem side, intraoperative bleeding reached 690 mL, yet intraoperative acetabular stability was satisfactory. The patient has been under observation for 8 months, during which reliable results have been obtained, and the affected hip has demonstrated good functionality (Figure 6). The patient exhibited no complications, including pain, dysfunction, imaging indicative of prosthesis in position, normal inflammatory markers, and no evidence of infection or secondary loosening of the prosthesis.

Figure 1: Image import interface of the system. The system incorporates both local and PACS import functions. Please click here to view a larger version of this figure.
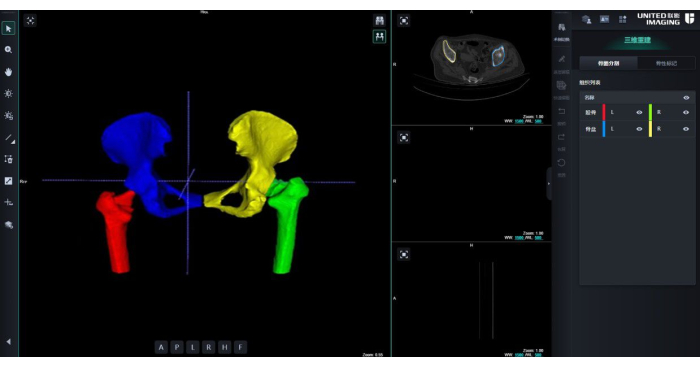
Figure 2: Reconstructed 3D model. Different parts are shown in different colors. Blue: right acetabular; Red: right femora; Yellow: left acetabular; Green: Left femora. Please click here to view a larger version of this figure.

Figure 3: Qin's partitioning method of acetabular defects. The acetabulum is divided into three defective sectors (cranial roof, anterior column, and posterior column). The sectors are subdivided into an inner layer and an outer layer. Please click here to view a larger version of this figure.

Figure 4: Procedure of revision hip arthroplasty planning. The complete procedure of reconstruction, evaluation, and planning for acetabular bone defects. Please click here to view a larger version of this figure.

Figure 5: Reconstruction results of the patients' acetabular. The figure presents the reconstruction outcomes for the four patients in conjunction with the corresponding database cases and their postoperative results. Please click here to view a larger version of this figure.

Figure 6: Example of case matching. (A) preoperative image of case two. (B) Reconstruction of acetabular bone defects in case 2. (C) Postoperative image of case two. (D) Preoperative image of matching expert case. (E) Reconstruction of acetabular bone defects in matching expert case. (F) postoperative image of matching expert case. Please click here to view a larger version of this figure.
| Case | Gender | Age | Diagnosis | Paparosky classification | Operative time (min) | Intraoperative hemorrhage (mL) |
| 1 | Man | 45 | aseptic prosthesis loosening after hip arthroplasty | IIA | 112 | 560 |
| 2 | Woman | 67 | IIC | 135 | 690 | |
| 3 | Man | 56 | IIIB | 146 | 1020 | |
| 4 | Man | 42 | IIB | 106 | 420 | |
| 5 | Man | 43 | IIC | 117 | 470 |
Table 1: Case summary and comparison.
Discussion
Due to significant anatomical damage, the intricate soft tissue condition after hip arthroplasty, and the presence of severe metal artifacts often associated with metal implants, it is frequently necessary for experienced medical professionals to utilize 3D reconstruction to comprehensively analyze imaging results and clinical manifestations in order to evaluate specific bone defects in patients and subsequently plan suitable acetabular prostheses9,10. However, even when a patient model is reconstructed, preoperative planning still heavily relies on the expertise of clinicians, particularly when dealing with patients who have severe acetabular defects. Consequently, young doctors face considerable challenges when treating such patients. In order to more accurately assess the extent of acetabular bone defects and leverage previous experience in complex hip joint preoperative planning as a reference for doctors, this study used an expert case database that encompasses nearly all clinical types of hip joint defects while categorizing patients based on certain criteria. By utilizing evaluations of acetabular bone defects from this database, doctors can select appropriate acetabular prostheses and surgical protocols to ensure post-surgical stability and functional recovery of the hip joint.
Although primary hip arthroplasty is a well-established procedure11, the evaluation of acetabular bone defects plays a critical role in ensuring the success and stability of revision hip arthroplasty. Imaging techniques such as X-rays, magnetic resonance imaging (MRI), and CT are commonly employed for assessing acetabular bone defects. These techniques offer detailed information on the structure of the acetabulum, including osseous condition, defect size, and location. Moreover, certain medical image analysis software can be utilized to calculate acetabulum thickness and visualize defects through heat maps12,13,14. However, the presence of metal prosthesis artifacts in preoperative images can affect the accuracy of acetabular segmentation. In this study, third-party software algorithms were utilized to remove artefacts prior to their importation into the system for subsequent operations. The refinement of de-artefacting steps is a subject to be explored in future studies. The network has been trained with genuine artifact images forming the training set and post-processed images devoid of artifacts forming the label set for network training. This approach has yielded satisfactory results in the removal of metal artifacts. Subsequently, a U-Net neural network was employed to automatically segment and reconstruct the original images in three dimensions. Leveraging distinct density values between hip bones and other tissues, this study achieved an impressive segmentation accuracy rate of 95% for the hip joint. The application of deep learning technology significantly reduces model reconstruction time and aids surgical planning while enhancing clinical efficiency. Consequently, it holds substantial practicality and clinical value.
A comprehensive grasp of the morphology and extent of acetabular bone defects, coupled with the development of an appropriate reconstruction plan, is pivotal to the success of hip revision surgery15. Due to the principle of differential calculation, the shape and size of the acetabulum were different for each patient. Accordingly, in cases where the patient presents with a unilateral defect, this study employed mirror processing in accordance with the acetabulum on the healthy side. Thereafter, the mirrored acetabulum model was utilized as the reconstruction model, and rigid registration was performed with the defective acetabulum. Finally, the difference between the reconstructed complete acetabulum and the original defect model was calculated to obtain the amount of bone defects. In order to calculate the extent of bone defects in this study, the acetabular partitioning method proposed by Qin7 was employed to determine the degree of bone defects in each partition. This was then correlated with the cases in the expert database. If the patient has bilateral defects, the reconstruction method is to use a statistical shape model through a large number of complete and healthy acetabulum data in advance, based on PCA principal component analysis statistical calculation, to obtain a set of average models for the calculation of subsequent defects.
Accurate preoperative planning can decrease operative time, reduce intraoperative blood loss, and improve surgical outcomes16. The application of 3D preoperative planning in primary THA has been demonstrated to yield more precise predictions of the acetabular cup and femoral stem dimensions, as well as prosthesis implantation position, in comparison to conventional 2D planning. This advancement significantly contributes to the success of THA surgery17,18. With the development of AI technology, AI-based THA 3D planning has demonstrated enhanced accuracy and efficiency19. Nevertheless, the potential of 3D preoperative planning and the significant clinical applications of AI technology in revision hip arthroplasty have yet to be fully realized. In this study, 3D preoperative planning and AI technology were applied to the clinical revision of hip arthroplasty. Although the application of cases was limited (only 5 cases), and it was not yet possible to assess the accuracy of the prosthesis matching size, the automatic matching of similar cases could provide the surgeon with suggestions for surgical plans. Meanwhile, patients who underwent revision surgery based on the suggested plan demonstrated satisfactory functional recovery. Furthermore, in previous studies, the mean length of revision surgery was 200-300 min, with a mean intraoperative blood loss of 800-2000 mL20,21,22. The mean duration of surgery in this study cohort of five patients was 123.2 min, with intraoperative hemorrhage amounting to 672 mL. The utilization of our novel approach to revision hip arthroplasty has been demonstrated to reduce operative time and intraoperative hemorrhage.
The utilization of an expert case database for the reconstruction of acetabular bone defects and preoperative planning in revision hip arthroplasty has demonstrated significant advantages. Leveraging previous experiences in revision hip arthroplasty, particularly for inexperienced medical professionals, can provide valuable insights and references to enhance the accuracy of preoperative planning. When facing intricate revision surgeries, adopting similar surgical plans from expert cases allows doctors to make necessary adjustments or even reuse them based on patient conditions, thereby reducing preoperative planning time and improving clinical efficiency. Simultaneously, patients can gain prior knowledge about postoperative outcomes through the expert case database. However, limitations still exist in accessing the expert database due to restricted retrieval capabilities and limited follow-up periods for patients, further long-term follow-ups are required to evaluate treatment efficacy. Furthermore, the planning of our revision hip arthroplasty does not include the lateral femoral. Therefore, in instances where femoral lateral revision presents challenges, the overall surgical time may not be shortened. To gain insight into the evolution of surgical time at each stage, a follow-up study will record the overall time of surgery in sections. This will enable statistical analysis and comparison of changes in surgical time across different stages.
Conclusion
The preoperative planning method, which incorporates acetabular bone defect reconstruction and retrieval from an expert case database, presents a novel approach to surgical planning for medical professionals. Leveraging the expertise stored in the case database facilitates expedited and precise execution of complex hip surgeries.
Disclosures
Author Xiaolu Xi, Ke Yuan and Qiang Xie are employed by Wuhan United Imaging Surgical Co., Ltd. The remaining authors declare that they have no competing interests.
Acknowledgements
The AI preoperative planning system in this work was supported by Wuhan United Imaging Surgical Co., Ltd.
Materials
| Name | Company | Catalog Number | Comments |
| PyCharm | JetBrains | 243.21565.199 | The Python IDE for data science and web development |
References
- Sadoghi, P., et al. Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty. 28 (8), 1329-1332 (2013).
- Laughlin, M. S., et al. Mortality after revision total hip arthroplasty. J Arthroplasty. 36 (7), 2353-2358 (2021).
- Bozic, K. J., et al. Comparative epidemiology of revision arthroplasty: Failed THA poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res. 473 (6), 2131-2138 (2015).
- Mahomed, N. N., et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 85 (1), 27-32 (2003).
- Ko, S., et al. Artificial intelligence in orthopedics: three strategies for deep learning with orthopedic specific imaging. Knee Surg Sports Traumatol Arthrosc. 30 (3), 758-761 (2022).
- Velasquez Garcia, A., et al. Artificial intelligence-based three-dimensional templating for total joint arthroplasty planning: a scoping review. Int Orthop. 48 (4), 997-1010 (2024).
- Wang, J., et al. Statistical shape models quantify acetabular defects in hip revision surgery: implications for classification and surgical planning. Arch Orthop Trauma Surg. 145 (1), 45 (2024).
- Telleria, J. J., Gee, A. O. Classifications in brief: Paprosky classification of acetabular bone loss. Clin Orthop Relat Res. 471 (11), 3725-3730 (2013).
- Zhang, J. W., et al. Comparison of 3D printing rapid prototyping technology with traditional radiographs in evaluating acetabular defects in revision hip arthroplasty: A prospective and consecutive study. Orthop Surg. 13 (6), 1773-1780 (2021).
- Li, Q., et al. Three-dimensional technology assisted trabecular metal cup and augments positioning in revision total hip arthroplasty with complex acetabular defects. J Orthop Surg Res. 14 (1), 431 (2019).
- Matar, H. E., Platt, S. R., Board, T. N., Porter, M. L. Overview of randomized controlled trials in primary total hip arthroplasty (34,020 Patients): What have we learnt. J Am Acad Orthop Surg Glob Res Rev. 4 (8), e20.00120 (2020).
- D'Apolito, R., Zagra, L. Uncemented cups and impaction bone grafting for acetabular bone loss in revision hip arthroplasty: A review of rationale, indications, and outcomes. Materials. 15 (10), 3728 (2022).
- Mancino, F., et al. Reconstruction options and outcomes for acetabular bone loss in revision hip arthroplasty. Orthop Rev. 12 (Suppl 1), 8655 (2020).
- Ying, J., et al. Treatment of acetabular bone defect in revision of total hip arthroplasty using 3D printed tantalum acetabular augment. Orthop Surg. 15 (5), 1264-1271 (2023).
- Shen, J., et al. Study on the causes of revision and prosthesis selection after total hip replacement for Crowe Type IV hip dysplasia. Chinese J Reparative Reconstructive Surg. 34 (05), 557-562 (2020).
- Yang, W., et al. Clinical application of artificial intelligence-assisted three-dimensional planning in direct anterior approach hip arthroplasty. Int Orthop. 48 (3), 773-783 (2024).
- Crutcher, J. P., Hameed, D., Dubin, J., Mont, M. A., Mont, M. Comparison of three-versus two-dimensional pre-operative planning for total hip arthroplasty. J Orthop. 47, 100-105 (2023).
- Chen, X., et al. Validation of CT-Based three-dimensional preoperative planning in comparison with acetate templating for primary total hip arthroplasty. Orthop Surg. 14 (6), 1152-1160 (2022).
- Huo, J., et al. Value of 3D preoperative planning for primary total hip arthroplasty based on artificial intelligence technology. J Orthop Surg Res. 16 (1), 156 (2021).
- Saito, K., et al. Intraoperative hemorrhage in revision total hip arthroplasty: a retrospective single-center study. J Anesth. 33 (3), 399-407 (2019).
- Pflüger, M. J., Frömel, D. E., Meurer, A. Total hip arthroplasty revision surgery: Impact of morbidity on perioperative outcomes. J Arthroplasty. 36 (2), 676-681 (2021).
- Bautista, M., et al. Thromboprophylaxis for hip revision arthroplasty: Can we use the recommendations for primary hip surgery? A cohort study. Clin Appl Thromb Hemost. 25, 1076029618820167 (2019).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved