Method Article
A Pilot Study Showing Application of Palatal Bone Harvesting Under Dynamic Navigation Guidance in Oral Implantology
In This Article
Summary
The protocol introduces a novel surgical method for palatal ring bone block harvesting using dynamic navigation guidance, addressing the challenge of insufficient bone volume in typical intraoral grafting areas and offering a viable solution for effective bone augmentation in implant dentistry.
Abstract
In cases of insufficient bone volume in the implant area, bone augmentation surgery is often required to ensure an adequate amount of bone around the implant. In autologous bone grafting procedures, some patients face insufficient bone volume at conventional intraoral bone harvesting sites. Due to the high difficulty associated with completing palatal osteotomies freehand, fewer palatal lateral osteotomies have been reported, and palatal bone blocks are not routinely used in bone augmentation procedures. With the development of digitally guided implant technology, palatal bone harvesting has become feasible. In this paper, we will present a method of obtaining a circumferential bone block of the palate for implant surgical application through dynamic navigation guidance. A total of three patients had undergone this procedure to obtain circumferential palatal bone blocks and completed bone augmentation surgery. The bone augmentation results in the implanted area have been favorable, and there has been some bone recovery at the harvesting site. This is a safe and effective way to obtain intraoral bone blocks.
Introduction
In recent years, with the advancement of implant technology, more and more patients with tooth loss are choosing dental implants for restorative treatment1,2. One of the keys to implant success is adequate bone volume in the alveolar ridge. Patients often experience varying degrees of alveolar bone resorption after tooth extraction. According to previous studies, the alveolar ridge width decreases by 5-7 mm, and the alveolar ridge height decreases by 2-4.5 mm within 12 months after tooth extraction3. Therefore, bone augmentation is a very important part of oral implantology, which offers the possibility of performing implant surgery in patients with inadequate implant conditions.
Patients with different types of alveolar ridge defects are treated with different bone augmentation techniques, such as distraction osteogenesis4, Maxillary Sinus Floor Elevation5, Guided Bone Regeneration6, Onlay Bone Graft7, etc. Autogenous bone block grafting is a common surgical option for patients with substantial loss of alveolar ridge width and height for better support and osteogenesis. Patients with severe bone defects require larger autograft bone blocks. Petrungaro and other scholars have statistically shown that ascending ramus, anterior mandible, and tuberosity, among the intraoral bone retrieval sites, yielded about 5-10 mL, 5 mL, and 2 mL of bone volume, respectively. Extraoral bone retrieval sites, including the posterior iliac crest, anterior iliac crest, tibia, etc., can obtain 20-70 mL of bone volume, but the difficulty and risk of extra-oral bone block retrieval surgery is high8.
In some patients, the conventional intraoral bone extraction site is unable to provide the appropriate volume of bone. A 2013 imaging-related study by Qinghua et al. showed that the maxillary palate is a potential osteotomy area in the oral cavity9. The palatal bone is predominantly cortical, supplemented by cancellous bone, and bone fragments obtained from this site exhibit good supportive and osteogenic properties. The palate also has a rich blood supply, is covered by keratinized epithelium, and demonstrates a high healing capacity after osteotomy. Because the palate lies in a blind area of the surgical field, and the operating space is constrained by the patient's mouth opening degree, the operational space is adjacent to critical anatomical structures such as the nasal cavity, maxillary sinus, and multiple tooth roots. Consequently, the difficulty of performing a freehand palatal osteotomy is high, which is why palatal osteotomy is seldom reported, and palatal bone blocks have not been widely used in bone augmentation surgeries. The absence of a specific tool for palatal bone extraction further increases the difficulty of the operation.
With the advances in computer-assisted implant surgery (CAIS), maxillary palatal bone extraction became possible. Static guides are difficult to apply to maxillary palatal osteotomies due to resin and guide ring thickness requirements, which require an increased degree of patient mouth opening10. The emergence of the dynamic CAIS system overcomes the above difficulties. The dynamic CAIS system uses motion-tracking technology to track implant drilling instruments and the patient's jaw position. This achieves real-time tracking of the surgery and feedback on the software to guide the surgery in real time11. Dynamic navigation makes maxillary palatal osteotomies possible by ensuring the accuracy of the osteotomies with low requirements for the patient's mouth opening and allowing for clear visualization of the operation.
Protocol
The study was approved by the Ethics Committee of West China Stomatological Hospital of Sichuan University (No. WCHSIRB-D-2021-209-R1), and all participants volunteered to participate in this clinical trial and signed an informed consent form. All patients were admitted to the Department of Implantology at West China Stomatological Hospital, Sichuan University, China, presenting with dental defects characterized by horizontal or vertical bone defects and expressing a desire for implants.
1. Patient information collection
- Select patients based on the following inclusion criteria: age 18-65 years; good oral hygiene; no systemic disease or well-controlled systemic disease; patients presenting dental defects with horizontal or vertical bone defects and wishing to receive implants; patients were compliant, volunteered to participate in this clinical trial, and signed an informed consent form.
- Exclude patients based on the following exclusion criteria:patients with a low amount of bone loss in the edentulous area who do not require block bone grafting; patients who do not have sufficient bone in the palatal bone extraction area for palatal bone extraction operation;acute inflammation of neighboring teeth, degree II looseness or greater, or one-walled sub-bone pockets; osteoporosis or history of taking or injecting bisphosphonates; those with poorly controlled systemic diseases; history of head and neck radiation therapy; female patients who are pregnant or breastfeeding are not candidates for implant surgery;those who are unable to cooperate with the follow-up examinations.
- Collect DICOM data from Cone Beam Computed Tomography (CBCT) scans, imaging in 100 x 100 mm (WXH), with a scan time of 30 s, performed on patients wearing the registration device.
- Select the appropriate type of registration device according to the patient's intraoral condition (Figure 1). Secure the registration device to the patient's remaining maxillary teeth using polyether impression material in a position as close to the missing teeth as possible. Perform hand-assisted fixation for 5 min to allow the material to set thoroughly.
- Take off the registration device and remove the excess material with a scalpel. Reposition the registration device in the patient's mouth and check for firmness of repositioning. If resetting is not possible or firmness is poor, remove all polyether material and repeat step 1.3.1.
- Take CBCT after the registration device is placed on the patient and check its stability. Use cotton balls to elevate the patient's posterior teeth to prevent displacement of the registration device when the patient bites into it during filming. Obtain DICOM data of CBCT scans while the patient is wearing the registration device (Figure 2A).
- Perform an oral scan of the patient to obtain data from the patient's intraoral model using an oral scanning instrument or alginate modeling (Figure 2B).
2. Designing the dynamic navigation software
- Create a new patient. Click on Open Case. Import DICOM data and oral scan data into the software.
- Based on the preliminary design of the patient's implant surgery, create the implant, crown, and abutment tooth position. Place additional implants at the 14th and 24th tooth positions to indicate the maxillary palatal bone extraction sites. If the patient's implant design involves the 14th and 24th positions, replace the implant, marking palatal bone extraction as necessary.
- Click Start Design. Click on Cutter to remove parts of the CBCT model that interfere with the design by trimming it. Take care to preserve the high-density radiolucent points of the registration device and essential structures such as the maxillary palate and implant sites.
- Click on Crown Design on stl to virtually align the missing teeth, paying attention to occlusion and gingival margin position in order to achieve restoration-oriented implant therapy.
- Click Panorama Curve. Draw a panoramic line at the apex of the maxillary alveolar ridge. Click stl superimposition. The CBCT data is then fitted to the intraoral model data.
NOTE: The software features AI (Artificial Intelligence) operation for fitting, but manual fitting should be used if AI fitting is unsatisfactory. Manual fitting involves aligning the CBCT model with the hard tissue of the intraoral model's teeth by selecting four identical points, which should be as spread out as possible. - Check the fitting results by observing whether the outer contour of the crown on CBCT coincides with the contour line of the intraoral model. If there is a deviation, repeat the manual fitting in step 2.5, replacing the tip as appropriate, until the fitting is successful.
- Click Implant Design. Perform implant, bone harvesting and bone augmentation surgical designs.
- Place virtual implants in the edentulous area and position them on implants or bone block retaining nails as required. Click Fine-tune Implant to make fine adjustment (Figure 3).
- Click on positions 14 and 24 in the schematic at the top left of the page to create virtual implants. Ensure the diameter and length of the virtual implant matches the design of the bone extraction.
- Drag the virtual implant to the palate, place it and fine-tune it according to the bone retrieval design. Perform a detailed inspection after placement, taking care to avoid damaging adjacent important anatomical structures, and retain at least a 1.5 mm safety distance (Figure 4).
- Click Set Marker Points. By clicking on the high-resistance radiographic spot in the 3D CBCT model, the software will automatically detect the registration device model for matching.
- Save and export the project. Import it into the navigation software on the computer connected to the Position Sensor prior to surgery.
3. Dynamic navigation preparation
- Installation of patient tracker and fixing device
- Select the appropriate fixing device according to the placement position, while avoiding the registration device and the surgical area (Figure 5).
- Connect the patient tracker to the fixing device using the connection device (Figure 6). Restore the registration device to the patient's mouth, place the fixing device in the patient's mouth, and adjust the movable joints of the connection device to the appropriate position before fixing them. Ensure that the patient tracker is not obscured by intraoperative maneuvers of the operator and that the receiver of the position sensor acquires the relevant information.
- After filling the fixing device outside the mouth with composite resin material, fix the patient tracker to the patient's remaining maxillary teeth through the fixing device using the composite resin material (Figure 7). Stabilize the intraoral fixation device for 3-5 min and not release it until the temporary crown material has completely solidified.
- Check the security of the patient tracker by lightly touching it. If it is loose, repeat step.
- Intraoperative registration
- Click on the Patient Tracker icon to enter the calibration screen.
- Select the corresponding code in the software based on the actual Handpiece Tracker and Patient Tracker version being used for the current procedure.
- Adjust the position and angle of the Position Sensor and Handpiece Tracker so that the Position Sensor receives signals from the Handpiece Tracker and Patient Tracker in a stable manner. Then, click Registration.
- Intraoperative calibration
- Click on the Calibration button at the lower right corner to enter the alignment screen.
- Confirm the tightness of the registration device after resetting. Replace the drill pin with a short ball drill for Dynamic Navigation. Use a short ball drill to tap the spherical pit of the registration device while the assistant clicks the Calibration button on the software. Repeat 5x-6x by replacing different spherical pits.
- Check the accuracy of calibration computed by AI; a tolerance within 0.3 mm is recommended. If the accuracy tolerance is too large, delete the data and repeat step 3.2. After confirming the accuracy, click Start Navigation.
4. Palatal bone extraction and alveolar ridge bone grafting under Dynamic Navigation guidance
NOTE: In the following operations, each time the operator changes the drilling needle, the assistant must select the appropriate type of drilling needle in the software. The operator is advised to verify this by placing the tip of the drill pin on the cusp of the crown of the neighboring tooth and observing whether the position shown on the navigation software corresponds to reality (Figure 8).
- After local anesthesia is completed, use a pioneer drill under Dynamic Navigation guidance to locate the bone extraction site. Use a 2 mm diameter twist drill for guided cavity preparation. According to the preoperative design of the diameter of the bone extraction, use the corresponding guided osteotomy ring drill to extract the bone.
- Take the soft tissue above the ringbone block and place it in saline for later use.
- Prepare the central hole of the ringbone block according to the surgical design. For example, for patients requiring bone ring surgery have the center of the bone block reamed incrementally based on the size of the implant being used.
- Carefully remove the ringbone block using a minimally invasive dental elevator. Place the ringbone block in situ on the palate or in saline for later use (Figure 9).
- Complete the bone grafting procedure according to the surgical design (Figure 10).
5. Treatment of palatal wounds
- Place silver-containing gelatin sponges in the holes of the palatal fossa to assist in hemostasis. Use surgical sutures (Monofilament polypropylene suture 5-0 ) to secure the soft tissue to the palatal incision.
- Apply compression with a gauze ball to stop bleeding. Take an alginate impression as soon as possible after the operation and make a pressure-membrane retainer-type palatal shield for the patient on the same day.
- Instruct patients to perform 24 h postoperative wear and only remove the palatal guard for cleaning after each meal. Palate guards should be worn for 30 days.
- After surgery, perform a maxillary CBCT scan. Follow-up appointments are made 1 week, 2 weeks, and 1 month after surgery. Remove stitches 2 weeks after surgery.
- Postoperatively, instruct patients to take amoxicillin capsules (0.25 g, 3x a day) for 7 days. If allergic to penicillin, give azithromycin (0.25 g, 1x a day), and diclofenac sodium extended-release capsules (Intaquan 0.1 g, 2x a day) to relieve postoperative pain as necessary. Additionally, ask patients to use 0.12% cotrimoxazole rinse solutions for gargles (10 mL, 2x- 3x a day) for 1 month postoperatively. Remove sutures 2 weeks after the operation and conduct oral hygiene counseling.
Results
Between May 2021 and May 2022, three patients were included in the West China Hospital of Stomatology at Sichuan University to complete palatal osteotomies. Obtained ring bone blocks of palatal origin were used for autologous bone ring grafting and implanted during simultaneous implant surgery. All patients received 3.3 mm Straumann implants. All patients successfully integrated the grafted bone block, the implant osseointegration was well established, the restorations were good, and the patients were satisfied with their aesthetics and function. The results show that the use of palatal ring bone blocks in the oral cavity can achieve good bone augmentation effects, allowing implant surgeries to be completed.
At the 1-month postoperative follow-up, all patient's palatal osteotomy incisions achieved clinical stage I healing (Figure 11). Postoperatively, patients wear a palatal shield, allowing for localized light pressure compression of the wound to prevent bleeding, protect the wound, and allow patients to complete daily activities such as speaking and eating. One month after the surgery, the palatal bone extraction site can achieve good soft tissue healing, and patients can restore normal oral physiological functions.
Accuracy of bone extraction
Postoperative bone extraction accuracy analysis was done with commercial software, and measurements of the site tolerance and angular error between the designed osteotomy and the actual misalignment were taken (Figure 12). The results are shown in Table 1, with a mean angular misalignment of 4.28° ± 3.36° and a mean site tolerance of 1.01 ± 0.25 mm. Using dynamic navigation to guide the extraction of palatal ring bone blocks ensures precision in bone extraction, making it safe and feasible.
| Angular misalignment (°) | Site tolerance (mm) | |
| Case1 | 7.73 | 0.74 |
| Case2 | 1.02 | 1.08 |
| Case3 | 4.08 | 1.22 |
| mean | 4.277 ± 3.359 | 1.013 ± 0.2468 |
Table 1: Osteotomy precision error. A mean angular misalignment of 4.2877° ± 3.3659° and a mean site tolerance of 1.013 ± 0.25468 mm was obtained.
Bone dimensions measurement
All CBCTs were modeled, and CBCT scans were performed at different times in the same patient, and the remaining teeth were fitted (Figure 13). The height increments of the labial side, the center of the long axis of the implant, and the lingual side were measured in the direction of the long axis of the implant, and the average value was recorded as the peri-implant bone height increment at 6 months postoperatively (Figure 14A). The bone increment values were measured at the neck of the implants on both labial and lingual sides. Measurements were taken correspondingly at 0 mm, 1 mm, 2 mm, and 3 mm below the neck, and the mean values were recorded as the labial bone increment values and the lingual bone increment values, respectively (Figure 14B).
At 6 months after palatal bone ring grafting, the height of peri-implant bone augmentation was 5.04 ± 0.66 mm, bone increment on the labial side was 3.55 ± 0.55 mm, and bone increment on the lingual side was 1.94 ± 0.84 mm (Table 2). The peri-implant bone volume can be effectively restored using palatal bone rings for simultaneous implantation, providing the foundation for dental restoration.
| Height of bone (mm) | Labial side (mm) | Lingual side (mm) | |
| Case1 | 3.23 | 2.97 | 1.44 |
| Case2 | 1.64 | 4.07 | 2.91 |
| Case3 | 1.83 | 3.61 | 1.47 |
| mean | 5.043 ± 0.656 | 3.550 ± 0.552 | 1.94 ± 0.840 |
Table 2: Bone gain at 6 months after the implantation. The height of peri-implant bone augmentation was 5.04 ± 0.66 mm, bone increment on the labial side was 3.55 ± 0.55 mm, and bone increment on the lingual side was 1.94 ± 0.84 mm. The peri-implant bone volume can be effectively restored using palatal bone rings for simultaneous implantation, providing the foundation for dental restoration.
Healing of the bone removal area
At 6 months after the operation, the patient was seen to have no visible scarring on the palatal side, and the site of bone extraction had completely healed, with no negative impact on the patient's long-term quality of life.
CBCT at 6 months postoperatively showed complete remodeling of the palatal bone tissue. CBCT models were fitted to the preoperative, operation day, and 6-month postoperative CBCT models and volume differences were calculated using Mimics software. The volume difference between the preoperative CBCT model and the operation day-CBCT model was counted as the volume of bone taken (Figure 15A). The volume difference between the 6-month postoperative CBCT model and the operation day-CBCT model was recorded as the bone recovery volume (Figure 15B). Bone recovery rates in three patients were between 25.23% and 54.46%, as shown in Table 3. At 6 months after the surgery, new bone formation can be observed at the bone extraction sites, indicating that the upper palatal part is a potential reusable bone source within the oral cavity.
| Bone removal volume (mm3) | Bone recovery volume (mm3) | Bone recovery rates | |
| Case1 | 211.44 | 115.14 | 54.46% |
| Case2 | 254.36 | 67.22 | 26.43% |
| Case3 | 364.58 | 91.97 | 25.23% |
Table 3: Bone recovery at 6 months after palatal osteotomy. Bone recovery rates were between 25.23% and 54.46%.
Based on the above results, it is evident that obtaining palatal bone rings guided by dynamic navigation is safe and effective. After surgery, both soft tissue and bone tissue heal well. At 1 month after the surgery, patients can resume normal oral physiological functions, and new bone formation can be observed 6 months post-surgery. The use of palatal bone rings in simultaneous implant surgery shows good bone augmentation effects 6 months post-surgery, demonstrating that palatal bone rings can provide the necessary bone augmentation needed for oral implant surgeries.

Figure 1: Different types of Registration Devices. The choice of the registration device is based on the patient's missing tooth area. Please click here to view a larger version of this figure.

Figure 2: Obtaining DICOM data for CBCT. The DICOM data was obtained (A) with high resistance radiographic points and (B) patient intraoral scan data. Please click here to view a larger version of this figure.

Figure 3: Navigation software interface. The interface displays a program of planting design. Please click here to view a larger version of this figure.

Figure 4: Navigation software interface. The interface shows options for palatal osteotomy design. Please click here to view a larger version of this figure.
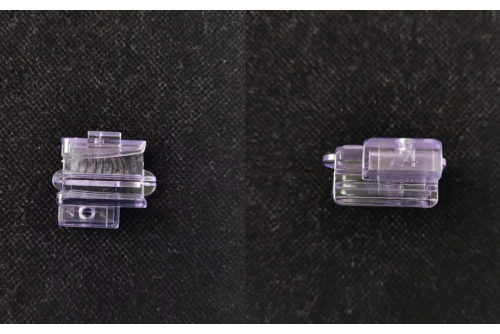
Figure 5: Fixing device. The figure above shows the fixing device, and the numbers on the left represent the intraoral positions in which they can be used. As shown in the picture, 24 can be used for both upper left and lower right dentition. Please click here to view a larger version of this figure.

Figure 6: Connection device setup. Using the Connection Device to connect the patient tracker and the fixing device. Please click here to view a larger version of this figure.
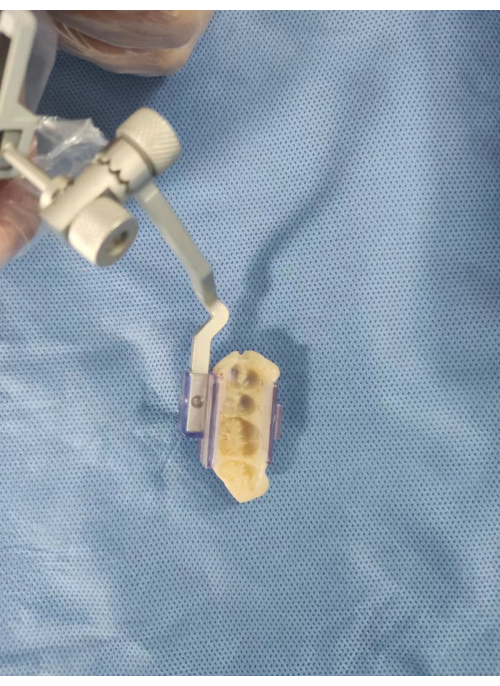
Figure 7: Positioning the fixing device. The fixing device is held in place with composite resin material. Please click here to view a larger version of this figure.

Figure 8: Usage of the drilling needle. (A) The appropriate drilling needle was replaced on the software according to the procedure, and (B) the remaining tooth tip was tapped for verification. Please click here to view a larger version of this figure.

Figure 9: Ring bone block. Diagram showing diameter and thickness of removed ring bone block. Please click here to view a larger version of this figure.

Figure 10: Bone implantation. The bone implant is accomplished using the ringbone block. Please click here to view a larger version of this figure.

Figure 11: Results after 1 month. Photograph of the patient's palatal side incision at 1 month postoperatively. Please click here to view a larger version of this figure.
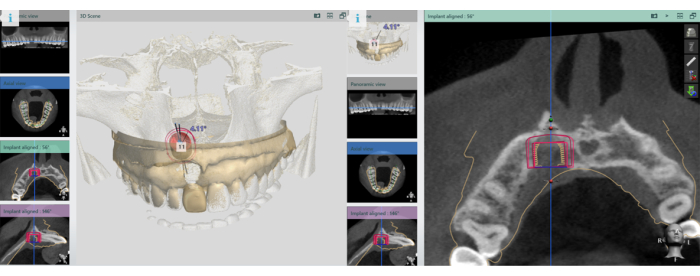
Figure 12: Validation of extraction sites. Perform accuracy validation of bone extraction sites. Please click here to view a larger version of this figure.

Figure 13: Models of patients' CBCT data. The models show CBST data fitted at different times. Please click here to view a larger version of this figure.

Figure 14: Parameter measurement. (A) Bone height gain, (B) labial and lingual bone gain were measured separately. Please click here to view a larger version of this figure.
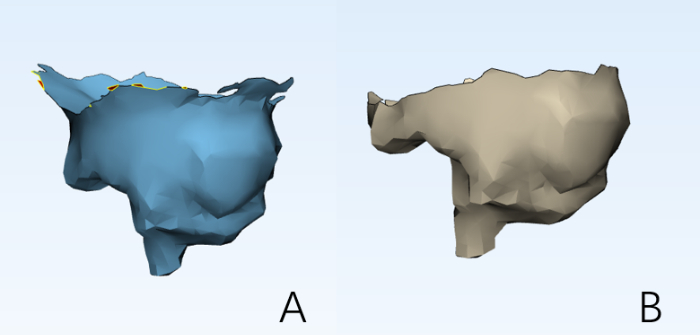
Figure 15: Bohr operations. Bohr operations were performed using the software to obtain a model of (A) the amount of bone taken from the patient and (B) the amount of bone recovered. Please click here to view a larger version of this figure.
Discussion
Block bone grafting is commonly used clinically to enhance bone volume in areas with bone defects. Grafted bone blocks can be categorized into three types based on their source: allogeneic, xenogeneic, and autogenous bone blocks. Allogeneic bone blocks are easier to obtain and relatively inexpensive, but their effectiveness in vertical bone augmentation is limited12. Allogeneic bone can yield better osteogenic results but is more costly and carries risks such as rejection reactions and ethical concerns. Autologous bone grafting features a short interval between bone extraction and grafting, allowing the bone tissue minimal time outside the body13. Its bioactivity and osteoinductivity are significantly stronger than those of other bone substitutes, making it the current standard for bone augmentation14.
Commonly used sites for autologous bone graft extraction include the maxillary tuberosity, mandibular ascending branch, in situ, and chin. The maxillary tuberosity, primarily composed of cancellous bone and having limited bone volume, does not yield block bone; therefore, the preparation of autogenous bone powder is prevalent15. The mandibular ascending branch, dominated by cortical bone, provides good support but poor osteoinductive potential16. The in situ bone ring's preparation risks compromising the amount of bone available for retention in the implantation area, potentially affecting the implant's initial stability17. Lastly, the chin bone ring, consisting of a thin layer of cortical bone and cancellous bone, is suitable for bone ring surgery. However, harvesting bone from this area may cause complications such as numbness of the lower lip18.
Based on previous literature9, the maxillary palate is abundant in bone, making it a potential site for bone retrieval within the oral cavity. The maxillary palate is composed mainly of cortical bone, supplemented by cancellous bone. This bone composition is suitable for a variety of bone augmentation procedures in the oral cavity19. Embryologically, the maxilla and mandible are homologous and have a high rate of bone tissue viability20. All three patients in this trial showed good implant osseointegration on a 6-month review after completing the procedure using a palatal ring bone block. The circumferential bone block provides good bone volume around the implant neck, obtaining a long-term stable bone gain. At 6 months after palatal bone ring grafting, the height of peri-implant bone augmentation was 5.043 ± 0.656 mm, bone increment on the labial side was 3.550 ± 0.552 mm, and bone increment on the lingual side was 1.94 ± 0.840 mm. This result is similar to previous literature in which vertical bone gain averaged approximately 4 mm21.
One article reported on palatal osteotomy using palatal marginal incisions, and a full-thickness flap was elevated, a procedure that accesses only the anterior portion of the palatal bone. Rodriguez-Recio et al. case report used computer software to assist in analyzing palatal bone harvesting and bone grafting procedures but did not use computer-assisted guidance for the surgical procedure22. Although the palate is a potentially high-quality area for bone harvesting in the oral cavity, it is still not routinely utilized in oral bone augmentation procedures. This may be due to the fact that palatal bone extraction is more difficult to achieve during oral local anesthesia procedures. When the patient is in the supine position, the surgeon is unable to look directly at the patient's palate, and the surgical field of view is obstructed. The palate is in close proximity to the patient's nasal cavity and the roots of the anterior teeth and premolars, requiring the use of digitally assisted technology to ensure that the osteotomy procedure is performed smoothly without damaging vital anatomical structures23.
Static guides can satisfy the requirement of high-accuracy bone retrieval, but the guide design needs to satisfy the resin and guide ring thickness10. This further increases the demands on the patient's mouth opening, and therefore, static guides are not adequate for palatal osteotomies. Dynamic Navigation has been used in oral implant surgery since 200024. This is a way of aligning the real oral 3D information with the digitized oral 3D information through the registration device and calibrating the implant handpiece and the patient's jawbone through the handpiece tracker and the patient tracker so as to achieve the connection between reality and the virtual and to guide the surgery. Dynamic Navigation can obtain comparable surgical precision with static guides, and there is no special requirement for the patient's mouth opening degree without blocking the surgical field of view25. In this trial, the palatal osteotomy was performed successfully using Dynamic Navigation without complications such as damage to adjacent important anatomical structures. Postoperative accuracy verification was performed, and the mean angular error was 4.277° ± 3.359°, and the mean locus error was 1.013 ± 0.2468 mm. This is similar to the review of literature results of 1.29 ± 0.50 mm in locus error and 3.06° ± 1.37° in angular error, which suggests that the use of Dynamic Navigation for bone retrieval is a safe and effective technique.
The osteotomy area is on the palate, which is more likely to touch the wound when talking and eating. We recommend that patients wear a pressure film retainer-type palatal guard to facilitate short-term postoperative protection of the incision and to ensure normal speech and feeding function. The soft tissues on the surface of the bone grafting wounds of all patients healed completely within 1 month, and the patients resumed normal physiological functions. On radiographic examination, the rate of bone recovery in the osteotomy area was seen to range from 25.23% to 54.46% at 6 months after operation. This suggests that there is some recovery of bone tissue after maxillary palatal osteotomy, with little long-term impact on the patient.
However, this technique still has some limitations. Using this technique for maxillary palatal osteotomies only allows the acquisition of a bone block to be performed in a circular shape, and it is not possible to obtain a bone block in rectangular or other shapes, which is a limitation for the design of the implant surgery. There are no specialized surgical tools for palatal bone extraction; therefore, the operation remains difficult to perform. Nevertheless, the available sample size is small, and the observation period is short; the relevant application and effect of palatal bone blocks need to be supported by more cases and a longer observation period.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We would like to thank the members of the Department of Implantology at West China Hospital of Stomatology, Sichuan University, for their help in the success of the surgeries. We would also like to thank Ms. Wenshu Dai for reviewing and ensuring the correct English grammar in this article. The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Research and Develop Program, West China Hospital of Stomatology Sichuan University. [grant number LCYJ2022-YY-4].
Materials
| Name | Company | Catalog Number | Comments |
| 3D Bone Graft Set | Zepf | 47.500.31 | |
| 3-matic software | Materialise | 13 | |
| 3Shape software | 3Shape | 1.7.27.6 | |
| Bio-Gide | Geistlich | ||
| Bio-Oss | Geistlich | ||
| Carestream 360 oral scanner | OneX | FN-11 | |
| CBCT scanner Morita 3D Accuitom | Morita | 1620 | |
| Dcarer dynamic navigation | Dcarer | ||
| Dental implant dynamic navigation sys-tem software | Dcarer | 3.0.7.2432 | |
| Dental tines | Zepf | 17.008.01 | |
| Drufomat scan | DREVE | DV3300 | |
| GraphPad Prism 9 | GraphPad | 9 | |
| Mimics software | Materialise | 21 | |
| PROLENE Monofilament polypropylene suture 5-0 | Johnson & Johnson | W8310 | |
| Straumann Dental Implant System | Straumann | 021.3312 | |
| Straumann Surgical Toolbox | Straumann | 040.165 | |
| Temporary crown and bridge material automix system | Coltene | 170152-202 | |
| Thermo-forming foils and plates | DREVE | 20172636510 |
References
- Linkow, L., Iyer, S., Piermatti, J. The world's longest functioning implant: A verified case report. J Oral Implantol. 49 (3), 278-278 (2023).
- Zhou, T., Mirchandani, B., Li, X. X., Mekcha, P., Buranawat, B. Quantitative parameters of digital occlusal analysis in dental implant supported restorative reconstruction recent 5 years: A systematic review. Acta Odontol Scand. 81 (1), 1-17 (2023).
- Schropp, L., Wenzel, A., Kostopoulos, L., Karring, T. Bone healing and soft tissure contour changes following single tooth extraction : A clinical and radiographic 12-monhts prospective study. Int J Periodontics Restorative Dent. 23 (4), 313-323 (2003).
- Chiapasco, M., Romeo, E., Casentini, P., Rimondini, L. Alveolar distraction osteogenesis vs. Vertical guided bone regeneration for the correction of vertically deficient edentulous ridges: A 1-3-year prospective study on humans. Clin Oral Implants Res. 15 (1), 82-95 (2010).
- Danesh-Sani, S. A., Loomer, P. M., Wallace, S. S. A comprehensive clinical review of maxillary sinus floor elevation: Anatomy, techniques, biomaterials and complications seyed amir danesh-sani. Br J Oral Maxillofac Surg. 54 (7), 724-730 (2016).
- Noelken, R. -., Al-Nawas, B. Bone regeneration as treatment of peri-implant disease: A narrative review. Clin Implant Dent Relat Res. 25 (4), 696-704 (2023).
- Schwartz-Arad, D., Levin, L. Intraoral autogenous block onlay bone grafting for extensive reconstruction of atrophic maxillary alveolar ridges. J Periodontol. 76 (4), 636-641 (2005).
- Peleg, M. Lateral alveolar ridge augmentation with allogenic block grafts: Observations from a multicenter prospective clinical trial. J Oral Maxillofac Surg. 63, 29-29 (2005).
- Qinghua, L. I., et al. Ct measurement of palatal as a bone-supply area in oral implanting surgery. Chinese J Med Imag. 21 (9), 697-700 (2013).
- Chung, C. H., Font, B. Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 126 (5), 569-575 (2004).
- Shuang, F., et al. Accuracy and patient-centered results of static and dynamic computer-assisted implant surgery in edentulous jaws: A retrospective cohort study. Clinical oral investigations. (9), 27 (2023).
- Jinno, Y., et al. Vertical bone augmentation using ring technique with three different materials in the sheep mandible bone. Int J Oral Maxillofac Implants. 33 (5), 1057-1063 (2018).
- Ragab Mahmoud, A. E., Mohammad Yassin, S., Ali Hassan, S., Sayed Abdelmoneim, H. Vertical alveolar bone augmentation of atrophied posterior mandibular regions with simultaneous dental implant placement using allogeneic bone rings vs autogenous bone rings: A randomized controlled clinical trial. Quintessence Int. 55 (3), 232-243 (2024).
- Zou, W., et al. A comparative study of autogenous, allograft and artificial bone substitutes on bone regeneration and immunotoxicity in rat femur defect model. Regen Biomater. 8 (1), (2021).
- Zufia, J., Abella Sans, F. Applications of maxillary tuberosity block autograft. J Esthet Restor Dent. 34 (7), 1015-1028 (2022).
- Zhuang, X. D., Chen, W. X., Mao, C. Q., Xu, Q. J., Chen, W. H. Morphological classification of mandible posterior region based on cone beam ct images. Zhonghua Kou Qiang Yi Xue Za Zhi. 53 (7), 443-447 (2018).
- Yuan, S., et al. Comparison of in-situ bone ring technique and tent-pole technique for horizontally deficient alveolar ridge in the anterior maxilla. Clin Implant Dent Relat Res. 22 (2), 167-176 (2020).
- Starch-Jensen, T., Deluiz, D., Deb, S., Bruun, N. H., Tinoco, E. M. B. Harvesting of autogenous bone graft from the ascending mandibular ramus compared with the chin region: A systematic review and meta-analysis focusing on complications and donor site morbidity. J Oral Maxillofac Res. 11 (3), 1 (2020).
- Schwartz-Arad, D., Levin, L. Multitier technique for bone augmentation using intraoral autogenous bone blocks. Implant Dentistry. 16 (1), 5-12 (2007).
- Berkovitz, B. K. B., Holland, G. R., Moxham, B. J. . Oral anatomy, histology and embryology. , (2002).
- Sáez-Alcaide, L. M., et al. Effectiveness of the bone ring technique and simultaneous implant placement for vertical ridge augmentation: A systematic review. Int J Implant Dent. 6 (1), 82 (2020).
- Rodriguez-Recio, O., Rodriguez-Recio, C., Gallego, L., Junquera, L. Computed tomography and computer-aided design for locating available palatal bone for grafting: two case reports. Int J Oral Maxillofac Implants. 25 (1), 197-200 (2010).
- Block, M. S., Emery, R. W., Cullum, D. R., Sheikh, A. Implant placement is more accurate using dynamic navigation. J Oral Maxillofac Surg. 75 (7), 1377-1386 (2020).
- D'haese, J., Ackhurst, J., Wismeijer, D., De Bruyn, H., Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontol. 73 (1), 121-133 (2016).
- Kaewsiri, D., Panmekiate, S., Subbalekha, K., Mattheos, N., Pimkhaokham, A. The accuracy of static vs dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin Oral Implants Res. 30 (6), 505-514 (2019).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved