Method Article
Establishing a Multidisciplinary Cavernous Carotid Injury Simulation to Train Neurosurgical, Otolaryngology, and Anesthesia Residents
W tym Artykule
Podsumowanie
This protocol establishes a multidisciplinary model to train learners on management of cavernous carotid artery injury. Cadaveric heads undergo expanded endonasal approach and injury to the cavernous carotid artery, and perfusion pump simulates blood flow to the injury point. Learners are tasked with medical and surgical management over 3 scenarios.
Streszczenie
Carotid artery injuries are serious complications of endoscopic endonasal surgery. As these occur rarely, simulation training offers an avenue for technique and algorithm development in resident learners. This study develops a realistic cadaveric model for the training of crisis resource management in the setting of cavernous carotid artery injury. An expanded endonasal approach and right cavernous carotid injury is performed on a cadaveric head. The cadaver's right common carotid artery is cannulated and connected to a perfusion pump delivering pressurized simulated blood. A simulation mannequin is incorporated into the model to allow for vital sign feedback. Surgical and anesthesia resident learners are tasked with obtaining vascular control with a muscle patch technique and medical management over the course of 3 clinical scenarios with increasing complexity. Crisis management instructions for an endoscopic endonasal approach to the cavernous carotid artery and blood pressure control were provided to the learners prior to beginning the simulation. An independent reviewer evaluated the learners on communication skills, crisis management algorithms, and implementation of appropriate skill sets. After each scenario, residents were debriefed on how to improve technique based on evaluation scores in areas of situational awareness, decision-making, communications and teamwork, and leadership. After the simulation, learners provided feedback on the simulation and this data was used to improve future simulations. The benefit of this cadaveric model is ease of set-up, cost-effectiveness, and reproducibility.
Wprowadzenie
Internal carotid artery injuries are a serious, albeit rare, complication of endoscopic endonasal approaches that require surgical dissection of tumor or vascular pathology adjacent to the cavernous sinus1. Techniques and algorithms for managing this type of complication can only be obtained through realistic simulation2. Wormald and colleagues have pioneered a training protocol for how to manage carotid injuries using a sheep model simulation3. They used a crush muscle patch with direct pressure over the injury site for hemostasis followed by direct vessel closure. This simulation has successfully improved outcomes in actual practice for multiple surgeons4. While beneficial, it has been shown that a cadaveric model of vascular injury is both more clinically relevant and cost-effective than using sheep and can be used for crisis management training5. Simulation training provides learners from neurosurgery and otolaryngology residencies the opportunity to develop algorithms for managing complications in real-time settings5,6. What is important going forward is establishing a replicable model for broad training across institutions, and multidisciplinary collaboration within simulations.
The purpose of this study is to highlight the steps to produce a realistic cadaveric model for cavernous carotid artery injury and how to set up a multidisciplinary crisis management simulation. This model provides a method for neurosurgery and otolaryngology residents, in collaboration with anesthesia residents, to train on medical management of cavernous carotid injury. The benefits of this model are its reproducibility, cost-effectiveness, and ease of set-up. This study utilizes a cadaveric head model with perfusion pumps, which is more transportable and less-expensive than the whole body perfusion model developed by Pham and colleague7. It can be used innumerable times to train resident learners over the course of several sessions. The benefit of replication is that different clinical scenarios can be devised to train learners on important clinical considerations in a real-time context and to train residents on important steps for crisis management. The cadaveric head model has been combined with a simulated mannequin body to allow representation of clinical vital signs during the scenarios, and facilitate collaboration with anesthesia residents. The following protocol highlights a step-by-step procedure for how to set up the model.
Protokół
Cadaveric heads used in this protocol were acquired from the Oregon Health & Science University Body Donation Program. All methods described have been approved by the Oregon Health & Science University Institutional Review Board (IRB).
1. Head Preparation
- Secure the fresh cadaveric head in the sink with the neck facing upwards.
- Using a 1:100 anti-coagulant citrate dextrose solution, rinse out the jugular veins, vertebral, and carotid arteries bilaterally. Start by inserting a 5mm diameter cannula into the right jugular vein and secure the vessel around the cannula with a 5-inch hemostat clamp. Run the perfusion pump for 15 min. Rotate the tube to the left jugular vein and then carotid arteries and repeat the washout for 15 min at each vessel. Use a 3 mm diameter cannula for the vertebral arteries. The fluid should be clear, not bloody, at the end of the washout.
- Let the heads dry overnight with the face upwards and the neck positioned at a 45° angle with a block positioned beneath it. Store in a cold room at 5 °C.
- The following day, embed the head in 2 L of embalming solution and store it in a bucket with formalin fixative.
Caution: embalming solution and formalin fixative are corrosive. Please wear protective equipment.
2. Tissue Dissection
- Support the head with a block and position it in the neutral orientation avoiding over flexion or extension.
- Use a zero degree endoscope of 4 mm diameter and 18 cm length.
- Lateralize the middle turbinates and perform a bilateral sphenoidotomy. Make the incision at the articulation of the rostrum and vomer.
- Clear the mucoperiosteum with a cottle elevator and remove the rostral bone bilaterally with a rongeur.
- Drill flush to the floor of the sphenoid sinus and laterally to the medial orbital walls bilaterally with a high-speed drill and matchstick type drill head.
3. Preparing Cavernous Carotid Injury
- Visualize the regions of the sella, clival structures, and cavernous carotid arteries. Remove the bone overlying the sella and cavernous carotid artery on the right with a rongeur.
NOTE: Multiple options can be utilized for the carotid injury. Option 1: use an 11-blade knife to make a 3-mm laceration in the right internal carotid artery at the level of the genu. Option 2: puncture directly into the vessel with a nerve hook to produce a tear. Option 3: take a small piece of the vessel wall with a rongeur.
4. Perfusion Set-up
- Insert a 5mm diameter cannula into the common carotid artery and secure with a 5-inch hemostat clamp.
- Connect the cannula to a pressurized perfusion pump.
- Prepare artificial blood consisting of red food coloring, water, and commercially purchased vampire blood [see Table of Materials]. Make artificial blood of the same relative density of real blood by using a 3:1 ratio of water to vampire blood. Add 2 drops of red food coloring for each 250 mL of water added.
NOTE: Artificial blood may be reused for multiple simulations. 3 liters of blood should be prepared for each cadaveric head prior to the start of simulation. It can be stored at room temperature, but should be shaken and mixed prior to use.
5. Establish Realistic Bleeding
- Set up an arterial line via the cannulated carotid artery.
- Start the perfusion pump and measure actual mean arterial pressure (MAP) delivered to the cadaver head via an arterial line transducer and vital signs monitor. Visualize the realism of the carotid injury via endoscopic examination.
NOTE: MAPs of 65-110 mm Hg should be used to produce realistic bleeding parameters depending on the clinical simulation scenario. Flow rate can be adjusted on the perfusion pump in order to reach physiologic MAPs.
6. Training Resident Learners
- Pair one neurosurgery or ENT resident with one anesthesia resident for each of the simulation scenarios.
- Give resident teams approximately 10 min to complete each scenario, with a 10 min debrief (5 min specialty specific, 5 min interprofessional) after each scenario.
- Provide a specialty-specific debrief for 5 mins.
- Deliver interprofessional debrief to residents from both specialties for 5 mins.
- Surgery residents
NOTE: The following steps are to be carried out as instructed by the supervising faculty.- Provide each learner with the same bony exposure, location, and size of cavernous carotid injury.
- Hold the endoscope and provide instructions to the surgery resident for how to manage vascular control. The residents work with the supervising faculty to manage the vascular injury using the 4-handed approach.
- Manage the scenario by 1) giving instructions to anesthesia residents to decrease blood pressure 2) asking for proximal vascular control, 3) using suction to guide the bleeding away from the endoscope, and 4) using a pituitary instrument to place a half cottonoid patty over the bleeding site and apply pressure. The bleeding must be adequately controlled with suction to visualize where to place the cottonoid patty.
- Exchange the cottonoid patty for a free muscle graft harvested from the temporalis muscle. Place the muscle directly over the right cavernous carotid artery injury with a good seal over the incision site. Blood should not be flowing into the cavernous cavity when the muscle patch is in place.
- Anesthesia residents
- Connect the anesthesia station to a simulated mannequin that is connected to a laptop, patient monitor, anesthesia cart with drug tray, anesthesia machine, anesthesia monitor, IV poles, IV bag, and two functional IV units.
- Setup arterial line with pressure monitor.
- Provide anesthesia residents with instructions on use of provided materials, computer, and monitor before starting the simulation.
- Task anesthesia residents with medical management and working as a team with the surgical resident during the simulation scenarios.
7. Enhancing realism
- Give learners different clinical scenarios for patients with varying comorbidities. The comorbid factors will cause changes in bleeding rate and pressure, which should be manually controlled by the faculty by adjusting the perfusion pump settings.
- Task learners with technical and medical management challenges of catastrophic bleeding, and have learners appreciate the medical ramifications that develop.
- Incorporate a simulated mannequin with the cadaveric head model to provide realistic feedback about changes in vital signs and patient stability.
8. Crisis management
- Provide learners with cases of increasing complexity and have them manage multiple changes in vital signs while successfully maintaining vascular control.
NOTE: Learners should effectively communicate so that team members address worsening patient status in a quick and effective manner.
9. Charting Outcomes
- Provide learners with post-simulation surveys to assess the value of the simulation.
- Facilitators should provide focused sessions with the individual learner to discuss ways to improve on communication and technique.
- Provide pre- and post-simulation anatomy exams to assess knowledge gain.
Wyniki
To successfully set-up the model it is important to select an appropriate perfusion pump and to properly prepare the cadaveric head. The pump should be fed into the internal carotid artery as depicted in Figure 1. Once the perfusion pump is set up, the steps outlined above should be employed to gain exposure to the cavernous carotid artery and to produce a realistic cavernous carotid injury. Visualization of the injury with subsequent placement of the muscle patch can be appreciated in Figure 2. The cadaveric head can be combined with the simulated mannequin to produce more clinically relevant scenarios. Vital signs and biometric data change in response to the learner's decisions and intervention choices made during the simulation. The complexity of the cases can vary in terms of patient comorbidities and how these comorbidities may exacerbate management. Representative scenarios are outlined in Table 1. The learners can be evaluated during the simulation on technique, confidence, communication, and leadership. A representative scoring rubric is shown in Table 2. Following the completion of the training, debriefing occurs where facilitators discuss guidelines and algorithms for clinical management, effective communication strategies, and how to effectively manage a crisis. Key points for the facilitator discussion are outlined in Table 3. Following the simulation, learners have the opportunity to provide feedback about the training experience. This feedback can be incorporated to improve the training for subsequent sessions. Representative feedback questions are provided in Table 4.

Figure 1. Cadaveric head model with attached perfusion pump5 – simulated mannequin shown without attachment at neck of cadaver head. Please click here to view a larger version of this figure.
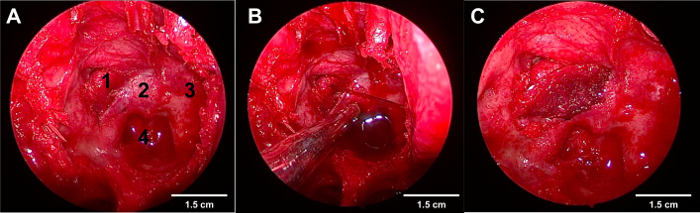
Figure 2. Endoscopic visualization of the cavernous carotid artery injury and successful placement of muscle flap. Please click here to view a larger version of this figure.
A. Endoscopic endonasal transphenoidal approach to the pituitary gland
1. Right cavernous carotid with injury at the genu
2. Sella
3. Left cavernous carotid
4. Clivus
B. Active bleeding from the right cavernous carotid artery
C. Muscle patch technique for repair of right cavernous carotid injury
| Scenario | Description | Relevant History | Induction | Case |
| Scenario 1 | 41-year-old male scheduled for a trans-nasal resection of a pituitary adenoma. The patient had complaints of a headache and feeling cold. | Hypothyroidism treated with levothyroxine. | The case had an uneventful induction with fetanyl 150 mcg, propofol 180 mg, lidocaine 100 mg, and rucoronium 70 mg. Intubation was easy and a 16 gauge PIV was placed in the right AC. Ancef was given as well as dexamethasone. | BP 124/78, HR 78, SpO2 99%. Tidal volume is 450 and rate 12. PEEP was 0. Bleeding begins to increase from surgical site. The anesthesia and neurosurgery residents must work together to manage the bleed and reduce BP. |
| Scenario 2 | 78-year-old female scheduled for a trans-nasal resection of a pituitary adenoma. The patient has complaints of headache, loss of peripheral vision, and feeling cold. | Coronary artery disease with 4 stents placed in the RCA and LAD distributions. Ischemic cardiomyopathy with LEVF 35% on ECHO. Hypertension and OSA on CPAP. Diabetes mellitus type 2, hypothyroidism. Medications include levothyroxine, simvastatin, carvedilol, NPH and normal insulin, and plavix. | The case had an uneventful induction with fentanyl 150 mcg, propofol 120 mg, lidocaine 100 mg, and rocuronium 60 mg. Intubation was easy and a 16 gauge PIV was placed in the right AC. Ancef was given as well as dexamethasone. | BP 164/78, HR 74, SpO2 99%. Tidal volume 450 and rate 12. PEEP was 0. Bleeding begins to increase from surgical site. The anesthesia and neurosurgery residents much work together to mange the bleed and reduce BP. If BP becomes very low, may increase ectopy with or without ischemia. |
| Scenario 3 | 66-year-old male scheduled for for a trans-nasal resection of a macroadenoma. | Healthy patient with normal labs. Hypocortisolemia has been present for the past year. | The case had an uneventful induction with fentanyl 150 mcg, propofol 120 mg, lidocaine 100 mg, and rocuronium 60 mg. Intubation was easy and a 16 gauge PIV was placed in the right AC. Ancef was given as well as dexamethasone. | BP 102/61, HR 88, SpO2 99%. Tidal volume 450 and rate 12. PEEP was 0. Bleeding begins to increase from surgical site. Severe hypotension develops that is refractory to IV fluids and pressors. The anesthesia and neurosurgery residents much work together to mange the bleed and reduce BP. In order to successfully treat the patient, the residents have to note that the hypocortisolemia is the cause of the refractory hypotension. |
Table 1. Representative clinical scenarios that can be utilized for crisis management training
| Category | Element | Score | ||
| (1-4) | ||||
| Situation Awareness | Gathering Information | |||
| Understanding Information | ||||
| Projecting and anticipating future state | ||||
| Decision Making | Considering options | |||
| Selecting and communicating options | ||||
| Implementing and reviewing decisions | ||||
| Communications and Teamwork | Exchanging information | |||
| Establishing a shared understanding | ||||
| Coordinating team activities | ||||
| Leadership | Setting and maintaining standards | |||
| Supporting others | ||||
| Coping with pressure | ||||
Table 2. Feedback scoring chart for crisis management - scenario performance chart. 1=poor, 2=fair, 3=good, and 4=excellent.
| 1 | What went well? What might you do differently next time? What are areas where you need to improve? | ||||
| 2 | How do you feel you did with communication? How are these communication skills relevant to other situations? Was it helpful working with other team members? | ||||
| 3 | How is this simulation relevant to other crisis situations? Do you feel you are more equipped to manage a crisis in the operating room? | ||||
| 4 | Did you develop an algorithm for vascular control? Do you feel you can apply this algorithm to other similar situations? | ||||
Table 3. Debriefing questions that can be used by the facilitator.
| 1 | Did you find the simulation session valuable? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 2 | Did you develop an algorithm for managing carotid artery? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 3 | Do you feel more comfortable using endoscopic instrumentation? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 4 | Do you feel comfortable working with residents from other specialties? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 5 | Is simulation a good complement to operative experience? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 6 | Simulation improved my surgical skill set | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 7 | Do you feel comfortable with Crisis Resource Management | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 8 | Would you like to see further similar simulated experiences offered in the future? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 9 | Can the lessons learned/experienced in the simulation be translated to other crisis scenarios? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 10 | The simulation model offers benefits not available in existing training models | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 11 | Was this course valuable in your training experience? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 12 | Skills learned in the simulated environment translate to the operating room | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 13 | Simulated experiences should be incorporated into surgical training prior to entering the operating room | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 14 | Simulation improved/reinforced my understanding of the relevant anatomy | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 15 | Would you like to see simulation integrated into the curriculum? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 16 | If given the choice, would you participate in simulation in the future? | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
Table 4. Representative post-training survey questions with scoring rubric.
Dyskusje
Carotid injury is a rare event but does occur in cases that involve the extended transphenoidal approach8. This approach is commonly used for pathology of the sella, suprasellar, parasellar, and clival spaces. Most skull base surgeons will face a carotid vascular injury at some point in their career. The expertise and confidence to handle such a dilemma can only be obtained through adequate training and appropriate crisis management simulation3. Valentine and colleagues have shown the relevance of using simulated training for carotid vascular injury2. Several models have been designed for such training purposes including Wormald's sheep model, Pham's whole body cadaver model, and Muto's synthetic polyamid nylon and glass bead model1,4,7. This paper presents the detailed protocol and results for a cadaveric head model, which incorporates multidisciplinary training in surgical and medical management.
The benefit of using a cadaveric head model is its cost-effectiveness, reproducibility, and ease of set-up5. Furthermore, as described in both the protocol and video, the model can be combined with a simulated mannequin. This opens the door to interdisciplinary training between residents from different specialties such as anesthesiology, neurosurgery, and otolaryngology. The clinical scenarios can then be expanded from building techniques alone to the more important skill of establishing interdisciplinary algorithms for crisis management. One of the key training points is how to effectively communicate with team members from different disciplines. Facilitators, in real-time, adjust parameters to make the model respond to the learners' actions. Resident learners can then be debriefed on both technical performance as well as effective communication between colleagues. By having such a dynamic model, teamwork can be emphasized during the simulation session and learners can appreciate a more realistic view of crisis management.
Padhye and colleagues have set up catastrophe management workshops that have trained numerous surgeons over the years9. These workshops have shown the superiority of muscle patches for managing carotid vascular injury and have been an excellent resource for surgeons in training to improve techniques10. While workshops are beneficial, the primary limitation is the lack of widespread adaptability due to the limited resources available at other sites to implement similar training. The reproducibility of this cadaver preparation has been demonstrated previously5. Doumouras and colleagues have shown that implementing simulation early on improves residents' surgical technical skills throughout residency11.
One of the benefits of simulation is that early training enhances learner confidence so that he or she can then focus on interdisciplinary communication. Interdisciplinary simulation has been shown to be more effective in improving patient outcomes than single specialty training sessions or workshops12. The model outlined in this paper allows simulation to be adaptable to the institution and to focus on the crisis management most relevant to their region. This is valuable in that surgery teams can train and practice in a realistic setting prior to entering the operative arena. It also provides a safe learning environment so that algorithms can be established without jeopardizing patient care13. By modifying the debriefing sessions, institutions can also focus on the aspects they deem most relevant to their learners14.
This paper highlights a protocol for establishing a cadaveric head cerebral perfusion model and crisis management simulation. The benefits of this model are its cost-effectiveness, ease of set-up, and adaptability. The video shows how the model can be combined with a simulated mannequin to enhance the realism of the training. This ultimately opens the door to interdisciplinary training, focused clinical scenarios, and individualized debriefing sessions. By incorporating the model early on in resident training, learners will be able to develop skill sets and algorithms that will last their entire career.
Ujawnienia
The authors have nothing to disclose.
Podziękowania
The authors have no acknowledgements.
Materiały
| Name | Company | Catalog Number | Comments |
| Anti-coagulant citrate dextose solution | Pierce Laboratories | 117037 | |
| Embalming solution | Chemisphere | ||
| Formalin fixative | Chemisphere | B2915DR55 | |
| Zero degree endoscope (4mm and 18 cm length) | Karl Storz | H3-Z TH100 | |
| Penfield 1 | Jarit | 285-365 | |
| Kerrison rongeur | Aesculap | FM823R, 3mm/180 mm | |
| Anspach eMax 2 Plus High Speed Drill | Depuy-Synthes | eMax2 plus | |
| 3 mm cutting ball | Depuy-Synthes | ||
| 11-blade surgical blade | Bard-Parker | 371111 | |
| Arterial cannula clamp | |||
| Arterial cannula | Instrument Design & Mfg. Co. | ART187-2-CT | |
| Perfusion Pump | Belmont Instrument Corporation, Billerica, MA, USA | Belmont Fluid Management System 2000 | |
| Vampire blood | Forum Novelties, Inc., Melville, NY, USA | 65368 | |
| Cottonoid surgical patties | Codman | 80-1480 | |
| Laerdal SimMan | Laerdal Medical, Wappingers Falls, NY, USA | SimMan 3G | |
| Laerdal SimMan Laptop | Laerdal Medical, Wappingers Falls, NY, USA | SimMan 3G | |
| Pituitary rongeur | Aesculap | FF806R | |
| Bayonet | Aesculap | BD 845 | |
| Suction - 7 and 10 FR | V. Mueller | ||
| IV poles | Pedigo | ||
| IV unit | Care Fusion | Alaris PC Unit | |
| Pump modules | Care Fusion | Alaris Pump Module | |
| Kit Arterial Line | Arrow International | RA-04020 | |
| Kit Pressure Monitor | ICU/BMP Inc | 426340405 | |
| Fluid IV NaCl 0.9 1000CC) | Baxter Healthcare | 2B1324X | |
| Fluid IV lactated ringers 1000CC | Baxter Healthcare | 2B2324X | |
| Integra SL Anesthesia Machine | DRE | 00104RS | |
| AVS2 Remote Ventilator | DRE | 409AVS2 | |
| Sigma Delta ISO Selectatec Vap Pour Fill | DRE | 39001O | |
| MP5 Bedside Monitor | Philips Healthcare | PMS-M8105a |
Odniesienia
- Muto, J., Carrau, R. L., Oyama, K., Otto, B. A., Prevedello, D. M. Training model for control of an internal carotid artery injury during transsphenoidal surgery. Laryngoscope. 127 (1), 38-43 (2017).
- Valentine, R., Padhye, V., Wormald, P. J. Management of arterial injury during endoscopic sinus and skull base surgery. Curr Opin Otolaryngol Head Neck Surg. 24 (2), 170-174 (2016).
- Valentine, R., Padhye, V., Wormald, P. J. Simulation Training for Vascular Emergencies in Endoscopic Sinus and Skull Base Surgery. Otolaryngol Clin North Am. 49 (3), 877-887 (2016).
- Padhye, V., Valentine, R., Wormald, P. J. Management of carotid artery injury in endonasal surgery. Int Arch Otorhinolaryngol. 18 (Suppl 2), S173-S178 (2014).
- Ciporen, J. N., Lucke-Wold, B., Mendez, G., Cameron, W. E., McCartney, S. Endoscopic Management of Cavernous Carotid Surgical Complications: Evaluation of a Simulated Perfusion Model. World Neurosurg. , (2016).
- Ciporen, J., Lucke-Wold, B., Dogan, A., Cetas, J. S., Cameron, W. E. Dual Endoscopic Endonasal Transsphenoidal and Precaruncular Transorbital Approaches for Clipping of the Cavernous Carotid Artery: A Cadaveric Simulation. J Neurol Surg B Skull Base. 77 (6), 485-490 (2016).
- Pham, M., et al. A Perfusion-based Human Cadaveric Model for Management of Carotid Artery Injury during Endoscopic Endonasal Skull Base Surgery. J Neurol Surg B Skull Base. 75 (5), 309-313 (2014).
- Ogawa, Y., Tominaga, T. Extended transsphenoidal approach for tuberculum sellae meningioma--what are the optimum and critical indications?. Acta Neurochir (Wien). 154 (4), 621-626 (2012).
- Padhye, V., et al. Coping with catastrophe: the value of endoscopic vascular injury training. Int Forum Allergy Rhinol. 5 (3), 247-252 (2015).
- Padhye, V., et al. Early and late complications of endoscopic hemostatic techniques following different carotid artery injury characteristics. Int Forum Allergy Rhinol. 4 (8), 651-657 (2014).
- Doumouras, A. G., Engels, P. T. Early crisis nontechnical skill teaching in residency leads to long-term skill retention and improved performance during crises: A prospective, nonrandomized controlled study. Surgery. , (2016).
- Sauter, T. C., et al. Interprofessional and interdisciplinary simulation-based training leads to safe sedation procedures in the emergency department. Scand J Trauma Resusc Emerg Med. 24, 97 (2016).
- Saver, C. Simulation lab a safe way to practice crisis management. OR Manager. 32 (2), 13-17 (2016).
- Isaranuwatchai, W., Alam, F., Hoch, J., Boet, S. A cost-effectiveness analysis of self-debriefing versus instructor debriefing for simulated crises in perioperative medicine. J Educ Eval Health Prof. , (2016).
Przedruki i uprawnienia
Zapytaj o uprawnienia na użycie tekstu lub obrazów z tego artykułu JoVE
Zapytaj o uprawnieniaPrzeglądaj więcej artyków
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. Wszelkie prawa zastrzeżone