Method Article
Arthroscopic Repair of Medial Meniscus Posterior Root Tear with Adjustable Titanium Plate Fixation
* Wspomniani autorzy wnieśli do projektu równy wkład.
W tym Artykule
Podsumowanie
This article describes a surgical approach to repairing a medial meniscus posterior root tear (MMPRT) using a single-suture, double-loop, adjustable titanium plate internal fixation under arthroscopy.
Streszczenie
Medial meniscus injury is one of the most prevalent knee disorders, with posterior root tears occurring in approximately 10% to 21% of affected individuals. A posterior root tear disrupts the meniscus's continuous annular structure, compromising its ability to absorb pressure and protect the knee's articular cartilage. If left untreated, this can result in increased stress on the cartilage, leading to conditions such as varus deformity and accelerated joint degeneration. Partial removal (resection) of the medial meniscus further exacerbates these issues, often leading to quicker joint deterioration. Repairing medial meniscus posterior root tears (MMPRTs) plays a crucial role in restoring the meniscus's structural integrity and improving knee biomechanics. Studies have shown that compared to partial medial meniscectomy or conservative treatments, repairing MMPRTs enhances clinical outcomes and significantly delays the onset of arthritis. This article details a surgical procedure that uses a single-suture, double-loop, adjustable titanium plate fixation technique under arthroscopy for effective MMPRT repair.
Wprowadzenie
The meniscus consists of fibrocartilage and cannot repair itself after an injury, except for partial injuries to the margins, which can heal on their own. A normal meniscus increases the depth of the tibial condyle and cushions the medial and external femoral condyles, enhancing joint stability and absorbing shock. After a meniscus injury, joint space pain can occur, and in severe cases, it may be accompanied by symptoms such as joint locking. Posterior root tears occur in 10% to 21% of patients with medial meniscus injuries1,2,3,4. The attachment point of the medial meniscus posterior root (MMPR) to the posterior region of the tibial intercondylar spine firmly anchors the meniscus to the tibial plateau, and its integrity plays an important role in maintaining the position and function of the normal meniscus5. A tear at the MMPR is an avulsion of the posterior tibial attachment of the medial meniscus or a radial tear within 1 cm of the bony attachment of the MMPR6, first reported by Pagnani et al. in 19917. MMPRTs are mostly degenerative injuries of the meniscus and commonly affect middle-aged and elderly patients8. Risk factors for posterior root tears of the medial meniscus include age, female sex, obesity (high Body Mass Index), and knee varus1,9. Activities such as descending stairs and jogging place twice the amount of stress on the MMPR compared to ordinary walking9, meaning poor exercise habits can also increase the likelihood of posterior root tears.
The MMPR is anchored to the tibial plateau to maintain the annular structure of the meniscus, which helps redistribute axial pressure across the joint, reducing the load on the cartilage10,11,12,13. When the knee joint experiences axial pressure, the meniscus is compressed and dislocated outward, which prevents it from adequately alleviating the axial stress on the knee joint, thereby accelerating joint degeneration and the development of osteoarthritis10,11,14,15,16. MMPRTs carry a higher risk of articular cartilage damage compared to other types of degenerative meniscal injuries3,17. Additionally, the larger the tear gap caused by the posterior root tear, the more severe the impact on the cartilage17,18,19.
Treatment options for MMPRTs include posterior root repair, partial meniscectomy, and conservative treatment. It has been reported that patients who undergo posterior meniscus root repair experience a significant delay in the progression of arthritis compared to those treated with partial meniscectomy or conservative methods, as shown by K-L grading on anterior lateral knee radiographs pre-operation versus post-operation20. After a tear at the MMPR, there is no functional or biomechanical difference from partial meniscectomy, as the absence of a ring-like stabilizing structure reduces the dispersion of axial forces21. MMPRT repair improves clinical outcomes, with 87% of patients unresponsive to conservative treatment and 31% requiring knee arthroplasty within 5 years11,22,23. A follow-up of patients with MMPRTs receiving conservative treatment for at least 10 years reported failure in approximately 95% of cases, with around 64% undergoing knee arthroplasty24. Numerous studies have shown that repair surgery is superior to partial meniscectomy and conservative treatment in terms of efficacy and function for patients with MMPRT, significantly delaying the progression of osteoarthritis4,24,25,26. This article describes a surgical approach to repairing MMPRT using a single-suture, double-loop, adjustable titanium plate internal fixation under arthroscopy.
Protokół
This protocol was approved by the Ethics Committee of Hebei Medical University Third Hospital (K2023-086-1). The patient and their family agreed upon the surgical plan, and an informed consent form was signed. The inclusion criteria for the surgical approach were patients with knee MMPRT and Kellgren-Lawrence grade 0-III osteoarthritis without severe varus deformity. Exclusion criteria were: patients with knee MMPRT with injury to the medial meniscus body or anterior horn, injury to the anterior or posterior cruciate ligament, injury to the medial collateral ligament, or Kellgren-Lawrence grade IV osteoarthritis27. The details of the reagents and equipment used in this study are listed in the Table of Materials.
1. Pre-operative preparation
- Abstain from eating and drinking for 6 h before the operation. Choose neuraxial anesthesia or general anesthesia based on the anesthesiologist's pre-operative assessment of the patient's physical condition (following institutional guidelines).
- Position the patient in the supine position on the operating bed.
- Apply a tourniquet to the proximal one-third of the affected limb. Disinfect the affected limb with 2% iodine, covering all areas distal to the tourniquet. Wait 2-3 min for the iodine to dry. Perform deiodination twice with 75% medical alcohol.
- Place the operating sheet, elevate the affected limb, and use a pneumatic tourniquet to expel venous blood from the distal to the proximal end of the limb. Inflate the tourniquet to SBP + 100 mmHg and set the timer for 90 min.
2. Checking the lesions
- Use an 11 G sharp knife to make an incision 5 mm from the joint capsule at the upper edge of the tibial plateau, extending 1 cm on both sides of the parapatellar joint. Establish the anteromedial and anterolateral approaches to the knee joint, respectively28.
NOTE: This procedure is performed with the knee flexed at 90 degrees. - Insert the arthroscope through the anterolateral approach to the knee. Insert a probe through the anteromedial approach. Examine the knee to locate the MMPRT (Figure 1A).
NOTE: Apply valgus and external rotation stress to the knee joint to fully expose the posterior medial compartment.
3. Creating a single-suture single-loop knot
- Use an epidural needle to puncture the skin on the posteromedial aspect of the knee joint. Insert the needle into the joint at the upper edge of the MMPR.
- Insert the needle 3 mm outward from the center of the MMPRT and thread a 2-0 PDS suture along the core of the epidural needle (Figure 1B).
- Establish an anteromedial approach to the knee.
NOTE: The incision should be positioned at the midline of the patellar ligament, 1 cm below the inferior pole of the patella. - Place wire grabbers through the anteromedial approach and pull the PDS suture out below the meniscus.
- Fix one end of the PDS suture at the anteromedial approach and use a thread grabber to pull the PDS suture above the meniscus.
- Tie the PDS suture with a No. 2 non-absorbable suture outside the anteromedial approach. Pull the PDS suture through the meniscus until it emerges outside the joint, then untie the PDS knot.
NOTE: The reflexed end of the non-absorbable suture should be drawn out from the anteromedial incision, with the two free ends remaining outside the incision. - Pull the free ends of the non-absorbable suture to draw the body loop of the suture into the joint. Place a thread grabber through the anteromedial approach inside the joint. Capture a free end of the non-absorbable suture through the single loop and pull it out through the anteromedial approach.
- Use a thread grabber to hold the free ends of the non-absorbable suture and pull them outside the anteromedial approach to form a single-suture, single-loop knot (Figure 1C).
4. Creating a single-suture double-loop knot
- Repeat steps 3.1-3.2, placing a PDS suture 3 mm outside the first puncture point of the MMPR.
