Method Article
Transcorporal Artificial Urinary Sphincter Cuff Placement in a Case Requiring Revision for Urethral Atrophy
In This Article
Summary
Here we describe the application of transcorporal artificial urethral sphincter (AUS) placement in a case requiring revision of an artificial urinary sphincter for urethral atrophy.
Abstract
Artificial urethral sphincter (AUS) implantation is the definitive management of male stress urinary incontinence (SUI). Under the long-term pressure of the cuff, recurrence of incontinence caused by urethral atrophy can always be observed in patients. In this situation, distal cuff locations are needed, and new cuff sites should be sought in patients who need to undergo AUS reimplantations. Meanwhile, the circumference of the more distal urethra is often too small to fit with a 4.0 cm cuff. This means that the bulk of the urethra should be added not only for a sufficient urethral circumference but also for better protection. Here, we report a case that required AUS reimplantation because of urethral atrophy. This 73-year-old man had undergone AUS implantation 7 years ago and developed incontinence in the past 3 months. Physical examination and ultrasonography determined that the device still worked, and no obstruction or injury was observed through cystoscopy. Surgery for revision of the AUS was needed. In this operation, a new cuff was implanted transcorporally, which was 2 to 3 cm distal to the original cuff site. During a 6 month short-term follow-up, no stress incontinence, urethral injury, or dysuria was observed. The transcorporal technique offers significant advantages in patients with urethral atrophy: corporal tunica albuginea is added to the urethra, allowing a suitable cuff size and lower risk of erosion. It is worth recommending in the reoperation of AUS implantation.
Introduction
In the past three decades, artificial urethral sphincter (AUS) implantation has been the definitive management for male stress urinary incontinence, and most patients can benefit from this technique1. However, some patients may develop recurrences of slight incontinence with time, which is usually caused by urethral atrophy beneath the cuff. Meanwhile, patients who undergo urethral surgeries or radical prostatectomy may also develop stress urinary incontinence accompanying urethral atrophy. In these situations, the original cuff sites are not suitable for simply reimplanting a downsizing cuff, and a new cuff site or a second tandem cuff implantation is a better choice2,3. Compared with the implantation of a second cuff, placing a cuff at a new site seems a safer alternative. Generally, the new cuff is advised to be placed at a new site proximal or distal to the previous site4,5. In some special cases that have undergone end-to-end urethral anastomosis, the proximal site is unfeasible. Thus, the more distal urethra is usually selected. However, the small circumference of the more distal urethra often leads to an inadequate urethral coaptation with the 4 cm cuff, and the dorsal side of the urethra is also a common location of urethral erosion. This means that the bulk of the urethra should be added not only for a sufficient urethral circumference but also for better protection.
To resolve these problems, Guralnick reported a transcorporal cuff implantation technique in 2002 and obtained satisfactory results6. This technique not only increases the urethral circumference but also protects the urethra. In this paper, we describe this technique with our small modification, which was performed on a patient requiring AUS revision for urethral atrophy.
Protocol
The study was approved by the local Medical Ethics Committee of Shanghai Ninth People's Hospital in China. All of the studies were conducted in accordance with the World Medical Association Declaration of Helsinki. Written consent was obtained from the patient.
1. Preparations
- Monitor the patient for the development of urethral injury or stricture under the long-term pressure of the original cuff through a flexible cystoscopy.
- Ensure that the device was determined to still function and that the recurrence of incontinence was caused by urethral atrophy according to physical examination, ultrasonography, and magnetic resonance imaging (MRI).
- Ask the patient to shower and wash the skin of the surgical region every day.
- Ensure that the urinary infection has been controlled before the operation twice through urine culture.
- Ensure that the preoperative anesthesia risk assessment of the patient has been performed by an anesthesiologist.
- Administer an intravenous antibiotic preoperatively 30 min before the operation using 1.5 g of cefuroxime sodium with 100 mL of 0.9% sodium chloride solution.
- To reduce the risk of infection, prepare 0.5 g of vancomycin in 500 mL of 0.9% sodium chloride solution for intraoperative antibiotic solution immersion and irrigation of AUS components.
- After general anesthesia, place the patient in the lithotomy position for good exposure to the surgical area.
- For adequate disinfection of the surgical area, continuously disinfect the skin of the surgical area with iodophor for 15 min.
2. Procedures
- Removing the original AUS
- Make a 5 cm longitudinal incision on the middle line of the lower scrotum where the original cuff was placed, and expose the urethra and the components of the AUS.
- Cut one side of the cuff using scissors and then remove it from the urethra.
NOTE: The wound should be irrigated by 0.5 g of vancomycin in 500 mL of 0.9% sodium chloride solution.
- Reimplantation of the new AUS
- Select the new cuff site 2-3 cm distal to the original cuff site (Figure 1A). Subsequently, extend the incision distally, and expose the urethra and adjacent corporal bodies.
- Dissect the urethra containing the bulbospongiosus muscle from the tunica albuginea of the corpora cavernosa and measure the urethral circumference. The circumference was much smaller than 4 cm.
- Make 2 cm longitudinal incisions on the tunica albuginea of the corpora cavernosa bilaterally 2 mm lateral to the urethra and deepen only until corporal spongy tissue is visible (Figure 1B, C).
- Create a tunnel between the two corporotomies by blunt dissection, and measure the urethral circumference containing the tunica albuginea and bulbospongiosus muscle (Figure 1D).
- Remove the pump and water reservoir along the connecting tubes.
- Prepare the AUS components and make sure to expel air from the components thoroughly. Then, immerse all the components in the solution mixed by 0.5 g of vancomycin and 500 mL of 0.9% sodium chloride.
- Position a new 4 cm cuff containing the tunica albuginea, bulbospongiosus muscle, and urethra.
- Place the pump in the original scrotal disc space.
- Open the external inguinal ring and create a retropubic prevesical space by blunt dissection using the index finger. Then, place the water reservoir into this space using sponge forceps.
- After filling with 22 mL of 0.9% sodium chloride solution, connect the whole device in the usual manner.
- Squeeze and release the pump bulb two to three times quickly and determine that all fluid has been removed from the cuff. After system testing, keep pressing the the metal buttom on the pump for several seconds to deactivate the device. Finally, place a 10 Fr catheter.
- Layer off each incision with 3-0 absorbable polyglactin sutures and dress the operative region with appropriate pressure.
NOTE: The tubes should be protected well by the mosquito hemostat jaws with the silicone tubing provided in the Accessory Kit. When using the hemostats, clamp jaws together only to the first click to prevent excessive pressure on tubes. When these tubes are being connected, each end should be washed with 0.9% sodium chloride solution to avoid antibiotic mixing.
3. Postoperative care
- Postoperatively, administer an intravenous antibiotic to prevent infection: Mix 1.5 g of cefuroxime sodium in 100 mL of 0.9% sodium chloride solution, q 12 h, for 3 days and mix 1.0 g of ornidazole in 100 mL of 0.9% sodium chloride solution, q 24 h, for 3 days.
- Recommend a cold compress with ice bag to relieve the swelling pain of the wound in the first 6 h.
- Remove the catheter 24 h postoperatively.
- Activate the device at 6 weeks postoperatively. Meanwhile, do not allow the patient to use pads and recommend temporarily using a penis clamp for urinary continence.
NOTE: Catheterization should be performed again with a 10 Fr catheter once the urine retention is observed after catheter removal.
Results
The operation went smoothly, and the patient recovered quickly. No complications, such as infection, edema, hematoma, or uroschesis, were observed. The device was activated at postoperative week 6 in the outpatient service. During a 6 month short-term follow-up, the patient could operate the AUS device expertly without stress incontinence, and no urethral injury or dysuresia occurred (Table 1).
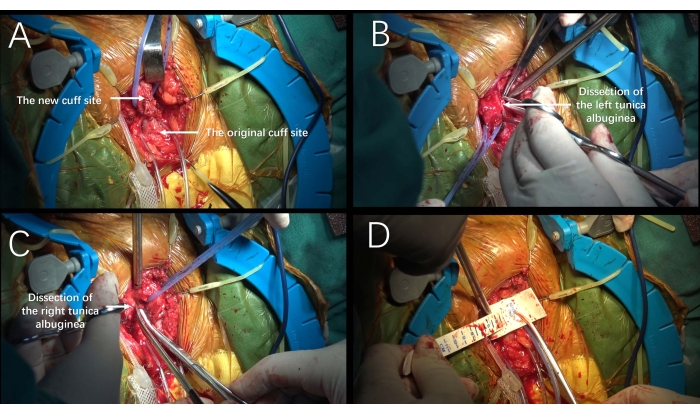
Figure 1: Transcorporal approach. (A) The new cuff site was selected to be 2-3 cm distal to the original cuff site. (B-C) Longitudinal incisions 2 cm long were made into the tunica albuginea of the corpora cavernosa bilaterally 1- 2 mm lateral to the urethra. (D) Measurement of the urethral circumference containing the tunica albuginea and bulbospongiosus muscle. Please click here to view a larger version of this figure.
| Age (year) | 73 |
| Etiology | postprostatectomy incontinence |
| Follow-up (month) | 6 |
| Prior treatment | AUS implantation 7 years ago |
| Size of cuff | 4 |
| Urethral circumference (cm) | 3.5 |
| Activation of the device | postoperative week 6 |
| Result | complete dry |
| Complication | None |
Table 1: Pre and postoperative patient details.
Discussion
Artificial urinary sphincter implantation is the gold standard for the treatment of SUI, and high success and satisfactory rates have been reported7. Yafi and colleagues reported a 79% success rate and a90% satisfaction rate in their systematic review8. In the long-term follow-up, complications such as nonfunctioning devices, subcuff atrophy, erosion, and infection were reported to be common. For patients who develop subcuff atrophy or erosion, removing the original cuff and reimplanting a new cuff is better than placing a second tandem cuff and may avoid further damage to the urethra. This was also the reason why we did not implant a tandem cuff in this patient. Although Saffarian9 reported an improved continence rate after downsizing procedures, the 3.5 cm cuff may still be a potential factor leading to new atrophy. In contrast, Bugeja10 and his colleagues did not agree with the theory of subcuff atrophy. Their study indicated that the recurrent incontinence was because of material failure of the pressure-regulating balloon, which led to a loss of its ability to generate the designated pressure. Under lower pressure, urethral atrophy would not occur. Thus, they suggested a simple reimplantation with a new, same-sized cuff in the same position10. In this patient, a typical 'hour-glass' shape of the corpus spongiosum was revealed after cuff removal. Considering that the underlying urethral wall was much thinner than other parts and did not recover to its original thickness, we chose relocation of the new cuff.
Compared with the original and proximal sites, the distal urethra can both reduce the risk of urethral injury and the difficulty of urethral dissection. However, the circumference of the distal urethra is sometimes too small to achieve adequate coaptation with the 4 cm cuff. Thus, more tissues are needed to increase the circumference of the urethra, which is why we preserved bulbospongiosus muscle in this case. When the urethra and its surrounding bulbospongiosus muscle were not fit with the smallest cuff, corporal tunica albuginea was added. Sometimes, the distal urethra was not covered by the bulbospongiosus muscle, and a wider and thicker corporal tunica albuginea could be used.
In theory, this technique is suitable not only for patients who need AUS reimplantation because of urethral atrophy or erosion, but also for patients with SUI and small urethral circumferences, such as patients who have undergone urethroplasty or radical prostatectomy. With the wide mastery of radical prostatectomy in China, the incidence of SUI will increase expectedly. Then, this technique will be used more widely when patients have postoperative urethral atrophy caused by the operative neurovascular injury.
Notably, the transcorporal approach carries the risk of causing erectile dysfunction11. Although most patients were more concerned about incontinence than erectile dysfunction, detailed and, frank consultations should be conducted before surgery. Compared with Guralnick's approach, the advantage of our modification is a reduced depth of dissection and less damage to erectile tissues, which may reduce the potential incidence of erectile dysfunction. For patients who suffer from male stress incontinence and erectile dysfunction, simultaneous implantation of an artificial urethral sphincter and a penile prosthesis is a good option. Meanwhile, this technique should be carefully performed on patients who have undergone urethral anastomosis before, especially those whose urethra may have been embedded into the two corpus cavernosa for tension-free anastomosis. For these patients, a sufficient depth of dissection of the corpus cavernosa is recommended for the protection of the urethra.
In conclusion, the transcorporal technique provides a good solution for patients with male stress urinary incontinence and accompanying urethral atrophy or erosion caused by any reason.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This study was sponsored by Cross Disciplinary Research Fund of Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine (JYJC202103).
Materials
| Name | Company | Catalog Number | Comments |
| 3-0 absorbable polyglatin suture | ETHICON | VCP311H | suture |
| 5-0 absorbable polyglatin suture | ETHICON | VC433H | suture |
| Artificial urinary sphincter | Boston Scientific | AUS800 | A device for managetment of male stress urinary incontinence |
| Cefuroxime sodium | Youcare Parmaceutical Group | H20063758 | Antibiotics |
| Flexible cystoscopy | KARL STORZ | C-VIEW® | cystoscopy |
| Foley catheter | HAIYAN KANGYUAN MEDICAL INSTRUMENT CO., LTD. | 20192140294 | Catheter |
| Ornidazole | Pudepharma | H20040104 | Antibiotics |
| Vancomycin | Eli Lilly Japan K.K,Seishin Laboratories | JX20130179 | Antibiotics |
References
- Boswell, T. C., Elliott, D. S., Rangel, L. J., Linder, B. J. Long-term device survival and quality of life outcomes following artificial urinary sphincter placement. Translational Andrology and Urology. 9 (1), 56-61 (2020).
- Motley, R. C., Barrett, D. M. Artificial urinary sphincter cuff erosion. Experience with reimplantation in 38 patients. Urology. 35 (3), 215-218 (1990).
- Brito, C. G., Mulcahy, J. J., Mitchell, M. E., Adams, M. C. Use of a double cuff AMS800 urinary sphincter for severe stress incontinence. The Journal of Urology. 149 (2), 283-285 (1993).
- Kowalczyk, J. J., Nelson, R., Mulcahy, J. J. Successful reinsertion of the artificial urinary sphincter after removal for erosion or infection. Urology. 48 (6), 906-908 (1996).
- Frank, I., Elliott, D. S., Barrett, D. M. Success of de novo reimplantation of the artificial genitourinary sphincter. The Journal of Urology. 163 (6), 1702-1703 (2000).
- Guralnick, M. L., Miller, E., Toh, K. L., Webster, G. D. Transcorporal artificial urinary sphincter cuff placement in cases requiring revision for erosion and urethral atrophy. The Journal of Urology. 167 (5), 2075-2078 (2002).
- Radadia, K. D., et al. Management of postradical prostatectomy urinary incontinence: A review. Urology. 113, 13-19 (2002).
- Yafi, F. A., Powers, M. K., Zurawin, J., Hellstrom, W. J. Contemporary review of artificial urinary sphincters for male stress urinary incontinence. Sexual Medicine Reviews. 4 (2), 157-166 (2016).
- Saffarian, A., Walsh, K., Walsh, I., Stone, A. R. Urethral atrophy after artificial urinary sphincter placement: is cuff downsizing effective. The Journal of Urology. 169 (2), 567-569 (2003).
- Bugeja, S., Ivaz, S. L., Frost, A., Andrich, D. E., Mundy, A. R. Urethral atrophy after implantation of an artificial urinary sphincter: fact or fiction. BJU International. 117 (4), 69-76 (2016).
- Wiedemann, L., et al. Transcorporal artificial urinary sphincter implantation as a salvage surgical procedure for challenging cases of male stress urinary incontinence: surgical technique and functional outcomes in a contemporary series. BJU International. 112 (8), 1163-1168 (2013).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved