Method Article
Sensor Assessment of Gap Balance in Mobile-Bearing Unicompartmental Knee Arthroplasty
* Questi autori hanno contribuito in egual misura
In questo articolo
Riepilogo
Here, we present a protocol to measure the gap contact force and gap balance in mobile-bearing unicompartmental knee arthroplasty (UKA). Along with the clinical and radiographic data, we hope to determine the normal range of the contact force and set up the threshold of the gap balance.
Abstract
The most important procedure of mobile-bearing unicompartmental knee arthroplasty (UKA) is to balance the knee flexion and extension gap. Conventionally, the balance was determined by the subjective assessment of plugging out the feeling gauge. Since it mainly depended on the surgeons' experience, the accuracy was always in doubt. In the past 10 years, pressure sensors have been introduced to guide the gap balance in total knee arthroplasty (TKA). However, the sensor technique was introduced to UKA very recently. Herein is our sensor assessment of the gap balance in 20 cases UKA by one experienced surgeon. The sensor was a custom-designed force sensor matrix according to the shape of the tibial trial of mobile-bearing UKA. The postoperative clinical outcomes and radiographic results were recorded for future comparison. We aim to use this method to assess more than 200 cases of UKA by various surgeons to ultimately standardize the gap-balance result.
Introduzione
The mobile-bearing UKA is currently one of the most successful treating methods for anteromedial osteoarthritis (AMOA) of the knee1. The balance of the flexion and extension gap during the operation is the key to a successful UKA2,3. The gap overload might aggravate the wear of the mobile bearing. Moreover, the elevated gap contact force might lead to postoperative valgus deformity and degeneration of the lateral compartment4. Therefore, achieving an optimal gap tightness as well as an acceptable gap balance in UKA is an important part of the learning curve5. According to the mobile-bearing UKA manual of surgical technique6, the surgeon must use the feeling gauge to insert and plug out of the joint gap to "feel" the contact force. By evaluating the force required to insert and remove the insert, the surgeon could estimate whether the gap balance is acceptable. Therefore, the judgment depended mainly on the surgeon's experience.
In recent years, digital measurement of intraoperative gap balance of medial and lateral gap had been widely reported in total knee arthroplasty (TKA)7,8,9. Recommendations for the threshold of the gap balance had also been set7. However, the sensor technique was introduced to UKA very recently without a well-recognized gap-balancing goal.
Last year, a force sensor specially designed to measure joint gap contact force during mobile-bearing UKA was introduced5. In the present research protocol, the sensor-guided gap force measurement method is demonstrated. In addition, a case series of 20 patients who had undertaken mobile-bearing UKA is included to assess the gap contact force and the gap balance. The final goal of this protocol is to determine the normal range of contact force and set up the threshold of gap balance in mobile-bearing UKA.
Protocollo
This study was approved by the human ethics committee of the China-Japan Friendship Hospital (approval number 2020-50-k28).
1. Preparation and sterilization of the force sensor
- Use abrasion-resistant adhesive tape to fix the force sensor on the upper surface of the tibial trial before sterilization.
- Pack and sterilize the force sensor using low-temperature sterilization with hydrogen peroxide gas plasma (Figure 1).
NOTE: The sensor should be fixed on the tibial trial to prevent the effect of the shear force.
2. Procedure of mobile-bearing UKA
- Perform the operation procedure of mobile-bearing UKA according to the standard surgical instruction6 or the kinematic alignment technique introduced by Zhang et al.10.
- Stop the procedure when all the bone cuttings are finished, and the gap balance is confirmed manually.
3. Installation of the force sensor
- Install the force sensor along with the tibial trail first, and then install the femoral component.
- Ensure the sensor, the USB line, and the laptop are connected properly. After that, insert the feeler gauge into the component gap, and place the knee joint at deep flexion of 120° as the start point of the measurement. (Figure 2).
NOTE: Use a sterilized protractor to make sure the accuracy of the knee flexion angle.
4. Measurement and recording of raw data of the contact force
- Record raw data of the force value using a computer program developed for this sensor.
- First, pay attention to the right side of the operation interface (Figure 3), and set up the recording frequency at 10 Hz and the recording time at 5 s. Then, click on the Data Feedback button when the knee is placed at the flexion angle of 120°.
- When the recording process is over, click on the Data Feedback button again when the knee flexion is 90°, then 60°, 45°, 20°, and 0° (Figure 3).
NOTE: Raw data is saved into .txt files by the computer program, and further management is needed to acquire force value.
5. Management of raw data
- Input the .txt file into a spreadsheet (digital table) for raw data conversion. Compute the average value of 50 records as the contact force.
NOTE: The program can also show the distribution of the contact force.
6. Clinical and radiographic observations
- Record the patient's demographic data such as age, gender, diagnosis, and the American Knee Society score (AKSS).
- Take radiographs of anteroposterior, lateral, and full-length weight-bearing lower limb preoperatively and within 1 week postoperatively.
- Measure the varus/valgus alignment of the femoral and tibial prosthesis (Figure 4-1), the flexion/extension alignment of the femoral prosthesis, and the tibial posterior slope (Figure 4-2).
- Measure the hip-knee-ankle angle on the full-length lower limb radiographs both preoperatively and postoperatively. Measure the continuity of the prosthesis (Figure 4-3) and the convergence/divergence angle, which implies the axis of the femoral prosthesis relative to the surface of the tibial prosthesis (Figure 4-4).
- Make sure these data are integrated and can be analyzed in the future.
NOTE: The method of the radiographic measurement of the angles6,11 are shown in Figure 4.
Risultati
Cohort demographics
The first 20 patients who undertook mobile-bearing UKA were enrolled in the China-Japan Friendship Hospital from March to June 2021. The surgeries were all done by a senior doctor with over 2,000 cases of UKA experience. The demographic along with prothesis data is shown in Table 1. The age ranged from 58-82 years, and the diagnoses were all AMOA.
Results of gap force and balance measurements
The pattern of gap force is shown in Figure 5. The average contact force of knee flexion at 0°, 20°, 45°, 60°, 90°, and 120° was 70.3 N, 96.9 N, 116.1 N, 95.1 N, 73.6 N, and 58.3 N, respectively. The mean gap balance was 23.2 N by calculating the force of 20° (extension gap) minus 90° (flexion gap). Results are shown in Table 2.
Results of clinical and radiographic assessments
In terms of the clinical outcome, the American Knee Society score (AKSS) was used, which comprised two parts: the objective score (the American Knee Society Objective score, AKSS-O) and the functional score (the American Knee Society Functional score, AKSS-F), with a maximum score of 100. The assessments were done at 6 months and 1 year postoperatively. A long-term follow-up would be taken at the end of the whole research, which would be in 2023, approximately. In the first 20 cases, the mean postoperative AKSS-O and AKSS-F were 87.2 and 90.0, respectively. In the radiographic assessment, the postoperative femoral and tibial prosthesis varus and valgus angles, femoral prosthesis flexion and extension angles, tibial slope, convergence angle of the prosthesis, and contiguity between the femoral and tibial prosthesis are shown in Table 3.
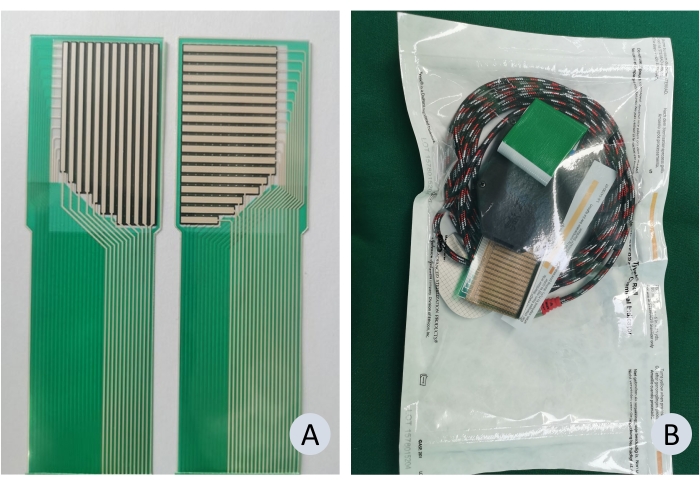
Figure 1: Preparation and sterilization of the force sensor. (A) The appearance of the force sensor; (B) The force sensor device after sterilization. Please click here to view a larger version of this figure.
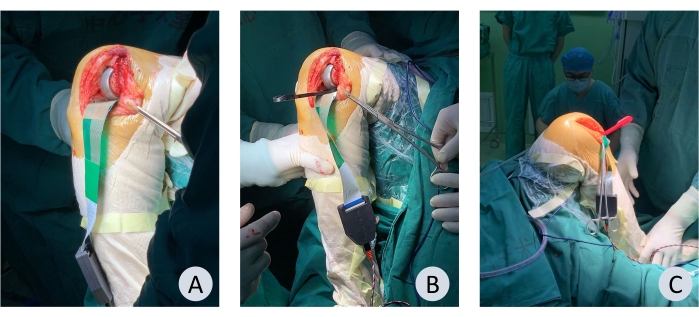
Figure 2: The contact force measurement of joint gaps in mobile-bearing UKA. (A) Installation of the sensor without the feeler gauge. (B) Insertion of the feeler gauge and the measurement of contact force. (C) The operator should be at least 2 m away from the surgical table. Please click here to view a larger version of this figure.
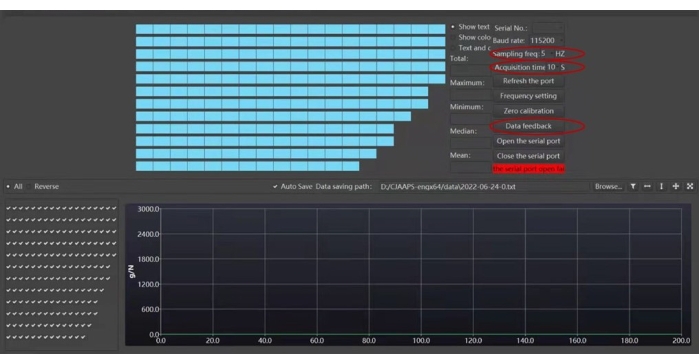
Figure 3: The interface of the computer program. The recording frequency should be set at 10 Hz, and the time should be set at 5 s. Please click here to view a larger version of this figure.

Figure 4: Radiographic measurements (A) Angle a: femoral varus/valgus angle. Angle c: tibial varus/valgus angle. (B) Angle b: femoral flexion/extension angle. Angle d: tibial slope. (C) Contiguity between the lateral margin of the femoral component and lateral wall of the tibial component. (D) Convergence/divergence angle of the femoral component relative to the tibial component. Please click here to view a larger version of this figure.
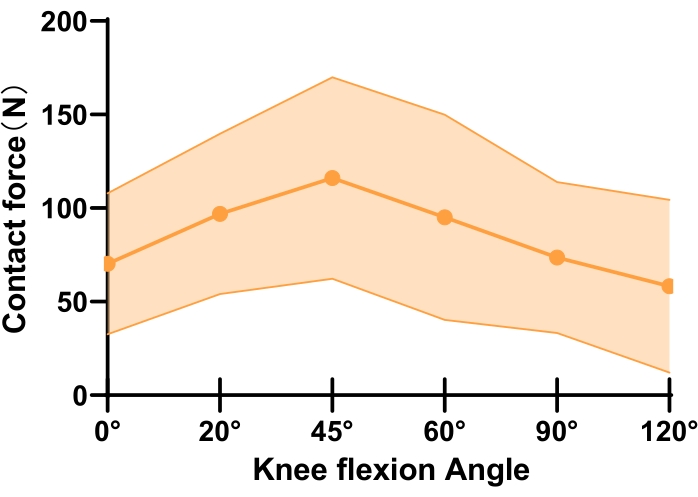
Figure 5: Contact force vs. knee flexion angle. The figure shows the component gap contact force pattern at different knee flexion angles. Please click here to view a larger version of this figure.
Table 1: The demographic data of patients included and the UKA prosthesis size. Please click here to download this Table.
Table 2: The results of gap forces and balance (in Newtons) in 20 cases of UKA surgeries. Please click here to download this Table.
Table 3: The results of clinical outcomes and radiographic measurements. Please click here to download this Table.
Discussione
This study provided a detailed protocol of sensor technology in assessing the joint gap contact force and balance in mobile-bearing UKA. We hope to set up a goal of standard contact force as well as gap-balancing difference, which would allow the orthopedic surgeons to determine the bearing thickness and gap-balancing more easily in the future.
The overload of the joint gap may lead to postoperative valgus deformity of the limb, future degeneration of the lateral compartment, and even OA progression, which was considered the most common reason for revision of UKA4,12. However, a too loose joint gap could not prevent the mobile bearing from dislocation, leading to postoperative complications. The bearing thickness was conventionally determined by the surgeon's experience of gap contact force without an objective goal to refer to5. The sensor technology was very successful in TKA for its convenient use and direct reading of the force value7,13. Sensor-guided TKA was considered to have better clinical outcomes than conventional procedure13. Furthermore, this technique was very friendly to less experienced surgeons and could shorten the learning curve of TKA8. However, the research on the usage of sensor techniques in UKA was still in the primary stage. Su et al. developed a tibial trial model based on pressure sensing technology to measure the trajectory of the mobile bearing14. Jaeger et al. designed a sensor in the same shape as the feeling gauge to measure the osmotic pressure of bone cement15. Ettinger et al. used a flexible sensor matrixto measure and compare the gap contact force between the mobile-bearing and the fixed-bearing UKA, but did not report the actual value or the recommended threshold16. In fact, there was still no commercialized force sensor for UKA, and this field was very worthy of being explored.
A novel force sensor for mobile-bearing UKA was designed according to the shape of the tibial trial of mobile-bearing UKA. The sensing area was 45 x 22 mm2, with a total of 197 force measuring points, the maximum data collection frequency was 20 Hz, and the range was up to 500 N/cm2. The accuracy and repeatability of the sensor were confirmed in a recently published research5. In this research protocol, we applied the same calibration method to convert the raw data stored in .txt files to actual contact force value5,17, and then restored the data in a digital table.
Since the sensor was developed for mobile-bearing UKA, the shear force was the major risk factor of failure in the measurement. We use an abrasion-resistant adhesive tape to fix the force sensor on the upper surface of the tibial trial to reduce the relative movement between the sensor and the trial. Moreover, the tape was only 0.1 mm thick; it had only limited affection of the force measurement bias, which could be ignored.
The gap-balancing of UKA was a big challenge for orthopedic surgeons. As the design of the Oxford unicompartmental prosthesis was similar in structure and function to that of the knee, the surgical technique was an important factor affecting clinical outcome1,11, with the flexion-extension gap-balance considered the most important factor2,18. The standard procedure in performing UKA was resecting the medial part of the tibia platform before resecting the posterior femoral condyle to obtain the flexion gap. The anterior surface of the medial condyle was then milled to balance the extension gap. According to the principle of UKA, no soft tissue release is allowed for balance. Therefore, UKA poses a higher request of skills to the surgeons. If the surgical experience is not enough, the surgeons may make mistakes in estimating the gap balance. The novel UKA force sensor could be used to evaluate knee flexion-extension gap balance; therefore, it could help surgeons to judge the gap balance more efficiently, thereby shortening the UKA learning curve.
A Difference within 67 N between the medial and lateral joint gap was considered balanced in TKA7,19,20. However, there is no established gap balance threshold in UKA. In this research stage, the average gap balance is 23.2 ± 26.1 N, much smaller than that of sensor-guided TKA. There might be a much more strict threshold of gap balance in UKA. In fact, the practical standard should be based on a large sample size of clinical results of UKA with contact force measurement. In this research protocol, totally three senior surgeons with a case-load of over 1,000 UKAs from three independent medical centers were invited. The scheme was to include over 200 UKAs with integrated gap force data, clinical records, and radiographs to accomplish the original goal.
Our study also has certain limitations. First, the sensor needs to be independently installed on the test mold; this will increase about 5 min of the surgical time. For further commercial development, the design should integrate the sensor and the test mold together. Another thing is that the study is just in the initial stage, so the sample size is still limited, and more data is required to establish a detailed and convincing criteria to estimate the gap balance.
Divulgazioni
Since the computer program and the digital table equations are protected by the patent law, authors could be contacted for this information. The authors declare that they have no competing interests.
Riconoscimenti
This work was supported by the Capital Health Research and Development of Special (grant number 2020-2-4067), Beijing Natural Science Foundation (grant number 7202183); National Natural Science Foundation of China (grant numbers 81972130, 81902203, and 82072494), and Elite Medical Professionals project of China-Japan Friendship Hospital (NO.ZRJY2021-GG08). Since the computer program and the digital table equations are protected by the patent law, authors could be contacted for this information.
Materiali
| Name | Company | Catalog Number | Comments |
| Oxford UKA | Zimmer/Biomet | For the catalog numbers refer to Oxford Partial Knee Microplasty Instrumentation (femoral component, tibial component, meniscus bearing) | |
| Teflon Tape | 3M | Abrasion resistant adhesive tape widely used in biomechanical experiments | |
| Verasense | OrthoSensor | Verasense | TKA sensor |
| Excel | Microsoft | digital table software | |
| STERRAD 100S sterilization system | Johnson&Johnson | STERRAD 100S | Low-temperature sterilizing with hydrogen peroxide gas plasma |
| UKA force sensor | Qingrui Boyuan | in house | Co-designed and produced by Qingrui Boyuan Technology |
| Computer program for recording raw data | Qingrui Boyuan | in house | Co-designed and produced by Qingrui Boyuan Technology |
| Protractor | Shanghai M&G Stationery Inc. | any | Sterilized in the sterilization system |
| USB line | Lenovo | any | |
| Laptop | Lenovo | any basic configuration |
Riferimenti
- Mohammad, H. R., Matharu, G. S., Judge, A., Murray, D. W. New surgical instrumentation reduces the revision rate of unicompartmental knee replacement: A propensity score matched comparison of 15,906 knees from the National Joint Registry. Knee. 27 (3), 993-1002 (2020).
- Bae, J. H., et al. Epidemiology of bearing dislocations after mobile-bearing unicompartmental knee arthroplasty: Multicenter analysis of 67 bearing dislocations. Journal of Arthroplasty. 35 (1), 265-271 (2020).
- Sun, X., et al. Bearing dislocation of mobile bearing unicompartmental knee arthroplasty in East Asian countries: a systematic review with meta-analysis. Journal of Orthopaedic Surgery and Research. 16 (1), 28 (2021).
- Ro, K. H., Heo, J. W., Lee, D. H. Bearing dislocation and progression of osteoarthritis after mobile-bearing unicompartmental knee arthroplasty vary between Asian and Western patients: A meta-analysis. Clinical Orthopaedics and Related Research. 476 (5), 946-960 (2018).
- Sun, X., et al. Sensor and machine learning-based assessment of gap balancing in cadaveric unicompartmental knee arthroplasty surgical training. International Orthopaedics. 45 (11), 2843-2849 (2021).
- Oxford Partial Knee microplasty instrumentation manual of the Surgical Technique. Zimmer-Biomet Available from: https://www.zimmerbiomet.com/content/dam/zimmer-biomet/medical-professionals/000-surgical-techniques/knee/oxford-partial-knee-microplasty-instrumentation-surgical-technique.pdf (2019)
- Gustke, K. A., Golladay, G. J., Roche, M. W., Elson, L. C., Anderson, C. R. A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. Journal of Arthroplasty. 29 (5), 955-960 (2014).
- Lakra, A., et al. The learning curve by operative time for soft tissue balancing in total knee arthroplasty using electronic sensor technology. Journal of Arthroplasty. 34 (3), 483-487 (2019).
- MacDessi, S. J., et al. Does soft tissue balancing using intraoperative pressure sensors improve clinical outcomes in total knee arthroplasty? A protocol of a multicentre randomised controlled trial. BMJ Open. 9 (5), 027812 (2019).
- Zhang, Q., et al. A novel extramedullary technique to guide femoral bone preparation in mobile unicompartmental knee arthroplasty based on tibial cut and overall alignment. Journal of Orthopaedic Surgery and Research. 15 (1), 92 (2020).
- Hurst, J. M., Berend, K. R., Adams, J. B., Lombardi, A. V. Radiographic comparison of mobile-bearing partial knee single-peg versus twin-peg design. Journal of Arthroplasty. 30 (3), 475-478 (2015).
- vander List, J. P., Zuiderbaan, H. A., Pearle, A. D. Why do medial unicompartmental knee arthroplasties fail today. Journal of Arthroplasty. 31 (5), 1016-1021 (2016).
- MacDessi, S. J., Gharaibeh, M. A., Harris, I. A. How accurately can soft tissue balance be determined in total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 34 (2), 290-294 (2019).
- Su, Z., Wang, Z., Chen, H. A force line trajectory measuring system and algorithms for unicondylar knee replacement surgery. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. , 2217-2221 (2019).
- Jaeger, S., et al. The influence of the femoral force application point on tibial cementing pressure in cemented UKA: an experimental study. Archives of Orthopaedic and Trauma Surgery. 132 (11), 1589-1594 (2012).
- Ettinger, M., et al. In vitro kinematics of fixed versus mobile bearing in unicondylar knee arthroplasty. Archives of Orthopaedic and Trauma Surgery. 135 (6), 871-877 (2015).
- Brimacombe, J. M., Wilson, D. R., Hodgson, A. J., Ho, K. C., Anglin, C. Effect of calibration method on Tekscan sensor accuracy. Journal of Biomechanical Engineering. 131 (3), 034503 (2009).
- Heyse, T. J., et al. Balancing mobile-bearing unicondylar knee arthroplasty in vitro. Knee Surgery, Sports Traumatology, Arthroscopy. 25 (12), 3733-3740 (2017).
- Gustke, K. A., Golladay, G. J., Roche, M. W., Elson, L. C., Anderson, C. R. Primary TKA patients with quantifiably balanced soft-tissue achieve significant clinical gains sooner than unbalanced patients. Advances in Orthopedics. 2014, 628695 (2014).
- Nodzo, S. R., Franceschini, V., Gonzalez Della Valle, A. Intraoperative load-sensing variability during cemented, posterior-stabilized total knee arthroplasty. Journal of Arthroplasty. 32 (1), 66-70 (2017).
Ristampe e Autorizzazioni
Richiedi autorizzazione per utilizzare il testo o le figure di questo articolo JoVE
Richiedi AutorizzazioneThis article has been published
Video Coming Soon