- Repeat steps 3.4-3.7, and use a thread grabber through the anteromedial approach. Pull the other free end of the non-absorbable suture through the second loop to form a single-suture double-loop knot (Figure 1D).
5. Creating a single-suture double-loop adjustable titanium plate complex
- Make a 1 cm incision at Gerdy's tubercle29, extending to the bone cortex to serve as the external entrance of the tunnel.
- Locate the inner entrance of the tunnel 5 mm inward from the tear of the posterior root.
- Insert the guide needle from the outside to the inside, ensuring the tip of the needle pierces through the inner entrance of the tunnel.
NOTE: Use the anterior cruciate ligament (ACL) reconstruction locator to accurately locate the inner and outer openings of the tunnel. - Use a 5 mm drill, following the guide needle from the outside to the inside, to create the bone tunnel.
NOTE: Use two retractors to pull back the skin and subcutaneous soft tissues to expose the outer opening of the tunnel; otherwise, it may be difficult to locate the outer opening. - Place the PDS thread loop in the anteromedial approach to the inner entrance of the tunnel. Insert a thread grabber from the outer entrance of the tunnel to the inner entrance. Capture the PDS thread loop and a free end of the non-absorbable suture.
NOTE: The two free ends of the PDS thread should be outside the anteromedial approach, and the PDS thread loop and a free end of the non-absorbable suture should be pulled out to the outer entrance of the bone tunnel. - Pass the free end of the non-absorbable suture through the adjustable titanium plate loop and then through the PDS thread loop. Pull the free ends of the PDS thread and the non-absorbable suture outside the anteromedial approach.
- Tighten the free end of the non-absorbable suture and locate the adjustable loop in the single-suture double-loop configuration (Figure 1E).
- Use a knotter to tie the non-absorbable sutures, forming the single-suture double-loop adjustable titanium plate complex.
NOTE: The first knot must be tied tightly, and the first knot should remain secure when tying the second knot.
6. Fixing the MMPR
- Pull the adjustable loop to draw the single-suture double-loop adjustable titanium plate complex, pulling the torn MMPR into the inner entrance of the tunnel.
- Gradually tighten the titanium plate towards the outer entrance of the tunnel until it adheres to the bone cortex.
NOTE: When tightening the adjustable loop, proceed slowly because it is unidirectional and cannot be loosened once tightened. - Use a probe to examine the medial meniscus and ensure the MMPR is firmly fixed in the tibial plateau footprint (Figure 1F).
- Cut the non-absorbable sutures at the base of the ties using a thread trimmer.
7. Closing the incisions
- Suture the incisions using intermittent No. 4 silk sutures.
- Cover the wound with sterile dressings.
8. Post-operative rehabilitation
- On the first day after surgery, focus on strengthening the quadriceps muscles.
- On the second day after surgery, begin knee flexion and extension exercises.
- On the second day after surgery, ask the patient to start walking without weight-bearing, using a brace for protection.
- From 1-6 weeks after surgery, ask the patient to walk with partial weight-bearing while using a brace for protection.
- On the 12th day after surgery, remove the sutures.
- From 6-12 weeks after surgery, ask the patient to walk with full weight-bearing, under the protection of a brace, and gradually resume normal movement.
- At 3 months post-surgery, remove the brace and gradually return to normal activities.
Wyniki
A total of 35 patients participated in the study, consisting of 25 females and 10 males. The average age was 53.54 years ± 11.03 years, ranging from 28 years to 78 years. Among the patients, 15 had an MMPR tear accompanied by degeneration of the medial femoral condyle or tibial plateau articular cartilage, classified as grade 2 or lower (Figure 2). The other 20 patients had an MMPR tear with grade 3 degeneration of the medial femoral condyle or tibial plateau articular cartilage (Table 1). No patients with grade 4 degeneration in these areas were included, and none had significant varus deformity.
Patients were assessed preoperatively and 1 year postoperatively using the Lysholm score30 and the IKDC score31 (Table 2). The pre-operative Lysholm score was 33.09 ± 13.24, with a 95% confidence interval (CI) of [28.54, 37.63]. The Lysholm score at 1 year postoperatively was 90.6 ± 6.95, with a 95% CI of [88.21, 92.99]. The pre-operative IKDC score was 40.46 ± 10.91, with a 95% CI of [36.71, 44.21]. The IKDC score at 1 year postoperatively was 84.5 ± 16.04, with a 95% CI of [78.99, 90.01]. The scores 1 year after surgery were significantly higher than those before surgery (P < 0.05) (Figure 3).
Anterolateral X-rays of the knee before surgery showed no significant progression of osteoarthritis compared to 1 year after surgery. MRI at the 1-year follow-up for all patients revealed that the MMPR was firmly fixed, with no significant outward protrusion of the meniscus (Figure 4).

Figure 1: Key steps of the surgical procedure. (A) Exploration reveals a tear at the MMPR. (B) The epidural needle is used to suture the MMPR, crossing the PDS suture. (C) A single-suture single-loop knot is formed by threading a free end of the non-absorbable suture through the single loop. (D) A single-suture double-loop knot is formed by passing the other free end of the non-absorbable suture through the second loop. (E) An adjustable loop is introduced from the external opening of the articular tibial tunnel to the inner opening, creating a single-suture double-loop adjustable titanium plate complex. (F) Exploration shows the posterior root is close to the footprint area of the medial tibial plateau. This figure is adapted from Chen et al.32. Please click here to view a larger version of this figure.

Figure 2: MRI images of a typical MMPR tear. (A) Sagittal MRI image showing a tear at the MMPR. (B) Coronal MRI image showing a tear at the MMPR. This figure is adapted from Chen et al.32. Please click here to view a larger version of this figure.
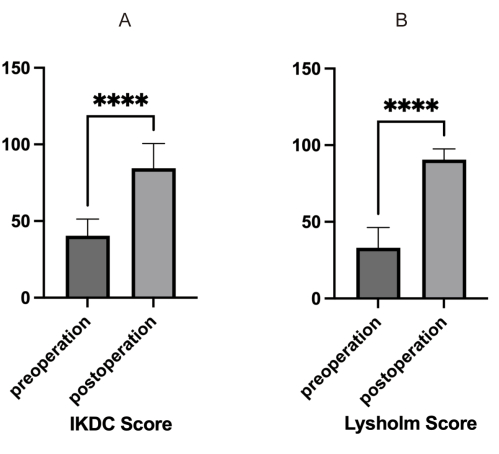
Figure 3: Pre-operative and post-operative knee scores. (A) Histogram comparing pre-operative and post-operative IKDC scores. A statistically significant difference is observed (P < 0.05). (B) Histogram comparing pre-operative and post-operative Lysholm scores. A statistically significant difference is observed (P < 0.05). Please click here to view a larger version of this figure.

Figure 4: MRI images of a typical MMPR tear repair. (A) Sagittal MRI image showing the repair of the MMPR tear. (B) Coronal MRI image showing the repair of the MMPR tear. This figure is adapted from Chen et al.32. Please click here to view a larger version of this figure.
| Total number of patients | Males | Females | Average age (years) | The oldest age (years) | The youngest age (years) | Combined with 2nd grade degeneration of the medial cartilage of the knee joint and below | Combined with 3rd grade degeneration of medial cartilage of the knee |
| 35 | 10 | 25 | 53.54 ± 11.03 | 78 | 28 | 15 | 20 |
Table 1: Basic information and statistics of the patients. This table includes patient demographics, age distribution, and medial cartilage degeneration grade.
| Lysholm scores | Lysholm score 95%CI | IKDC scores | IKDC scores 95%CI | |
| Pre-operation | 33.09 ± 13.24 | [28.54,37.63] | 40.46 ± 10.91 | [36.71,44.21] |
| Post-operation | 90.6 ± 6.95 | [88.21,92.99] | 84.5 ± 16.04 | [78.99,90.01] |
Table 2: Pre-operative vs. post-operative scores of the patients. This table compares pre-operative and post-operative IKDC and Lysholm scores, showing significant improvement in scores post-operation (P < 0.05).
Dyskusje
Treatment options for MMPRTs include posterior root repair, partial meniscectomy, and conservative treatment. Many studies have shown that partial medial meniscectomy and conservative treatment are ineffective in preventing or delaying osteoarthritis23,26,33. MMPRT repair, however, can effectively alleviate pain symptoms and prevent or delay the progression of osteoarthritis. For patients with MMPRTs accompanied by severe medial cartilage degeneration and lower limb varus alignment, MMPRT repair alone may be insufficient34,35,36,37, and high tibial osteotomy is recommended. For younger patients with MMPRTs who require active rehabilitation and long-term efficacy, MMPRT repair surgery is advised.
Common MMPRT repair techniques include transosseous tunnel MMPRT repair and rivet suture repair38. Transosseous tunnel MMPRT repair involves using a locator to establish a bone tunnel from the proximal tibia to the medial tibial root. An angle suture hook or suture gun is then used to suture the torn MMPR, with the suture line pulled through the bone tunnel and fixed to the external opening of the cortical bone at the proximal tibia. This method aims to anatomically reconstruct the MMPR in the tibial plateau footprint area, forming a meniscus-cancellous bone healing structure.
In 1995, Shino et al.39 first reported two cases of lateral meniscus root tears repaired through tibial tunneling. In 2006, Raustol et al.40 applied a similar approach to repair MMPRTs, incorporating an added posteromedial compartment approach. Kim et al.41 used two sutures to repair the torn meniscus posterior root, pulling the sutures out of the proximal tibial cortex through a 5 mm single tunnel, and fixing them with screws at the outer opening of the tibial tunnel. Ahn et al.42 criticized the single-tunnel technique for its limited contact area and uneven force distribution, proposing a modification that involved using double sutures drawn through two tibial tunnels and knotted and fixed on a bone bridge between the tunnels at the proximal tibia. LaPrade et al.43 found no significant biomechanical difference between single and double tunneling techniques in a comparison of ten pairs of cadaveric specimens. Transtibial tunneling technology effectively repairs the torn MMPR, provides firm fixation, and promotes meniscus bone healing through the growth factors and bone marrow mesenchymal stem cells produced by drilling the bone.
In 2007, Engelsohn et al.44 introduced a surgical method involving the use of an absorbable rivet to secure the MMPR at its tibial attachment point with the aid of a posteromedial approach. This method repairs the torn MMPR using the tail suture of the anchor and fixes it with a knot. Subsequent studies have reported good efficacy with this anchor suture repair technique45,46,47. However, rivet suture repair requires an additional posteromedial approach, which poses risks of injury to the posterior vascular and nerve structures. The narrow posteromedial operating space makes the insertion of the rivet and posterior root suturing technically challenging, increasing the risk of cartilage injury. Additionally, there is a risk that the rivet may become dislodged, potentially leading to surgical failure. The anchor suture, which creates a large knot, may also cause entrapment within the joint, potentially affecting the post-operative outcome.
MMPRT repair through a bone tunnel may present risks such as suture cutting through the meniscus root, wear of the suture material, and failure of the meniscus-cancellous bone to integrate into a single structure, which can lead to surgical failure. Additionally, the established bone tunnel may interfere with cruciate ligament reconstruction. To address these issues, the single-thread, double-loop suture technique is employed to reduce the cutting force of the suture on the MMPR. The double loops create a stress surface that increases the force area, thereby dispersing the cutting force of the suture. By using adjustable loops to control fixation tension, the tension can be gradually tightened, ensuring firm fixation of the MMPR in the footprint area.
To minimize the risk of suture wear, the MMPR is pulled into the tunnel of the internal tibial orifice, with sutures inserted as deeply as possible into the tunnel. This approach enhances the integration of the cancellous bone in the tunnel with the posterior root of the meniscus, increasing the contact area and likelihood of healing. For suturing the MMPR, an epidural needle is used to puncture the posteromedial aspect of the knee without an incision, thereby reducing the risk of vascular and nerve injury. Since the suture hook does not need to be operated in the narrow posteromedial compartment, the single suture and double loops are prepared by simply guiding the lead directly into the target position of the meniscus using the epidural needle, which minimizes cartilage damage. To prevent interference with the bone tract of cruciate ligament reconstruction, the outer tibial tunnel opening is positioned at the tibial Gerdy's tubercle.
The 35 patients treated with single-suture double-loop adjustable titanium plate internal fixation for MMPRTs under arthroscopy achieved significant improvements in pre-operative and post-operative Lysholm and IKDC scores30,31.
However, this approach has its limitations. The manual knot used to secure the single-suture double-loop adjustable titanium plate may loosen or detach, potentially leading to insufficient tension at the posterior root and resulting in surgical failure. Additionally, the adjustable loop of the titanium plate provides unidirectional and irreversible tension. Once the tension is set, it cannot be adjusted if it becomes too tight, which could affect the fixation and overall surgical outcome. Furthermore, the follow-up period for patients has been relatively short, and the long-term efficacy of this technique requires further validation.
In conclusion, the surgical approach for MMPRT repair using single-suture double-loop adjustable titanium plate internal fixation under arthroscopy is a safe, effective, and relatively simple procedure.
Ujawnienia
The authors declare that there are no conflicts of interest in this study.
Podziękowania
This research was supported by the Youth Science and Technology Project of the Department of Health of Hebei Province (20201046) and the Hebei Province key research and development plan project.
Materiały
| Name | Company | Catalog Number | Comments |
| Adjustable loop titanium plate | star | F06003978 | Φ60 |
| Aimer,tip,drctr ACL guide | smith&nephew | 7205519 | |
| Angled bullet | smith&nephew | 7207282 | |
| Arthroscopic sheath | smith&nephew | 72200829 | 6 mm |
| Arthroscopy | smith&nephew | 72202087 | 30° 4 mm |
| Beam guide | smith&nephew | 72204925 | 5 mm x 3.6 m |
| Beam guide-arthroscopy end connector | smith&nephew | 2143 | |
| Beam guide-panel connector | smith&nephew | 2147 | |
| Blood-repellent belt | selani | tpe15100 | 15 cm x1 m |
| Blunt puncture cone | smith&nephew | 4356 | 4 mm |
| Camera | smith&nephew | 72200561 | NTSC/PAL |
| Canulated drill | smith&nephew | 13498 | 5 mm |
| Coupler | smith&nephew | 72200315 | |
| Drill guide wire | smith&nephew | 14396 | 2.4 mm |
| DYONICS POWER II | smith&nephew | 72200873 | 100-24VAC, 50/60Hz |
| DYONICS POWERMAX ELITE | smith&nephew | 72200616 | |
| Elite Knot Manipulating Full Loop | smith&nephew | 72201213 | |
| Elite Premium Bankart Rasp | smith&nephew | 72201660 | |
| Elite premium suture loop vertical grasper,blue handle | smith&nephew | 7209494 | |
| Elite sliding suture cutter | smith&nephew | 7209492 | |
| Endoscopic camera system | smith&nephew | 72201919 | 560P NTSC/PAL |
| Handle | smith&nephew | 7205517 | |
| HD monitor | smith&nephew | LB500031 | 27 inch |
| Hook probe | smith&nephew | 3312 | |
| Incisor plus platinum shaver | smith&nephew | 72202531 | 4.5 mm |
| Lumbar needle AN-E/S II | tuoren | AN-E/S  | 1.6 x 80 mm |
| Micropunch,teardrop,left | smith&nephew | 7207602 | |
| Micropunch,teardrop,right | smith&nephew | 7207601 | |
| Micropunch,teardrop,straight | smith&nephew | 7207600 | |
| PDS II | Johnson&Johnson | D6451 | 2-0 |
| Pitbull Jr. Grasper | smith&nephew | 14845 | |
| Shoulder Elavator | smith&nephew | 13949 |
Odniesienia
- Abdrabou, A. Medial meniscus posterior root tear. Radiopaedia.org. , (2016).
- Choi, C. J., Choi, Y. J., Song, I. B., Choi, C. H. Characteristics of radial tears in the posterior horn of the medial meniscus compared to horizontal tears. Clin Orthop Surg. 3 (2), 128 (2011).
- Guermazi, A., et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: The multicenter osteoarthritis study. Radiology. 268 (3), 814-821 (2013).
- Krych, A. J., et al. Nonoperative management of degenerative medial meniscus posterior root tears: Poor outcomes at a minimum 10-year follow-up. Am J Sports Med. 51 (10), 2603-2607 (2023).
- DePhillipo, N. N., et al. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: Defining meniscal ramp lesions. Am J Sports Med. 47 (2), 372-378 (2019).
- Koenig, J. H., Ranawat, A. S., Umans, H. R., DiFelice, G. S. Meniscal root tears: Diagnosis and treatment. Arthroscopy. 25 (9), 1025-1032 (2009).
- Pagnani, M. J., Cooper, D. E., Warren, R. F. Extrusion of the medial meniscus. Arthroscopy. 7 (3), 297-300 (1991).
- Pache, S., et al. Meniscal root tears: Current concepts review. Arch Bone Jt Surg. 6 (4), 250-259 (2018).
- Yokoe, T., et al. Shear stress in the medial meniscus posterior root during daily activities. Knee. 43, 176-183 (2023).
- Allaire, R., Muriuki, M., Gilbertson, L., Harner, C. D. Biomechanical consequences of a tear of the posterior root of the medial meniscus: Similar to total meniscectomy. J Bone Joint Surg Am. 90 (9), 1922-1931 (2008).
- Jackson, G. R., et al. A systematic review of adverse events and complications after isolated posterior medial meniscus root repairs. Am J Sports Med. 52 (4), 1109-1115 (2023).
- Mohamadi, A., et al. Evolution of knowledge on meniscal biomechanics: A 40 year perspective. BMC Musculoskelet Disord. 22 (1), 625 (2021).
- Padalecki, J. R., et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 42 (3), 699-707 (2014).
- LaPrade, M., et al. Investigating the chronology of meniscus root tears: Do medial meniscus posterior root tears cause extrusion or the other way around. Orthop J Sports Med. 9 (7_suppl 4), (2021).
- LaPrade, R. F., et al. Meniscal root tears: Solving the silent epidemic. J Arthrosc Surg Sports Med. 2, 47-57 (2021).
- Lerer, D. B., Umans, H. R., Hu, M. X., Jones, M. H. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 33 (10), 569-574 (2004).
- Dirim Mete, B., Cilengir, A. H., Gursoy, M., Dag, F., Bulut, T. Meniscal extrusion, cartilage, bone, and ligament lesions associated with medial meniscus posterior root tear gap. Eur J Radiol. 162, 110801 (2023).
- Bin, S. -. I., Jeong, T. -. W., Kim, S. -. J., Lee, D. -. H. A new arthroscopic classification of degenerative medial meniscus root tear that correlates with meniscus extrusion on magnetic resonance imaging. Knee. 23 (2), 246-250 (2016).
- Kim, J. -. Y., et al. A novel arthroscopic classification of degenerative medial meniscus posterior root tears based on the tear gap. Orthop J Sports Med. 7 (3), 232596711982794 (2019).
- Bernard, C. D., et al. Medial meniscus posterior root tear treatment: A matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med. 48 (1), 128-132 (2020).
- Marzo, J. M., Gurske-DePerio, J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 37 (1), 124-129 (2009).
- Chung, K. S., et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: A minimum 5-year follow-up. Arthroscopy. 31 (10), 1941-1950 (2015).
- Krych, A. J., et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 25 (2), 383-389 (2017).
- Faucett, S. C., et al. Meniscus root repair vs. meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: Clinical and economic effectiveness. Am J Sports Med. 47 (3), 762-769 (2019).
- Lee, W. Q., Gan, J. Z. -. W., Lie, D. T. T. Save the meniscus-Clinical outcomes of meniscectomy versus meniscal repair. J Orthop Surg. 27 (2), 230949901984981 (2019).
- Lutz, C., et al. Meniscectomy versus meniscal repair: 10 years radiological and clinical results in vertical lesions in stable knee. Orthop Traumatol Surg Res. 101 (8), S327-S331 (2015).
- Kellgren, J. H., Lawrence, J. S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 16 (4), 494-502 (1957).
- Funk, F. J. A color atlas of arthroscopy. J Sports Med. 1 (1), 24-26 (1972).
- Donegan, D. J., Seigerman, D. A., Yoon, R. S., Liporace, F. A. Gerdy's tubercle: The lighthouse to the knee. J Orthop Trauma. 29 (2), e51-e53 (2015).
- Lysholm, J., Gillquist, J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 10 (3), 150-154 (1982).
- Hefti, E., Müller, W., Jakob, R. P., Stäubli, H. -. U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1 (3-4), 226-234 (1993).
- Chen, J., et al. Arthroscopic linear chain fixation for the treatment of medial meniscus posterior root tear: A case study. Orthop Surg. 16 (3), 775-780 (2024).
- Krych, A. J., et al. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 26 (4), 1117-1122 (2017).
- Ahn, J. H., et al. Comparison between conservative treatment and arthroscopic pull-out repair of the medial meniscus root tear and analysis of prognostic factors for the determination of repair indication. Arch Orthop Trauma Surg. 135 (9), 1265-1276 (2015).
- Chung, K. S., Ha, J. K., Ra, H. J., Kim, J. G. Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy. 32 (7), 1319-1327 (2016).
- Ishikawa, H., et al. Arthroscopic medial meniscus posterior root reconstruction and pull-out repair combined technique for root tear of medial meniscus. Arthrosc Tech. 11 (2), e109-e114 (2022).
- Jiang, E. X., et al. Clinical factors associated with successful meniscal root repairs: A systematic review. Knee. 26 (2), 285-291 (2019).
- Moon, H. -. S., et al. Medial meniscus posterior root tear: How far have we come and what remains. Medicina (Kaunas). 59 (7), 1181 (2023).
- Shino, K., Hamada, M., Mitsuoka, T., Kinoshita, H., Toritsuka, Y. Arthroscopic repair for a flap tear of the posterior horn of the lateral meniscus adjacent to its tibial insertion. Arthroscopy. 11 (4), 495-498 (1995).
- Raustol, O. A., Poelstra, K. A., Chhabra, A., Diduch, D. R. The meniscal ossicle revisited: Etiology and an arthroscopic technique for treatment. Arthroscopy. 22 (6), 687.e1-687.e3 (2006).
- Kim, Y. -. M., et al. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 22 (7), 795.e1-795.e4 (2006).
- Ahn, J. H., et al. Double transosseous pull out suture technique for transection of posterior horn of medial meniscus. Arch Orthop Trauma Surg. 129 (3), 387-392 (2009).
- LaPrade, C. M., LaPrade, M. D., Turnbull, T. L., Wijdicks, C. A., LaPrade, R. F. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 43 (4), 899-904 (2015).
- Engelsohn, E., Umans, H., DiFelice, G. S. Marginal fractures of the medial tibial plateau: Possible association with medial meniscal root tear. Skeletal Radiol. 36 (1), 73-76 (2007).
- Choi, N. -. H., Son, K. -. M., Victoroff, B. N. Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: A technical note. Knee Surg Sports Traumatol Arthrosc. 16 (9), 891-893 (2008).
- Jung, Y. -. H., Choi, N. -. H., Oh, J. -. S., Victoroff, B. N. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 40 (6), 1406-1411 (2012).
- Kim, J. -. H., et al. Arthroscopic suture anchor repair of posterior root attachment injury in medial meniscus: Technical note. Arch Orthop Trauma Surg. 129 (8), 1085-1088 (2009).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone