Method Article
3D Printing Model of a Patient's Specific Lumbar Vertebra
In This Article
Summary
This study aims to create a 3D-printed model of a patient-specific lumbar vertebra, which contains both the vertebra and spinal nerve models fused from high-resolution computed tomography (HRCT) and MRI-Dixon data.
Abstract
Selective dorsal rhizotomy (SDR) is a difficult, risky, and sophisticated operation, in which a laminectomy should not only expose an adequate surgical field of view but also protect the patient's spinal nerves from injury. Digital models play an important role in the pre-and intra-operation of SDR, because they can not only make doctors more familiar with the anatomical structure of the surgical site, but also provide precise surgical navigation coordinates for the manipulator. This study aims to create a 3D digital model of a patient-specific lumbar vertebra that can be used for planning, surgical navigation, and training of the SDR operation. The 3D printing model is also manufactured for more effective work during these processes.
Traditional orthopedic digital models rely almost entirely on computed tomography (CT) data, which is less sensitive to soft tissues. Fusion of the bone structure from CT and the neural structure from magnetic resonance imaging (MRI) is the key element for the model reconstruction in this study. The patient's specific 3D digital model is reconstructed for the real appearance of the surgical area and shows the accurate measurement of inter-structural distances and regional segmentation, which can effectively help in the preoperative planning and training of SDR. The transparent bone structure material of the 3D-printed model allows surgeons to clearly distinguish the relative relationship between the spinal nerve and the vertebral plate of the operated segment, enhancing their anatomical understanding and spatial sense of the structure. The advantages of the individualized 3D digital model and its accurate relationship between spinal nerve and bone structures make this method a good choice for preoperative planning of SDR surgery.
Introduction
Spastic cerebral palsy affects over half of all children with cerebral palsy1, leading to tendon contractures, abnormal skeletal development, and decreased mobility, greatly impacting the quality of life of affected children2. As the main surgical method for the treatment of spastic cerebral palsy, selective dorsal rhizotomy (SDR) has been fully validated and recommended by many countries3,4. However, the intricate and high-risk nature of SDR surgery, including the precise cutting of the lamina, positioning and dissociation of nerve roots, and severing of nerve fibers, presents a significant challenge for young doctors who are just beginning to engage with SDR in clinical practice; further, the learning curve of SDR is very steep.
In traditional orthopedic surgery, surgeons must mentally integrate all preoperative two-dimensional (2D) images and create a 3D surgical plan5. This approach is particularly difficult for preoperative planning involving complex anatomical structures and surgical manipulations, such as SDR. With advances in medical imaging and computer technology, 2D axial images, such as computed tomography (CT) and magnetic resonance imaging (MRI) can be processed to create 3D virtual models with patient-specific anatomy6. With improved visualization, surgeons can analyze this processed information to make more detailed diagnoses, planning, and surgical interventions tailored to the patient's condition. In recent years, the application of multimodal image fusion technology in orthopedics has gradually attracted attention7. This technology could fuse CT and MRI images, greatly improving the accuracy of the digital3D analog model. However, the application of this technique in preoperative models of SDR has not been researched yet.
Accurate positioning of the lamina and spinal nerve and precise cutting during SDR surgery are crucial for successful outcomes. Typically, these tasks rely on experts' experience and are confirmed repeatedly by a C-arm during the operation, resulting in a complex and time-consuming surgical process. The 3D digital model serves as the foundation for future SDR surgical navigation and can also be utilized for preoperative planning of laminectomy procedures. This model fuses the bone structure from CT and the spinal nerve structure from MRI, and assigns different colors to the lumbar vertebra sections marked for cutting according to the surgical plan. Such holographic 3D printing models for SDR not only facilitate preoperative planning and simulation, but also output accurate 3D navigation coordinates to the intraoperative robotic arm for precise cutting.
Protocol
All data come from the clinical patient, whose SDR operation was carried out at BJ Dongzhimen Hospital. The protocol follows the guidelines of and was approved by the Dongzhimen Hospital research ethics committee.
NOTE: The whole map of the model reconstruction protocol is shown in Figure 1. The high-resolution computed tomography (HRCT) data and Dixon data are raw materials for modeling; then, the 3D model creation consists of image registration and fusion. The final 3D digital model is printed by PolyJet technology which is a high-precision 3D printing process that produces smooth and accurate parts using a wide range of materials. In order to describe the spatial relationship between the vertebra and spinal nerve exactly, HRCT data and Dixon image series are used. The Dixon scanning can identify water and fat separation images, in which the Dixon water phase image series can be used to extract the structure of the spinal nerves, and the Dixon-in phase image series can be used to check the registration of the bone structure.

Figure 1: The whole map of the protocol. The research methodology of this study involves the fusion of CT and magnetic resonance Dixon sequences. Specifically, the CT vertebrae structure is registered with the identical vertebrae structure contained in the Dixon-in sequence, followed by fusion with the Dixon-w sequence for the spinal nerve. Please click here to view a larger version of this figure.
1. Data collection and preparation
- High-resolution CT for vertebrae
NOTE: The parameter difference is not sensitive to the research method.- Set the data resources from the CT machine station.
NOTE: Here, the SIEMENS-CTAWP73396 CT machine is used. - Open the Syngo CT 2012B software to receive data from the scanning protocol SpineRoutine_1. Select the Pixel Size and Slice Thickness (ST) of the dataset to adapt to the size of the vertebrae intended to be represented in the 3D digital model.
- Use an ST of 1 mm with a matrix size of 512 pixels x 512 pixels, in which the pixel spacing is 0.3320 mm. The actual size of the 3D volume achieved is 512 x 512 x 204 voxels.
- Set the data resources from the CT machine station.
- Dixon sequence for spinal nerve
NOTE: A 1.5 T MRI machine is used in this study.- Set the Dixon image Resolution as 290 pixels x 320 pixels, Pixel Spacing as 0.9375 mm, and Slice Thickness as 3 mm to obtain accurate data.
- Set the Repetition Time as 5,160 ms and the Echo Time as 94 ms.
- Ensure every scanned layer consists of four-phase images, which are Dixon-in, Dixon-opp, Dixon-F, and Dixon-w.
- Prepare data-storing files for model reconstruction.
NOTE: A well-defined data-storing structure is more convenient for follow-up work.- Make a project folder to contain all the data belonging to the patient.
- Prepare different file paths for HRCT and MRI-Dixon data by making different folders for the digital imaging and communications in medicine (DICOM) data.
- Make a separate folder under the project for all analysis results.
2. The 3D digital vertebrae model
NOTE: All subprocess functions come from software tools, whose property belongs to Beijing Intelligent Entropy Science & Technology Co Ltd.
- Call the Dicom2Mat subprocess in the MATLAB workplace to obtain the 3D volume from the DICOM files stored in the HRCT data folder.
- After undergoing the Dicom2Mat subprocess, view each slice within the 3D volume through the graphical user interface (GUI), as depicted in Figure 2.
- Then, visualize the intensity distribution of the vertebrae HRCT data by the hist function (Figure 3).
- Call the NoiseClean subprocess to delete signal noise formed by the device under the HRCT data file paths.
- Use the Vertebrae function subprocess under the same path to gain the vertebrae model, which is also a 3D volume but only with the bone structure (Figure 4). The high-pass filter parameters, the intensity ranging from 190 to 1,656.
3. The 3D digital spinal nerve model
NOTE: Dixon-in contains bone structure, while Dixon-w describes neural structure.
- Use the Dicom2Mat subprocess in both paths of the Dixon-in and Dixon-w sequences and get their 3D volume.
- Furthermore, visualize each individual slice that constitutes a 3D volume using the GUI presented in Figure 5. Access this visualization once the Dicom2Mat subprocess has been completed.
- Use the Spinal_Nerve function to reconstruct the spinal nerve model with high-pass filter parameters, the intensity ranging from 180 to 643. Because the signals of the nerve in the Dixon-w sequence are very high, extract the spinal nerve 3D volume by filtering out points with low intensity.
- When the Spinal_Nerve subprocess is finished, check the model generated in the GUI shown in Figure 6.
4. Registration and fusion
NOTE: The key insight is that bone architecture is present in both HRCT and Dixon-in imaging sequence.
- Copy the three 3D volumes obtained so far to the file path of the project made in step 3.1. The models from HRCT and Dixon-in include the same vertebrae structure, and the models from Dixon-in and Dixon-w have the same coordinates.
- Then, put the three models' filenames into the vertebra_fusion subprocess as an input to generate the fusion model. This can be visualized in Figure 7.
- The fusion is usually well done. If fine-tuning is necessary from the doctor's perspective, add coordinate parameters in all directions to the same function to correct the fusion model. If slight errors are observed in fusion from a clinical perspective, use the vertebra_fusion function to fine-tune the fusion coordinates. This process involves parameter adjustments to the six dimensions of coordinate direction (XYZ coordinates and their rotation).
- Make a separate folder in the project directory for outputting the result of the fusion model.
5. Digital model files for 3D printing
NOTE: A fully-developed 3D printing apparatus is utilized for the manufacturing of the aforementioned digital model, with the implementation of Delaunay triangulations. Here, the Stratasys J55 Prime 3D printer was used.
- Export the fusion models to be used for 3D printing in the DICOM format sequences under the file path of the fusion directory. Utilize the Mat2Dicom algorithm to execute the export operation by inputting the fusion model.
- Open the DICOM file sequence exported previously using Materialise Mimics V20. To perform the export operation, navigate to the Export menu under the File tab and select the VRML format. The file path for the export can be freely customized according to the user's requirements.
- As transparent colorful 3D printing is a professional service, compress and pack the VRML files and send them to the service provider. The 3D printing result is shown in Figure 8.
Results
Based on lumbar CT/MRI image fusion data in children with cerebal palsy, we created a representative model of the lumbar spine combined with spinal nerves. High-pass filtering was used to extract the high signal in the CT value range of 190-1,656 from HRCT, so as to achieve the reconstruction of the bone structure of the lumbar spine in the operation area. Spinal nerve structures were reconstructed by the high-pass filtering of Dixon-w sequences in MRI. The digital model and point cloud data coordinates of the lumbar vertebral structure and spinal nerve fusion were obtained through rigid registration, and the file was saved in stereolithography (STL) format for data measurement and further printing processing. The STL digital model files are converted to VRML format for transfer to the Stratasys J55 Prime 3D printer. To actively demonstrate the anatomy of the surgical site during SDR surgery, we printed the bones in transparent resin and printed the other parts in different colors. The 3D-printed model can then reveal the spatial relationship of key surgical sites in SDR for surgeons and patients during preoperative planning and training.
The obtained personalized 3D lumbar spine model provides the possibility for preoperative planning and training of SDR. Different color dyes are used to stain and distinguish the structures, such as bones and nerves. As shown in Figure 8, the spinal nerve structure is dyed yellow, and the lamina of L4 and L5 segments in the corresponding operation area are distinguished by red and blue staining, respectively. The bone structure is printed using a transparent resin material, which has a good perspective, allowing doctors to observe the nerve structure under the lamina through the bone structure. The personalized, customized model truly restores the corresponding relationship between the lumbar bone structure in the operation area and the spinal nerve anatomy, allowing doctors to better define the appropriate cutting direction and range before the operation.

Figure 2: The GUI of slices in the volume from HRCT data. Through the GUI shown in the figure, surgeons can view the spine structure contained in all the CT data. Please click here to view a larger version of this figure.
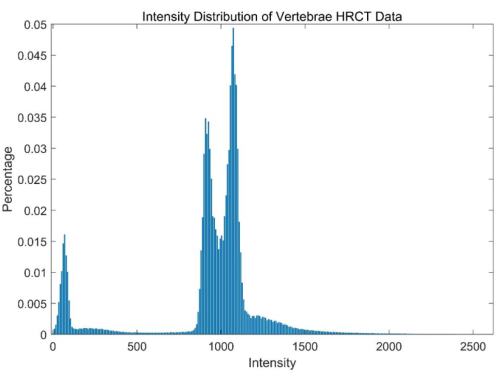
Figure 3: The intensity distribution of vertebrae HRCT data. This quantitative information is helpful in determining the filtering range of vertebrae structure. Please click here to view a larger version of this figure.

Figure 4: The GUI of the 3D volume of the vertebrae. The figure shows the three views of the vertebrae and the 3D volume at the same time. Through this GUI, surgeons can observe the vertebrae of patients from any desired perspective. Please click here to view a larger version of this figure.
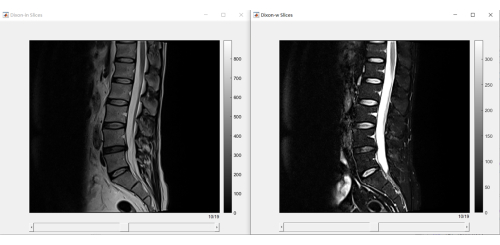
Figure 5: The GUI of slices in the volume from Dixon-in and Dixon-w. Dixon imaging can be quickly browsed, and the images of patients' vertebrae and spinal nerves can be checked. Please click here to view a larger version of this figure.
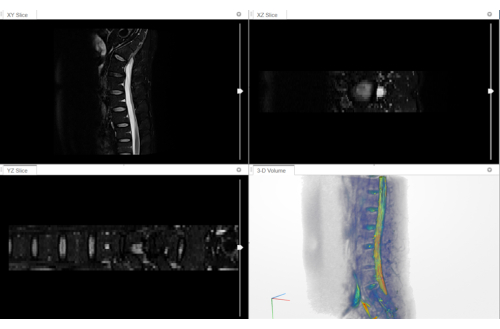
Figure 6: The GUI of the 3D volume of the spinal nerve. The 3D reconstruction of the Dixon-w sequence of the patient for observing the 3D structure of the patient's spinal nerve. Please click here to view a larger version of this figure.
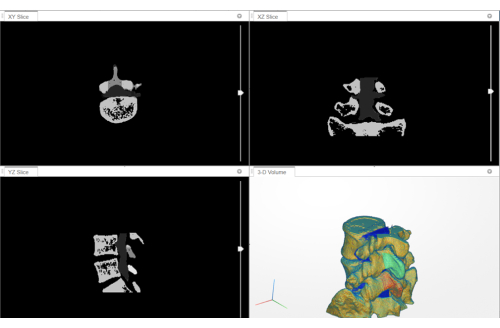
Figure 7: The GUI of the fusion model (3D digital volume). The 3D volume contains both the vertebral structure from the CT data and the 3D structure of the spinal nerve from magnetic resonance. Please click here to view a larger version of this figure.

Figure 8: The 3D printing model for SDR planning and training. The transparent colorful 3D printing model shows the anatomical structure of the area where SDR surgery needs to be performed on the patient. Please click here to view a larger version of this figure.
Discussion
This study provides a workflow for establishing a preoperative 3D printing model of the lumbar spine in patients with cerebral palsy, with the aim of facilitating preoperative planning for SDR surgery and enhancing anatomical training based on the patient's specific model. The study aims to establish a highly reliable 3D-printed model that accurately demonstrates the patient's lumbar vertebral and nerve structures. By measuring the position of the lamina and spinal nerve in the model before surgery, precise planning of the lamina cutting can be achieved, leading to the optimization of surgical procedures and the acquisition of mastery in SDR surgical technology.
The primary key step investigated in this study was the fusion of CT and Dixon sequences. The fusion relied on the presence of the same bone structures in both the CT data and Dixon-in sequences, as well as the fact that the Dixon-in and Dixon-w data were in the same coordinate system. This allowed for the final fusion of the spinal nerves and vertebral bone structures. The second key step was the use of color-transparent printing technology to manufacture the 3D digital model. This printing technology was capable of highlighting the patient's anatomical structures, the precise location of laminectomy, and the relative position of the intervertebral foramina and nerve roots.
In recent decades, many surgical teams have developed innovative techniques for SDR8,9, with a primary focus on minimizing spinal damage during the procedure. This arises from the well-established efficacy of long-segment surgery in spasm relief, alongside concerns regarding the impact of extensive laminectomy on spinal stability10. Successful SDR surgery requires a critical laminectomy, which necessitates both sufficient incisions of the lamina to enable further neurosurgical manipulation and the preservation of enough lamina to avoid spinal destabilization. Precise laminar cutting without damage or negative effects during the operation requires a comprehensive understanding of the position, size, and section of the cutting. Currently, preoperative SDR evaluation primarily relies on CT/MRI imaging and clinical experience, which may not fully meet the requirements of precise cutting operations. In recent years, the application of multimodal image fusion in spine surgery has shown great potential value, while relevant research is still rare. Thus, this study aimed to fuse preoperative lumbar spine CT and MRI to reconstruct a 3D digital model accurately representing both the bone structure and spinal nerves. The reconstructed 3D digital model was further 3D-printed and could be utilized for effective doctor-patient communication and preoperative planning. The model's precise positioning of the lumbar nerve root outlet enabled a better understanding of the spatial relationship between the vertebrae and the nerve root, facilitating an efficient operation for both surgeons and surgical robots.
Furthermore, children with cerebral palsy exhibit distinct spinal and skeletal development, characterized by a hypoplastic trabecular bone microstructure, thin cortex, and low bone strength11. These unique anatomical features and complex manipulations render SDR surgery challenging to master. Therefore, we employed 3D printing technology to fabricate anatomically precise lumbar vertebrae models of real patients, offering an objective reference for surgical learning. This technique is ideal for less experienced surgeons and may potentially reduce the learning time12. In addition, individually tailored models offer the added benefit of fully restoring the patient's unique structure, providing valuable insight for those with complex anatomical variations13,14.
High-quality initial image acquisition is essential for successful 3D printing15. In this study, a realistic and accurate 3D printing model was obtained through the registration of HRCT and MRI data. Transparent printing of the bone structure and dyeing of the planning range of the laminae further enhanced the model's intuitive representation of surgical anatomy. Traditionally, surgeons acquire surgical skills primarily in the operating room, which increases the risks of surgery when younger surgeons first attempt to acquire such skills in practice12. With objective physical 3D printing models, senior surgeons can more easily communicate their surgical experience to younger physicians. Additionally, the 3D printing models can uniquely provide individuals with simulated surgical training based on a real patient structural reconstruction, potentially accelerating the physician learning process for SDR while improving the safety of medical procedures. Overall, this approach holds great promise in enhancing surgical training and improving patient outcomes.
At present, the application of 3D printing in orthopedics remains in the exploration stage, and existing biomaterial technology falls short of accurately representing the materials of different human tissues and simulating the biomechanics of joints5. During a laminectomy, the elastic models of various tissues are complex and subject to disruption by disc motion and respiratory motion16,17. Therefore, this study cannot fully replicate the real condition of the intraoperative patient during the cutting operation, which requires further research on the 3D printing model in biomechanics and materials science. Furthermore, the fusion procedure employed in this study may be further improved if a coordinate registration method can be devised during the medical imaging procedures for both the CT and MRI equipment, potentially enhancing accuracy.
If a coordinate registration method can be designed during medical imaging procedures for both CT and MRI equipment, the fusion procedure of this study may further improve the accuracy. The expected gradual improvement in this part of the research is ongoing. Currently, the model cannot fully display information on spinal nerve fiber bundles. In the upcoming scientific work, diffusion tensor imaging will be further used to track spinal nerve fiber bundles and fused to obtain a more detailed 3D digital model for SDR.
In conclusion, the 3D printing model for SDR in this study not only provides detailed and accurate data for preoperative planning, but also provides a core medium for SDR training. The model successfully fuses bone structure from CT with soft tissue structure from MRI. The success of this image group fusion paradigm takes advantage of the respective advantages of two important medical image sources to form a complement. This research paradigm will also play an equally important role in other fields of medical imaging diagnosis, treatment, and prognosis evaluation.
Disclosures
The digital models in this study are reconstructed by co-author Fangliang Xing.
Acknowledgements
This publication was supported by the Beijing Municipal Natural Science Foundation (L192059).
Materials
| Name | Company | Catalog Number | Comments |
| J55 Prime 3D-Printer | Stratasys | J55 Prime | Manufacturing the model |
| MATLAB | MathWorks | 2022B | Computing and visualization |
| Mimics | Materialise | Mimics Research V20 | Model format transformation |
| Tools for volum fusion | Intelligent Entropy | VolumeFusion V1.0 | Beijing Intelligent Entropy Science & Technology Co Ltd. Modeling for CT/MRI fusion |
References
- Rosenbaum, P., et al. A report: the definition and classification of cerebral palsy April 2006. Developmental Medicine and Child Neurology. Supplement. 109, 8-14 (2007).
- Krigger, K. W. Cerebral palsy: an overview. American Family Physician. 73 (1), 91-100 (2006).
- Davidson, B., Fehlings, D., Milo-Manson, G., Ibrahim, G. M. Improving access to selective dorsal rhizotomy for children with cerebral palsy. Canadian Medical Association Journal. 191 (44), E1205-E1206 (2019).
- Buizer, A. I. Selective dorsal rhizotomy in children with cerebral palsy. The Lancet. Child & Adolescent Health. 3 (7), 438-439 (2019).
- Wong, K. C. 3D-printed patient-specific applications in orthopedics. Orthopedic Research and Reviews. 8, 57-66 (2016).
- Wong, K. C., Kumta, S. M., Geel, N. V., Demol, J. One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Computer Aided Surgery. 20 (1), 14-23 (2015).
- Zhu, R., Li, X., Zhang, X., Ma, M. MRI and CT medical image fusion based on synchronized-anisotropic diffusion model. IEEE Access. 8, 91336-91350 (2020).
- Park, T. S., Gaffney, P. E., Kaufman, B. A., Molleston, M. C. Selective lumbosacral dorsal rhizotomy immediately caudal to the conus medullaris for cerebral palsy spasticity. Neurosurgery. 33 (5), 929-934 (1993).
- Sindou, M., Georgoulis, G. Keyhole interlaminar dorsal rhizotomy for spastic diplegia in cerebral palsy. Acta Neurochirurgica. 157 (7), 1187-1196 (2015).
- Peacock, W. J., Staudt, L. A. Selective posterior rhizotomy: evolution of theory and practice. Pediatric Neurosurgery. 17 (3), 128-134 (1991).
- Vitrikas, K., Dalton, H., Breish, D. Cerebral palsy: an overview. American Family Physician. 101 (4), 213-220 (2020).
- Niikura, T., et al. Tactile surgical navigation system for complex acetabular fracture surgery. Orthopedics. 37 (4), 237-242 (2014).
- Lepisto, J., Armand, M., Armiger, R. S. Periacetabular osteotomy in adult hip dysplasia-developing a computer aided real-time biome-chanical guiding system (BGS). Finnish Journal of Orthopaedics and Traumatology. 31 (2), 186-190 (2008).
- Armiger, R. S., Armand, M., Tallroth, K., Lepisto, J., Mears, S. C. Three-dimensional mechanical evaluation of joint contact pressure in 12 periacetabular osteotomy patients with 10-year follow-up. Acta Orthopaedica. 80 (2), 155-161 (2009).
- Rengier, F., et al. 3D printing based on imaging data: review of medical applications. International Journal of Computer Assisted Radiology and Surgery. 5 (4), 335-341 (2010).
- Jiang, Z., et al. Model-based compensation of moving tissue for state recognition in robotic-assisted pedicle drilling. IEEE Transactions on Medical Robotics and Bionics. 2 (3), 463-473 (2020).
- Setton, L. A., Chen, J. Mechanobiology of the intervertebral disc and relevance to disc degeneration. The Journal of Bone and Joint Surgery. American. 88, 52-57 (2006).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved