Method Article
Extraperitoneal Laparoscopic Modified Y-V Plasty for the Treatment of Refractory Bladder Neck Contracture
Dans cet article
Résumé
Here, we describe a modified surgical procedure for refractory bladder neck contracture that is associated with easy manipulation, optimum intraoperative exposure, and minimal invasiveness.
Résumé
Bladder neck contracture (BNC) is a rare, late complication of transurethral resection of the prostate (TURP). Although the endoscopic procedure is the primary treatment for BNC, the recurrence rate remains high. Y-V plasty offers excellent surgical results for those individuals with refractory and recurrent BNC. Traditional open operations usually fail to provide satisfactory exposure to the operating field and lead to greater invasiveness. Interrupted sutures lead to prolonged operative time and increased anastomotic leakage. Laparoscopic modified Y-V plasty is performed through extraperitoneal access to the pelvis, which provides adequate exposure to the surgical view and avoids intra-abdominal injury. After incising the anterior bladder wall neck in a Y-shaped fashion, anastomosis is performed using two absorbable barbed sutures. The mucosa and submucosa layer of the bladder is closed to both sides with consecutive sutures in a V-shape before suturing serosa, and tunica muscularis are sutured to reinforce. The aforementioned procedures reduce leakage from the anastomosis and decrease operative time and patient trauma. Extraperitoneal laparoscopic modified Y-V plasty offers significant advantages over the open approach in terms of post-surgical recovery and invasiveness, making it a feasible and safe surgical option for patients with refractory BNC.
Introduction
Transurethral resection of the prostate (TURP) remains the gold standard for the surgical treatment of benign prostatic hyperplasia (BPH)1. Bladder neck contracture (BNC) is a common late complication of TURP, affecting 0.3% to 15.4% of patients2,3. The mechanism and etiology of BNC occurrence are not yet fully understood. Risk factors include small glands, excessive resection of the bladder neck, robust fulguration, and hypertrophic scarring from extensive resection4. The endoscopic procedure is usually the treatment of choice for BNC; however, the failure rate is as high as 14%-28%4. Patients are considered refractory to BNC if stricture recurrence occurs after two or more failed endoscopic treatments5.
Reconstructive surgery of the bladder neck is considered an effective treatment for patients with refractory BNC. Young was the first to describe an open Y-V plasty of the bladder neck, which replaced the sclerotic bladder neck with a healthy bladder6. However, open surgery rarely provides satisfactory exposure to the operative field and causes greater invasiveness. The application of laparoscopy and robots reduces the difficulty and trauma of the procedure. Success rates of 87.5%, 92.6%, and 83.3%-100% are reported for open, laparoscopic, and robotic surgery, respectively5,7,8,9.
In this study, we introduced an extraperitoneal laparoscopic modified Y-V plasty for the treatment of refractory BNC. The procedure is performed through an anterior extraperitoneal approach, and the bladder incision is closed with two continuously running barbed sutures. This new approach provides an adequate surgical field of view and reduces the invasiveness of the procedure compared to the conventional approach. In addition to that, the procedure can also reduce leakage from the anastomosis and decrease operative time.
Protocole
All the procedures in the following protocol were reviewed and approved by the Shandong Provincial Hospital ethics committee.
1. Patient selection and preparation
- Inclusion criteria: Include patients having: lower urinary tract obstruction; urethrogram or cystoscopy suggestive of BNC; history of at least two unsuccessful transurethral procedures.
- Exclusion criteria: Exclude patients with: suspected malignancy; acute systemic inflammation or pelvic inflammatory disease; severe coagulation disorders; any other contraindications for general anesthesia or laparoscopy.
- Inform all patients about the surgical option with its expected outcomes and potential risks, and obtain written informed consent.
- Perform the procedure under general endotracheal anesthesia. Administer prophylactic antibiotics intravenously 1 h before surgery.
2. Establish pneumoperitoneum
- Place the patient in the recumbent position. Make a 3 cm vertical incision at the lower umbilicus edge.
- Perform a blunt separation to reveal extraperitoneal space between rectus abdominis and posterior sheath of rectus abdominis. Then, perform balloon dilatation to improve operative field exposure.
- Insert a 10 mm trocar into the vertical incision. Then, place the camera and establish pneumoperitoneum.
- Place two 12 mm trocars on both sides 2 cm below the navel, and two 5 mm trocars on bilateral McBurney's point (Figure 1).
3. Modified Y-V plasty
- Clear the fat around the surface of the bladder neck and prostate to expose their junction.
- Make a Y-shaped incision at the anterior wall and neck of the bladder at the junction of prostate and bladder with an ultrasonic knife.
- Then cut the narrow segment fully (i. e., cut the scar tissue completely until the normal bladder mucosa is observed) (Figure 2A).
- Insert a 20F silicone catheter slowly, and check whether the urinary tract is probed for patency. If there is resistance when passing through the bladder neck, the narrow segment may need to be incised again (Figure 2B).
- Perform a V-shaped anastomosis with two 2-0 absorbable barbed sutures. Suture the lowest point of bladder flap and normal mucosa.
- Then, close the mucosa and submucosa layer with a tensionless continuous suture on the left side of the bladder. Perform the same procedure on the other side (Figure 2C).
- Tighten both sutures simultaneously. Then, suture serosa and tunica muscularis for reinforcement (Figure 2D). Knot the two sutures at the 12 o'clock position.
- Indwell a pelvic drainage tube and remove the trocars after the abdomen is deflated. Close the skin with an interrupted suture.
4. Postoperative management
- Monitor the color and volume of urine and drainage fluid. Remove the drainage tube 1-2 days after surgery, and remove the urinary catheter 2 weeks after surgery.
- Follow up postoperatively at 3 months, 6 months, 1 year, and annually thereafter. The follow-ups include the international prostate symptom score (IPSS), maximum urine flow rate (Qmax; mL/s), urethrography, urethroscopy, and ultrasound.
Résultats
Five patients were included in the study with a mean age of 66.2 years (range, 62-75 years) who had undergone at least two unsuccessful transurethral procedures. All patients completed the surgery successfully with no open surgeries. There were no significant intraoperative or postoperative complications. Preoperative Qmax was 5.48 mL/s (range, 3.7-4.9 mL/s) and the IPSS score was 22.6 (range, 17-29). The average operation time, blood loss, and postoperative stay were 104 min (range, 90-130 min), 74 mL (range, 60-100 mL), and 6.8 days (range, 6-8 days). The postoperative assessment was undertaken at about 1 month and latest follow-up, and the mean follow-up time was 24 months (range, 19-30 months). All patients were evaluated by IPSS score, urodynamics, and urethroscopy. Mean postoperative Qmax reached 24.7 (range, 19.1-30.7), and the IPSS score was 3.2 (range, 2-5). Cystoscopy showed that the lower urinary tract was unobstructed. Up to now, there have been no recurrent cases (Figure 3 and Table 1).
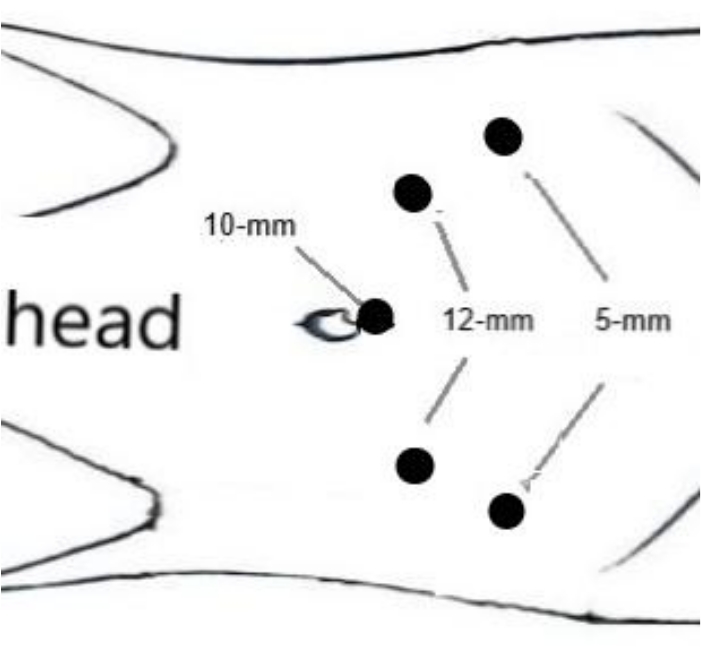
Figure 1: Five-port extraperitoneal approach. Please click here to view a larger version of this figure.

Figure 2: Schematic diagram of extraperitoneal laparoscopic modified Y-V plasty. (A) Make a Y-shaped incision at the anterior wall and neck of bladder. (B) Insert a 20F silicone catheter slowly, and check whether the urinary tract is probed for patency. (C) Continuously suture the mucosa and submucosa layer in a V shape. (D) Suture serosa and tunica muscularis for reinforcement. Please click here to view a larger version of this figure.
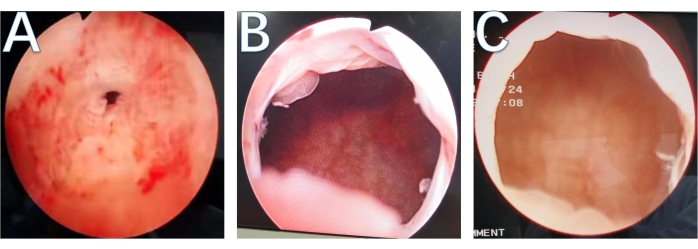
Figure 3: Follow up with urethroscopy. (A) Preoperative urethroscopy. (B) Urethroscopy 3 months after operation. (C) Urethroscopy 6 months after operation. Please click here to view a larger version of this figure.
| Patients | Age(years) | Pre-operative IPSS | Pre-operative Qmax (mL/s) | Operation time (min) | Blood loss (mL) | Post-operative hospital stay (days) | Post-operative IPSS | Post-operative Qmax (mL/s) | Follow-up (months) | Recurrence |
| 1 | 62 | 25 | 4.2 | 105 | 70 | 7 | 4 | 21.8 | 23 | No |
| 2 | 63 | 20 | 5.8 | 100 | 80 | 7 | 3 | 23.5 | 20 | No |
| 3 | 75 | 22 | 5.8 | 95 | 60 | 6 | 5 | 19.1 | 19 | No |
| 4 | 63 | 29 | 3.7 | 130 | 100 | 6 | 2 | 28.6 | 28 | No |
| 5 | 68 | 17 | 7.9 | 90 | 60 | 8 | 2 | 30.7 | 30 | No |
Table 1: Characteristics and perioperative outcomes of patients who underwent extraperitoneal laparoscopic modified Y-V plasty.
Discussion
BNC has long puzzled patients and urologists as a complication of prostate manipulation. The patient often presents varying degrees of symptoms of lower urinary tract obstruction or urinary retention5. Many patients who undergo initial treatment for BNC achieve early success, but a significant proportion of patients experience recurrent obstruction10. After exhausting endoscopic means and dilatation techniques to treat recalcitrant BNC, surgical repair is considered an effective treatment option11. The Y-V plasty is one of the most widely used techniques for bladder neck reconstruction, providing a high success rate by reconstructing a wide re-anastomosis through a healthy tissue flap12. However, due to the relatively narrow retropubic space, open surgery usually does not provide an adequate surgical area and can be more invasive.
Compared with open Y-V plasty, the modified techniques are more advantageous in minimally invasive, operative field view, and anastomosis. Access to the pelvis from outside the extra peritoneum allows full exposure to the surgical field and avoids intra-abdominal injury. Laparoscopy provides a high-definition close view, which allows clear observation of the stenosis in the neck of the bladder. By properly adjusting the use of the urinary catheter, a urologist can cut the narrow segment fully and avoid damaging the urethral sphincter. During closure, both sutures are tightened simultaneously after the mucosal and submucosal layers on both sides have been closed. Special attention should also be paid to tension-free suturing; in this way, the anastomotic suture is more regular and smoother, which is conducive to wound healing, and reduces scar hyperplasia. Besides, tight anastomosis is noticed, and the number of knots is decreased. Therefore, the operation time and anastomotic leakage are reduced. Our findings suggest that it is a feasible and safe surgical option for patients with refractory BNC, and those patients are more willing to accept this minimally invasive surgery.
In recent years, satisfactory results have been reported in the literature for different modified surgical techniques based on Y-V plasty (e.g., T-plasty)13, but no previous studies analyzed the statistical differences between surgical procedures. Compared to traditional laparoscopy, robots have more advantages in accurate dexterity8. However, high prices and poor popularity may be limiting factors for robots.
The small number of patients and inadequate follow-up are the main limitations of this study. We will acquire more available clinical data and a longer follow-up period to validate the results.
In summary, this extraperitoneal laparoscopic modified Y-V plasty is a safe and effective, minimally invasive treatment for refractory BNC compared to traditional treatment. The surgical procedure offers significant advantages in easy manipulation, good exposure, minimal invasiveness, and bladder incision suture.
Déclarations de divulgation
The authors have nothing to disclose.
Remerciements
None.
matériels
| Name | Company | Catalog Number | Comments |
| 2-0 V-Loc 180 | Covidien | A1F0606VY | 2-0 absorbable barbed sutures |
| 20F silicone catheter | CREATE MEDIC | D19111322 | A disposable Foley Catheter |
| HARMONIC ACE Ultrasonic Surgical Devices | Johnson & Johnson | V95V2N | It is suitable for controlling bleeding and minimizing thermal damage as needed during soft tissue incision |
| Laparoscopic system | Olympus | 20172220119 | Provide HD images |
| Laproscopic trocar | Anhui Aofo Medical Equipment Tech Corporation | 20202020172 | Disposable laproscopic trocar |
Références
- Mayer, E. K., Kroeze, S. G., Chopra, S., Bottle, A., Patel, A. Examining the 'gold standard': a comparative critical analysis of three consecutive decades of monopolar transurethral resection of the prostate (TURP) outcomes. BJU International. 110 (11), 1595-1601 (2012).
- Rassweiler, J., Teber, D., Kuntz, R., Hofmann, R. Complications of transurethral resection of the prostate (TURP)-incidence, management, and prevention. European Urology. 50 (5), 969-980 (2006).
- Castellani, D., et al. Bladder neck stenosis after transurethral prostate surgery: a systematic review and meta-analysis. World Journal of Urology. 39 (11), 4073-4083 (2021).
- Primiceri, G., Castellan, P., Marchioni, M., Schips, L., Cindolo, L. Bladder neck contracture after endoscopic surgery for benign prostatic obstruction: Incidence, treatment, and outcomes. Current Urology Reports. 18 (10), 79 (2017).
- Sayedahmed, K., El Shazly, M., Olianas, R., Kaftan, B., Omar, M. The outcome of Y-V plasty as a final option in patients with recurrent bladder neck sclerosis following failed endoscopic treatment. Central European. Journal of Urology. 72 (4), 408-412 (2019).
- Young, B. W. The retropubic approach to vesical neck obstruction in children. Surgery, Gynecology & Obstetrics. 96 (2), 150-154 (1953).
- Liu, Z., Huang, G., Zhou, N., Man, L. Modified cystoscopy-assisted laparoscopic Y-V plasty for recalcitrant bladder neck contracture. Minimally Invasive Therapy & Allied Technologies. 31 (2), 185-190 (2022).
- Much, M., et al. Robot-assisted laparoscopic Y-V plasty in 12 patients with refractory bladder neck contracture. Journal of Robotic Surgery. 12 (1), 139-145 (2018).
- Granieri, M. A., Weinberg, A. C., Sun, J. Y., Stifleman, M. D., Zhao, L. C. Robotic Y-V plasty for recalcitrant bladder neck contracture. Urology. 117, 163-165 (2018).
- Ramirez, D., Simhan, J., Hudak, S. J., Morey, A. F. Standardized approach for the treatment of refractory bladder neck contractures. Urologic Clinics of North America. 40 (3), 371-380 (2013).
- Breyer, B. N., McAninch, J. W. Management of recalcitrant bladder neck contracture after radical prostatectomy for prostate cancer. The Journal of Urology. 185 (2), 391-392 (2011).
- Reiss, C. P., et al. The T-plasty: a modified YV-plasty for highly recurrent bladder neck contracture after transurethral surgery for benign hyperplasia of the prostate: clinical outcome and patient satisfaction. World Journal of Urology. 34 (10), 1437-1442 (2016).
- Shu, H. Q., et al. Laparoscopic T-plasty for the treatment of refractory bladder neck stenosis. American Journal of Men's Health. 13 (5), 1-7 (2019).
Réimpressions et Autorisations
Demande d’autorisation pour utiliser le texte ou les figures de cet article JoVE
Demande d’autorisationThis article has been published
Video Coming Soon