Method Article
Innovative Approach to Minimize Serious Complications in Cosmetic Dermal Filling
In This Article
Summary
The protocol proposes an innovative approach to cosmetic dermal filling focusing on ultrasound, icing, pressing, auxiliary gestures, and effective withdrawal to reduce the risk of serious complications like vascular occlusion. Despite the general safety of dermal fillers, accidents can still occur because of the inherent risks.
Abstract
Cosmetic dermal filling represents a significant advance in aesthetic medicine, providing non-invasive treatments with immediate and durable outcomes. Despite the generally safe nature of dermal fillers and avoidable complications with proper technique and planning, they are still risky, with potential complications varying from mild and transient to severe and enduring. This study introduces innovative strategies designed to decrease the risk of serious complications, such as vascular occlusion. These include the use of ultrasound guidance, the application of ice, auxiliary gestures, effective withdrawal, etc. Throughout our research, we observed no severe complications like embolism, skin necrosis, or ocular issues. However, minor complications such as erythema, edema, and bruising were noted. It is important to recognize that while most severe complications can be avoided with meticulous technique and planning, the inherent risk of unexpected outcomes persists in any medical procedure. Our findings suggest that with these innovative strategies, the safety of cosmetic dermal filling can be significantly enhanced, thereby minimizing the risk of severe adverse effects.
Introduction
The field of cosmetic surgery has witnessed a paradigm shift with the advent of dermal fillers, a development that has significantly altered the approach to aesthetic enhancement1. These non-invasive treatments, designed to combat the signs of aging and fatigue, offer individuals a viable option for rejuvenation, circumventing the need for traditional surgical interventions. The appeal of dermal fillers lies in their ability to deliver immediate, long-lasting results with minimal downtime, a crucial factor that has fueled their popularity among consumers seeking to enhance their appearance safely and effectively1,2. The growing demand for these treatments has been matched by an aggressive marketing push from pharmaceutical companies, which have positioned dermal fillers as an attractive solution for soft tissue enhancement2.
Despite the widespread acclaim and acceptance of dermal fillers in aesthetic medicine, the rise in their use has also highlighted a critical issue: the potential for adverse outcomes and complications. Documented extensively in the medical literature, these complications range from minor, temporary problems to severe, long-lasting issues3,4,5. Factors contributing to adverse complications include the procedural aspects, the injection techniques applied, and the specific types of fillers used6. Among these, the technique of injection stands out as a crucial determinant of safety and efficacy, particularly with temporary fillers7. The prevalence of undesirable outcomes has been notably linked to the practices of inexperienced or inadequately trained practitioners, who may prioritize financial gains over patient safety, employing sub-optimal injection techniques7.
Recognizing the need to address these concerns, we introduce a novel set of strategies to minimize the risk of one of the most serious complications associated with dermal fillers: vascular occlusion8,9. This condition, characterized by the obstruction of blood flow, can lead to irreversible tissue damage if not promptly and effectively managed9. The overall goal of our method is to enhance the safety profile of cosmetic dermal filling procedures by implementing measures such as ultrasound guidance, ice application, auxiliary maneuvers, and meticulous injection techniques. These innovative strategies are grounded in a thorough understanding of facial anatomy and filler dynamics, offering a significant advancement over traditional techniques by providing an additional layer of precision and safety.
The rationale behind the development of these techniques is rooted in the increasing incidence of complications associated with dermal fillers, necessitating a proactive approach to minimize risks. By integrating imaging technologies and refining procedural tactics, the method described in this study aims to circumvent the limitations of conventional injection techniques, thereby reducing the likelihood of vascular occlusion. Compared to existing methods, our approach offers several advantages. Ultrasound guidance, for instance, allows visualization of possible anatomic variation, enabling practitioners to avoid critical vascular structures and ensure optimal filler placement. Additionally, the application of ice and gesture maneuvers can further mitigate the risk of complications by reducing tissue swelling and facilitating smoother filler distribution.
Within the broader context of the literature on cosmetic procedures, this technique represents a significant contribution to enhancing the safety and efficacy of dermal filler treatments. By addressing the pivotal issue of vascular occlusion, the method not only improves patient outcomes but also contributes to the ongoing evolution of best practices in aesthetic medicine. For practitioners seeking to adopt the latest advancements in dermal filling, our study provides valuable insights and practical guidelines that underscore the importance of technique, planning, and patient safety in achieving optimal results.
Protocol
This study was carried out in accordance with the clinical ethics committee guidelines of the First Affiliated Hospital of Zhejiang University. Written informed consent was obtained from all participating patients. Sites of dermal filling generally include the tempora, tear trough, nasolabial fold, and chin. Patients with contraindications, like active skin infections, unrealistic expectations, or a history of related allergies, autoimmune diseases, bleeding disorders, and keloid scarring, were excluded.
1. Preoperative steps
- Take photographs of the intended injection areas from multiple angles.
- Perform an ultrasound (B-mode) examination of the intended injection sites (Figure 1) to delineate the course of major vessels for potential anatomical variations and to identify any remaining fillers in individuals who have previously received filler treatments10.
2. Pre-injection preparation
- Apply ice packs to the intended injection areas for 3-5 min (as long as it is bearable) before the procedure to promote vasoconstriction and reduce pain.
3. Patient positioning
- Have the patient sit in a semi-upright position.
- Disinfect the intended injection sites three times with iodine (Figure 2).
4. Auxiliary gesture
- Use the non-injection hand to apply pressure on the major vessel marked while performing the injection movement (Figure 3)
5. Injection techniques
- Penetrate the skin with an empty needle/cannula.
- Use 30-32 G needles for finer injections and more superficial placements, like the lips, fine lines, and tear trough.
- Use 25-27 G cannulas for their flexible and even distribution in areas like the cheeks, jawline, or nasolabial folds) or one pre-loaded with saline or lidocaine (0.5%).
- Penetrate the recommended needle/cannula and withdraw for 5 s (Figure 4).
NOTE: The angles of penetration during injections are indeed contingent on a variety of factors, such as the specific injection sites, the types of fillers being used, and the choice between needles or cannulas. Additionally, the desired effects the practitioner aims to achieve play a significant role in determining these angles.- Only proceed with the injection if no blood is aspirated. In cases of significant resistance or blood aspiration, reposition and attempt the same injection techniques.
- Inject fillers slowly while withdrawing the needle/cannula. Determine the injection technique-linear threading, fanning, serial puncture, or bolus injections-based on the specific injection sites and the type of filler used11,12.
6. Immediate post-injection
- Perform gentle massage and pressure on the injection site to ensure the even distribution of the dermal filler or to slide it to the desired location (Figure 5).
NOTE: The time for the massage or pressure is flexible as long as the filler is evenly distributed or precisely positioned in the desired area.
7. Symmetrical balance
- In cases where injections are administered bilaterally, allocate roughly 1/5 of the total injection volume to account for and correct any potential asymmetries, ensuring symmetrical balance in the final result. This reserved volume acts as a buffer, allowing adjustments to be made to achieve harmony and proportion between both sides, enhancing the overall aesthetic outcome.
8. Post-operative care
- Take photographs from multiple angles again.
- Apply antibiotic ointment on the penetration site.
- Apply ice packs across a sterile gauze and compress the injected area for 15 min.
- Instruct the patient from getting the treated area wet for 4-6 h and refrain from vigorous rubbing or massaging the injection site for the first 3 days.
- Advise follow-up in 1, 3, and 6 months.
Results
In the study, 50 patients seeking cosmetic enhancement were selected. The areas treated included temporal depression (5, needles 30 G), tear troughs (19, needles 32 G/ cannulas 30 G), nasolabial folds (22, needles 30 G/ cannulas 27-30 G), cheek depressions (2, cannulas 27-30 G), and chin (2, needles 30 G) (Table 1). A variety of needle and cannula sizes were chosen based on the treatment area and the type of dermal filler used. Deep filling (as support) is usually injected with 30 G needles, while superficial filling (for volume supplementation) is typically injected with 27-30 G cannulas or 32 G needles. The fillers selected were based on their viscosity and the desired outcome, ranging from fillers for fine wrinkles to more robust options for deeper volumization. The practitioners opted for 30-32 G needles for precision work in delicate areas like tear troughs and 27-30 G cannulas for broader, more volumizing treatments in the temporal depression, chin, or nasolabial folds. The procedures were performed following the techniques proposed, and patients were monitored for immediate reactions.
During and after the procedures, patients were observed independently by two irrelevant resident doctors for any immediate complications such as erythema, edema, or embolisms. Follow-up was conducted at least 2 weeks post-procedure to assess long-term complications, including infection, chronic allergic reactions, etc.
The absence of serious complications among the patients supports the hypothesis that with proper planning techniques, dermal fillers can be a safe cosmetic procedure (Figure 6). The transient and controllable nature of the minor complications encountered further reinforces the proposed approach's safety profile (Figure 7, Table 2). The findings of this study align with our initial hypothesis, suggesting the importance of detailed planning and injection techniques in facial dermal filling procedures. This evidence-based approach to dermal fillers not only enhances the safety and satisfaction of patients but also contributes to the broader understanding of best practices in cosmetic dermal filling.

Figure 1: B-ultrasound assistance. The figure shows the image of the superficial temporal artery under B-ultrasound for potential anatomic variation, ensuring safe and precise injection placement. Please click here to view a larger version of this figure.
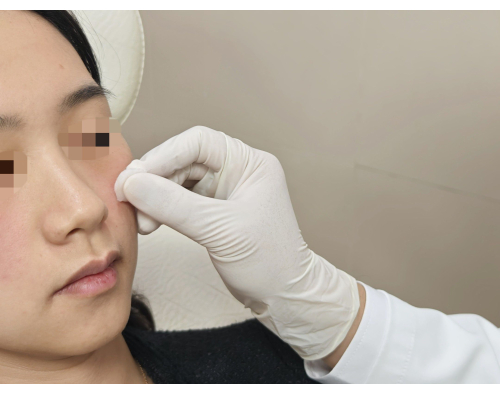
Figure 2: Position and disinfection. In this figure, the semi-upright position is demonstrated alongside the disinfection process, which is crucial for maintaining a sterile environment before injection. Please click here to view a larger version of this figure.

Figure 3: Auxiliary gesture. The technique of applying auxiliary pressure with the left index finger on the suborbital foramina is illustrated, which helps deflate the related vessels during tear trough filling with hyaluronic acid. Please click here to view a larger version of this figure.

Figure 4: Effective withdrawal. The figure showcases the penetration and effective withdrawal technique using a cannula pre-loaded with lidocaine (0.5%) on the tip, ensuring relatively safe delivery of fillers. Please click here to view a larger version of this figure.

Figure 5: Applying massage and pressure. The figure illustrates the gentle massage and pressure applied after the injection to evenly distribute the filler and reduce transient complications, demonstrating the importance of post-injection care. Please click here to view a larger version of this figure.

Figure 6: Fine instant result. The images of the front (left) and lateral (right), before (up) and immediately after (down) the injection procedure are displayed, showing a fine and satisfactory outcome without any complications. Please click here to view a larger version of this figure.

Figure 7: Mild and transient complication. The figure depicts the presence of slight erythema (redness) in the injection sites immediately after the procedure, which is a mild and transient complication post-injection. Please click here to view a larger version of this figure.
| Injection site | Number of patients | Needle/Cannula size |
| Temporal depression | 5 | 30 G Needles |
| Tear troughs | 19 | 32 G Needles/30 G Cannulas |
| Nasolabial folds | 22 | 30 G Needles/27–30 G Cannulas |
| Cheek depressions | 2 | 27–30 G Cannulas |
| Chin | 2 | 30 G Needles |
Table 1: Injection sites and needle/cannula sizes used in the patients. The injection/treatment sites included temporal depression (5, needles 30 G), tear troughs (19, needles 32 G/ cannulas 30 G), nasolabial folds (22, needles 30 G/ cannulas 27-30 G), cheek depressions (2, cannulas 27-30 G), and chin (2, needles 30 G).
| Total Subjects: 50 | Complications | Occurrence |
| Mild and Transient | Erythema | 6 (12%) |
| Edema | 3 (6%) | |
| Ecchymoses | 6 (12%) | |
| Discomfort | 3 (6%) | |
| Moderate and Rare | Hematoma | 0 |
| Infection | 0 | |
| Allergic Reactions | 0 | |
| Serious and Permanent: Embolism | Skin Necrosis | 0 |
| Vision Abnormalities | 0 | |
| Stroke | 0 |
Table 2: Complications encountered in the 50 patients who underwent cosmetic dermal filling.
Discussion
Cosmetic dermal filling stands out as a continually evolving and popular field in aesthetic medicine, driven by factors such as its non-invasive nature, immediate results, minimal downtime, and versatile functions in reducing wrinkles and restoring volume1,2. The appeal also lies in its achievement of natural-looking and long-lasting results1. The ongoing and anticipated rise in popularity can be attributed to innovations in filler formulations and injection techniques, promising enhanced outcomes and extended effects. Moreover, the growing interest in aesthetic enhancements among individuals contributes to the expansion of this field2.
It is crucial to acknowledge that while dermal fillers are generally considered safe, potential complications are not uncommon, ranging from mild and temporary to severe and enduring3, 4,13. Mild and transient complications, such as erythema, edema, ecchymoses, pain, or discomfort, are frequently observed but typically resolve within a few days3,4,13. Simple measures like local icing or compression can alleviate these issues. Relatively rare complications include hematoma, infection, and allergic reactions, necessitating proper medical intervention if they worsen4. In very rare instances, serious complications like vascular occlusion or embolism may occur if the filler inadvertently enters blood vessels, leading to vessel blockage and severe sequelae14,15. This can result in complications such as skin necrosis, scarring, vision abnormalities, blindness, and even stroke14,15,16,17. The prognosis of embolism caused by filler injection is usually poor, with long-lasting or permanent functional and aesthetic consequences. The severity of these adverse events, particularly embolism, raises concerns with the growing popularity of facial filler injections.
In this study, 50 patients underwent facial cosmetic dermal filling with the recommended injection process. The few complications encountered were all mild and transient, typical for such procedures. These transient problems mainly arose from the minimal injuries of needle/cannula penetration and subdermal dissection. Prompt and effective relief was achieved through local icing application. The critical steps outlined include comprehensive training in facial anatomy for practitioners, preoperative imaging to identify vascular structures, and the application of proper injection techniques to minimize complications. Notably, this protocol incorporates pre-injection icing to constrict vessels, reducing the likelihood of intravascular filler placement, and suggests employing auxiliary gestures for high-risk vessel areas to further mitigate risks. Troubleshooting steps like repositioning upon encountering significant resistance or blood aspiration underline the protocol's adaptability to intra-procedural challenges, demonstrating a proactive approach to complication prevention. The use of tools like empty or pre-loaded needles to ensure effective withdrawal and post-procedure massaging to ensure even filler distribution are also significant modifications aimed at enhancing safety and outcomes.
Despite the encouraging outcomes, it is crucial to recognize that the study's sample size was limited and confined to a single center, which may impact the generalizability of the findings. Plus, the efficacy and safety of cosmetic dermal filling are highly dependent on practitioner skill and experience, particularly in navigating complex facial anatomy and managing unexpected complications. The study's findings, while indicative of a reduced complication rate with adherence to the outlined protocol, may not be universally replicable, especially among less experienced practitioners. Additionally, the variability in patient anatomy and response to fillers suggests that even with the most diligent application of these techniques, the risk of adverse events, though minimized, cannot be eliminated.
Various factors, including the procedure itself, techniques employed during injection, and the specific filler used, contribute to the risk of adverse events6,7. Injection techniques, in particular, play a pivotal role, with inexperienced or unqualified practitioners using suboptimal methods for financial gain being a significant factor in unfortunate outcomes. Serious complications, notably embolism, associated with cosmetic dermal filling can be significantly minimized by focusing on details and employing specific techniques during the injection process7. This study summarizes and standardizes preventive injection measures to maximize complication risk reduction, focusing on five key aspects. Firstly, practitioners must undergo comprehensive training in facial anatomy to develop a thorough understanding of relevant vessels at injection sites. Utilizing preoperative ultrasound (B-mode), as we recommended, can be a powerful tool in imaging vessels and identifying potential anatomical variations.
While anatomical knowledge aids in complication prevention, meticulous planning, and proper injection techniques are crucial. Pre-injection icing helps constrict vessels at injection sites, reducing the likelihood of filler injection into these vessels. In situations where encountering risky vessels is unavoidable, auxiliary gestures and effective injection withdrawal become crucial to prevent fillers from entering these vessels. Applying temporary pressure at the vessel's starting route constricts its caliber, decreasing the risk of penetration. Effective and valid withdrawal is essential to avoid direct injection into vessel lumens, preventing serious embolism. Some dermal fillers may block needles or cannulas after a single injection. Using empty needles/cannulas or those pre-loaded with saline or lidocaine significantly enhances the validity of injection withdrawal. Significant resistance during injection may indicate arterial injection, necessitating repositioning. Post-procedure massaging aids in even filler distribution, reducing the risk of irregularities or unevenness. Reserving a small volume for the final stages helps prevent asymmetry in bilateral injections.
Also, practitioners must possess a clear understanding of the attributes and characteristics of available dermal fillers to choose the right one. Different fillers exhibit varying viscoelasticity and cohesivity, influencing associated risks. Some fillers are better suited for specific facial areas, while others pose a higher risk of complications5. The practitioner should carefully consider patient needs and filler characteristics when selecting the most suitable product.
Additionally, practitioners should be attentive to the patient's medical history18. Vascular anatomy alterations from previous injections or surgeries may elevate the risk of vascular accidents. Patients with autoimmune disorders, multiple allergies, bleeding disorders, or infection/inflammation at injection sites should avoid dermal filling due to associated complications.
Early recognition and effective management of complications are vital to minimize adverse effects and improve patient outcomes. Patients are advised to remain under observation for 30 min post-injection. Practitioners must be trained to recognize early signs of complications, such as blood supply disturbance or embolism, and have a thoughtful plan in place to address these issues promptly6,13,19.
Compared to existing methods11,12,20, this study's protocol offers a structured, detailed approach to reducing the risk of complications associated with cosmetic dermal filling. Focusing on anatomical knowledge, pre-procedural planning, and specific injection techniques provides a comprehensive framework that enhances the safety and effectiveness of dermal fillers. This protocol's significance lies in its potential to serve as a benchmark for best practices in the rapidly evolving field of aesthetic medicine, promoting both patient safety and satisfaction.
Looking ahead, the continuous advancement in filler materials and technology presents an opportunity for further refinement of injection techniques. Future applications may include the integration of advanced imaging technologies for real-time visualization of filler placement, the development of new filler materials with reduced complication profiles, and personalized treatment plans based on detailed patient anatomical assessments. Moreover, as the field progresses, the protocol may adapt to incorporate emerging evidence and techniques, ensuring that practice evolves in tandem with innovation.
In conclusion, this study contributes valuable insights into the practice of cosmetic dermal filling, highlighting the criticality of precise techniques and the potential for future advancements. While acknowledging its limitations, the protocol presented herein marks a step forward in the quest to optimize safety and outcomes in aesthetic medicine.
Disclosures
The authors have nothing to disclose.
Acknowledgements
We would like to thank Dr. Tingbo Liang (Hepatobiliary and Pancreatic Surgery, The First Affiliated Hospital, School of Medicine, Zhejiang University) for helping project this manuscript.
Materials
| Name | Company | Catalog Number | Comments |
| Hyaluronic Acid | YVOIRE | CFDA(A)20163131804 | Serves as a supporting role; Supplied with the injection needles (30–32 G) |
| Hyaluronic Acid | Imeik | (01)08800050200083 | Serves as volume filling; Supplied with the injection needles |
| Cannulas | Conpuvon | 20200017 | For volume filling |
| Ultrasound | Philips | EPIQ-5/US120C1632 | Detect anatomic variations or remaining fillers from previous treatments |
References
- Cassuto, D., Bellia, G., Schiraldi, C. An overview of soft tissue fillers for cosmetic dermatology: from filling to regenerative medicine. Clin Cosmet Investig Dermatol. 14, 1857-1866 (2021).
- Bukhari, S. N. A., et al. Hyaluronic acid, a promising skin rejuvenating biomedicine: A review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects. Int J Biol Macromol. 120, 1682-1695 (2018).
- Ozturk, C. N., et al. Complications following injection of soft-tissue fillers). Aesthet Surg J. 33 (6), 862-877 (2013).
- Oranges, C. M., Brucato, D., Schaefer, D. J., Kalbermatten, D. F., Harder, Y. Complications of nonpermanent facial fillers: A systematic review. Plast Reconstr Surg Glob Open. 9 (10), e3851 (2021).
- Vedamurthy, M. Beware what you inject: Complications of injectables-dermal fillers. J Cutan Aesthet Surg. 11 (2), 60-66 (2018).
- Bailey, S. H., Cohen, J. L., Kenkel, J. M. Etiology, prevention, and treatment of dermal filler complications. Aesthet Surg J. 31 (1), 110-121 (2011).
- Urdiales-Gálvez, F., et al. Preventing the complications associated with the use of dermal fillers in facial aesthetic procedures: An expert group consensus report. Aesthetic Plast Surg. 41 (3), 667-677 (2017).
- Vargas-Laguna, E., García-Gavín, J., Bárcena-Ruiz, E. Safety in dermatologic procedures: Vascular occlusion by filling materials. Actas Dermosifiliogr. 112 (9), 794-797 (2021).
- Loyal, J., Hartman, N., Fabi, S. G., Butterwick, K. J., Goldman, M. P. Cutaneous vascular compromise and resolution of skin barrier breakdown after dermal filler occlusion-Implementation of evidence-based recommendations into real-world clinical practice. Dermatol Surg. 48 (6), 659-677 (2022).
- Schelke, L. W., Decates, T. S., Velthuis, P. J. Ultrasound to improve the safety of hyaluronic acid filler treatments. J Cosmet Dermatol. 17 (6), 1019-1024 (2018).
- Alam, M., Tung, R. Injection technique in neurotoxins and fillers: planning and basic technique. J Am Acad Dermatol. 79 (3), 407-419 (2018).
- Dayan, S. H., Bassichis, B. A. Facial dermal fillers: selection of appropriate products and techniques. Aesthet Surg J. 28 (3), 335-347 (2008).
- Funt, D., Pavicic, T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Plast Surg Nurs. 35 (1), 13-32 (2015).
- DeLorenzi, C. Complications of injectable fillers, Part 2: Vascular Complications. Aesthet Surg J. 34 (4), 584-600 (2014).
- Zhuang, J., Zheng, Q., Su, X., Jiang, L., Hu, J. Clinical manifestations and prognosis of embolism caused by filler injection in different facial regions. Plast Reconstr Surg Glob Open. 11 (8), e5225 (2023).
- Wang, H. C., et al. Cerebral embolism as a result of facial filler injections: A literature review. Aesthet Surg J. 42 (3), 162-175 (2021).
- Tran, A. Q., Lee, W. W. Vision loss and blindness following fillers. J Dermatol Skin Sci. 3 (2), 1-4 (2021).
- De Boulle, K., Heydenrych, I. Patient factors influencing dermal filler complications: prevention, assessment, and treatment. Clin Cosmet Investig Dermatol. 8, 205-214 (2015).
- Wollina, U., et al. Complication of soft tissue fillers: prevention and management review. J Drugs Dermatol. 19 (9), 829-832 (2020).
- Glogau, R. G., Kane, M. A. C. Effect of injection techniques on the rate of local adverse events in patients implanted with nonanimal hyaluronic acid gel dermal fillers. Dermatol Surg. 34, S105-S109 (2008).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved