Case Report
Laparoscopic Anatomical Resection of The Right Anterior Lobe Based on The Laennec Capsule Technique
In This Article
Summary
This protocol describes a laparoscopic anatomical right anterior sectionectomy utilizing the Laennec capsule concept, combined with comprehensive preoperative therapy. The approach enables precise tumor resection in hepatocellular carcinoma (HCC) cases closely associated with major vascular structures, improving surgical safety, efficacy, and long-term patient outcomes.
Abstract
This paper presents a laparoscopic anatomical resection technique for hepatocellular carcinoma (HCC) utilizing the Laennec capsule concept. The goal of this protocol is to improve surgical precision and safety during complex liver resections, particularly in tumors closely associated with vital vascular structures, by ensuring clear identification and dissection of critical anatomical landmarks. Surgical resection remains the primary curative treatment for hepatocellular carcinoma (HCC), but laparoscopic anatomical right anterior sectionectomy becomes particularly challenging when tumors are closely associated with major vascular structures, as this increases the risk of significant bleeding. Comprehensive preoperative treatment, including targeted therapy, immunotherapy, and hepatic arterial infusion chemotherapy (HAIC), can reduce tumor size and improve surgical outcomes, making previously borderline resectable tumors operable. In this case, a 75-year-old patient with a tumor in segment 8 (S8) of the liver, closely associated with major vascular structures, underwent two cycles of preoperative treatment. This reduced the tumor size from 6 cm by 5 cm to 4.5 cm by 3.1 cm. Laparoscopic anatomical right anterior sectionectomy was performed using the Laennec capsule, an anatomical structure that aids in vascular dissection. The procedure lasted 240 minutes with minimal blood loss (200 mL). The tumor was successfully resected with negative surgical margins, and the patient was discharged on the seventh postoperative day without complications. Postoperatively, the patient was monitored for signs of liver dysfunction and underwent routine imaging to assess for recurrence. Follow-up included liver function tests and regular CT scans, showing no recurrence after 6 months. This case demonstrates that the combination of the Laennec capsule technique and comprehensive preoperative treatment allows for precise, minimally invasive resections of HCC tumors closely associated with vascular structures, providing a safe and effective solution to challenging liver tumors with minimal intraoperative complications and promising postoperative outcomes.
Introduction
Hepatocellular carcinoma (HCC) is a significant global health concern, representing 75% to 85% of primary liver cancers. It ranks as the 6th most common malignancy worldwide and is the 4th leading cause of cancer-related deaths globally1. In China, HCC remains a major challenge, ranking 4th in cancer incidence and 3rd in cancer mortality2. The primary goal of managing HCC is to achieve complete resection of the tumor while preserving liver function and minimizing complications, particularly in cases involving tumors adjacent to major vascular structures
Managing HCC becomes particularly complex when tumors are located near vital hepatic structures. The close proximity to these critical structures significantly complicates surgical intervention, necessitating a strategic approach to treatment. The challenges are exacerbated by risks of intraoperative bleeding, incomplete resection, and postoperative complications, highlighting the need for innovative surgical techniques and comprehensive preoperative management
Recent advancements in multidisciplinary treatment strategies, including targeted therapy, immunotherapy, and hepatic arterial infusion chemotherapy (HAIC), have shown promise in managing such challenging cases3. These therapies aim to reduce tumor size and improve surgical outcomes, making previously inoperable tumors amenable to resection4,5. In this context, the concept of the Laennec capsule, which focuses on precise anatomical dissection within the hepatic capsule, provides a framework for performing complex liver surgeries with improved precision and safety6,7.
This paper presents a patient with stage IB HCC, where neoadjuvant therapy comprising targeted therapy, immunotherapy, and HAIC successfully reduced the tumor size. Following this multimodal treatment, a laparoscopic anatomical right anterior sectionectomy was performed using the Laennec capsule concept. This approach enabled meticulous dissection of the right anterior branch of the portal vein, middle hepatic vein, and right hepatic vein, facilitating a successful resection with clear margins. The overall goal of this method is to integrate advanced neoadjuvant therapies with minimally invasive surgical techniques to achieve safe and effective resections of complex HCC cases, particularly those involving tumors closely associated with critical vascular structures.
The integration of advanced therapeutic modalities and innovative surgical techniques underscores progress in managing complex HCC cases, offering patients enhanced surgical outcomes and improved prognoses. Compared to conventional approaches, this combined strategy offers enhanced safety, reduced invasiveness, and improved long-term prognosis, providing a promising pathway for addressing high-risk HCC cases involving complex vascular anatomy.
CASE PRESENTATION:
The patient, a 75-year-old female, presented with a recent diagnosis of a liver tumor. A CT scan performed at an external hospital revealed a space-occupying lesion in the S8 segment, raising concerns about primary hepatocarcinoma. No significant family history of liver disease or cancer was reported. The patient was a non-smoker with no history of alcohol consumption. The patient was retired and lived in an urban area with access to healthcare facilities. No history of chronic liver diseases such as hepatitis or cirrhosis. The patient reported hypertension managed with medication and no history of diabetes or cardiovascular disease. No previous abdominal surgeries. The patient was asymptomatic, with no complaints of abdominal pain, jaundice, weight loss, or fatigue. Physical examination showed abdomen soft and non-tender, no palpable masses or organomegaly, and no signs of ascites or peripheral edema. The patient had not undergone any treatmentsprior to this admission.
Diagnosis, Assessment, and Plan:
The initial diagnosis of hepatocellular carcinoma (HCC) was made based on imaging findings and elevated alpha-fetoprotein (AFP) levels. The patient was staged as IB (pT1N0M0) according to the AJCC 8th Edition guidelines8. A treatment plan was established to include two cycles of neoadjuvant therapy, consisting of targeted therapy, immunotherapy, and hepatic arterial infusion chemotherapy (HAIC), to reduce tumor size and ensure operability. The patient was then scheduled for laparoscopic anatomical right anterior sectionectomy. After physical examination, the blood pressure was 130/80 mmHg, heart rate: 75 bpm, respiratory rate: 18 breaths/min, and temperature: 36.8 °C. The abdomen showed no visible distension or abnormal vascular patterns, and the liver and spleen were not palpable. No signs of cachexia or malnutrition were found. Skin and sclera were non-icteric. No spider angiomas or palmar erythema were observed.
Protocol
Prior to the surgery, the patient provided written informed consent. The surgical procedure was approved by the institutional review board at Dongguan Bin-Hai-Wan Central Hospital.
1. Preoperative preparation
- Neoadjuvant therapy
- Targeted therapy: Administer targeted therapy with Lenfacitinib at 8 mg QD, orally for two cycles. Each cycle of comprehensive therapy was administered approximately every 21 days.
This aims to reduce the tumor size and improve its resectability by inhibiting tumor vascularization and progression.
NOTE: Lenfacitinib is a tyrosine kinase inhibitor that targets multiple kinases involved in tumor angiogenesis and growth9. - Immunotherapy: Administer tislelizumab at 200 mg by intravenous (IV) mode over a specified period, commonly around 30 min to 1 h, depending on the patient's response and the specific protocol followed to stimulate the patient's immune system to target and eliminate tumor cell. Administer the drug every 3 weeks. Before administration, assess patients for any allergies to monoclonal antibodies or specific components of the formulation. Closely monitor patients during and after (typically 30 min to 1 h) the infusion for any signs of infusion-related reactions, such as fever, chills, hypotension, rash, or difficulty breathing.
NOTE: Tislelizumab is an anti-PD-1 monoclonal antibody that enhances the immune response against cancer cells10. Corticosteroids, antihistamines, or acetaminophen may be given before infusion to minimize the risk of infusion-related reactions. Proper hydration is recommended during the infusion to help prevent side effects and support kidney function. If a patient experiences anxiety or discomfort, mild sedatives or analgesics may be used. - Hepatic Arterial Infusion Chemotherapy (HAIC): Administer the HAIC with the FOLFOX4 regimen (Oxaliplatin, Leucovorin, and 5-FU) for two cycles to reduce tumor size, control intrahepatic spread, and enhance resectability. Administer drugs every 3 weeks for 2 cycles, after which tumor response is evaluated.
- Administer Oxaliplatin at 85 mg/m², infused through the hepatic artery over 2 h on Day 1. Administer Leucovorin at 200 mg/m², infused through the hepatic artery over 2 h on Day 1. Administer 5-Fluorouracil (5-FU) as a bolus dose of 400 mg/m² administered by hepatic artery infusion on Days 1 and 2 and then by continuous infusion at 600 mg/m² over 22 h on Days 1 and 2.
- Before the procedure, ensure the liver function is sufficient (bilirubin <2 mg/dL, INR <1.5, and adequate platelet count). Rule out contraindications, such as portal vein thrombosis, extrahepatic metastases, or severe cardiovascular conditions. Administer prophylactic antibiotics to prevent infection at the catheter insertion site.
- Administer local anesthesia during catheter placement to minimize discomfort for the hepatic arterial infusion system. Deliver the chemotherapy directly into the liver through a catheter inserted into the hepatic artery.
- Insert a sterile catheter, typically a microcatheter or arterial catheter compatible with HAIC, through the femoral or radial artery using the Seldinger technique. Use a guidewire for precise placement and use fluoroscopic guidance to ensure the catheter tip is positioned correctly in the hepatic artery.
- Place the catheter using interventional radiology and connect it to an infusion pump or reservoir to control the rate of drug delivery. Monitor for immediate complications, such as arterial spasm or catheter misplacement. Monitor for hepatic artery thrombosis, dislodgement of the catheter, or hepatic toxicity. Perform regular blood tests to evaluate liver and kidney function and monitor for systemic toxicities.
NOTE: This delivers chemotherapy directly to the liver, enhancing its therapeutic effect while minimizing systemic toxicity11.
- Targeted therapy: Administer targeted therapy with Lenfacitinib at 8 mg QD, orally for two cycles. Each cycle of comprehensive therapy was administered approximately every 21 days.
- Imaging evaluation
- Abdominal CT scan: Perform a contrast-enhanced abdominal CT scan to assess the tumor's size, location, and relationship with adjacent structures, including the hepatic veins, portal veins, and inferior vena cava. Evaluate the tumor's vascularity and note critical information for surgical planning. Contrast-enhanced CT examination before comprehensive treatment indicated a tumor located in the S8 segment, approximately 6.5 cm × 5.5 cm in size (Figure 1A), the tumor was closely associated with the second hepatic portal, inferior vena cava (IVC), right hepatic vein, middle hepatic vein, right anterior branch of the portal vein (Figure 1B), and right posterior branch of the portal vein.
- Magnetic resonance imaging (MRI) with enhanced liver: Perform an MRI using liver-specific contrast agents (e.g., gadoxetate disodium) to more precisely delineate the tumor's borders, identify liver parenchyma involvement, and assess any extrahepatic spread. Use the information to assess liver function and vascular anatomy in greater detail. After two cycles of treatment, the tumor size was reduced to 4.3 cm x 3.1 cm (Figure 2A, 2B).
- 3D Liver reconstruction imaging: Perform three-dimensional (3D) liver reconstruction imaging to evaluate the tumor's relationship with critical vascular structures, such as the right hepatic vein, middle hepatic vein, and portal veins. Visualize the liver's vascular anatomy and use it to plan the extent of the resection. The tumor maintained close proximity to major vascular structures but showed clear demarcation from the second hepatic portal and inferior vena cava (Figure 3A-C)
- Laboratory evaluation
- Liver function tests: Obtain a complete liver function panel, including measurements of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), total bilirubin, and albumin. Use test data to assess the patient's liver reserve and identify any underlying liver dysfunction.
- Ask the patient to fast for 8-12 h prior to sample collection to avoid interference from food or medications. Note any medications that may affect liver function. Select an appropriate vein, typically in the antecubital fossa (inner elbow), and clean the site with an alcohol swab to ensure sterility.
- Use a sterile butterfly needle or straight needle to access the vein. Attach a vacuum-sealed blood collection tube, often with specific additives like heparin (for plasma) or EDTA (to prevent clotting), to the needle for blood collection. Draw approximately 5-10 mL of blood into one or more tubes, depending on the tests required.
- Invert tubes gently to mix the blood with any preservatives or anticoagulants. After the sample is collected, remove the needle and apply pressure to the puncture site to prevent bleeding. Apply a bandage.
- Label the blood samples with the patient's details and send them to the laboratory for analysis. Store and transport blood samples under appropriate conditions, such as refrigeration at 2-8 °C, to maintain sample integrity. In the lab, process the samples to separate serum or plasma, depending on the test requirements.
- Alpha-fetoprotein (AFP): Measure serum AFP levels to assess hepatocellular carcinoma (HCC) activity. Elevated AFP is commonly associated with HCC and serves as a tumor marker for prognosis. Before comprehensive treatment, the alpha-fetoprotein (AFP) level was 95 ng/mL. After two cycles of treatment, the AFP was reduced to 2.29 ng/mL.
- Leave the blood sample, collected as described in step 1.3.1, to clot at room temperature for 15-30 min. Centrifuge the samples for about 10 min at 1,500-2,000 x g to separate the serum from other blood components. Transfer the separated serum into a sterile secondary container, if required. Store at 2-8 °C if analyzed within a few hours or frozen at -20 °C or lower for longer storage.
- Coagulation profile: Evaluated coagulation parameters, including prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT), to assess the patient's bleeding risk during surgery.
- Collect blood samples as described in step 1.3.1. To measure PT, assess the time it takes for blood to clot after the addition of tissue factor and use INR to standardize PT results. To measure aPTT, assess the time it takes for blood to clot after the addition of an activator to the intrinsic pathway of coagulation.
- Kidney function tests: Perform renal function tests, including serum creatinine and blood urea nitrogen (BUN), to evaluate the patient's renal status, particularly in anticipation of nephrotoxic treatments.
- Preparation for urine collection: For random urine collection, no special preparation is required, though patients may be advised to collect a sample in the morning for better consistency. For 24 h urine collection, instruct the patient to collect all urine over a 24 h period in a provided container. Discard the first-morning urine and collect the following urine voids, including the first-morning void of the following day.
- Collection Process: For a random urine sample, instruct the patient to urinate into a sterile container. Prefer a midstream urine sample to avoid contamination from the genital area. For 24 h urine sample: Collect all urine produced by the patient within a 24 h period. Ask the patient to store the container in a cool place (e.g., refrigerator) during the collection period to prevent bacterial growth.
- Post-collection handling: Label the urine sample with patient details and send it to the laboratory for testing. Perform tests such as urine protein levels, urinalysis (for blood, glucose, or infection indicators), and urine creatinine. If not analyzed immediately, keep urine samples refrigerated and test within 24 h of collection to avoid degradation.
- Liver function tests: Obtain a complete liver function panel, including measurements of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), total bilirubin, and albumin. Use test data to assess the patient's liver reserve and identify any underlying liver dysfunction.
- Preoperative medications and adjustments
- Anticoagulation adjustment: If the patient receives anticoagulant therapy, discontinue it at least 5 days before surgery to minimize bleeding risks. Provide bridging therapy with low-molecular-weight heparin (LMWH) if the patient has a high thrombotic risk.
- Preoperative antibiotics: Administer prophylactic antibiotics, such as cefazolin, 1 h prior to surgery to reduce the risk of infection. Administer cefazolin 1-2 g by IV injection. For patients with higher body weight (>120 kg), increase the dosage to 3 g. In patients with impaired renal function, adjust dosage based on renal function (e.g., eGFR) as necessary.
NOTE: The optimal time for antibiotic administration is within 60 min prior to the surgical incision to ensure effective blood levels during the procedure. For longer surgeries (>3-4 h) or significant blood loss, additional doses may be required. - Fasting instructions: Instruct the patient to fast for at least 8 h before surgery to reduce the risk of aspiration during anesthesia induction. Allow clear fluids for up to 2 h before the procedure.
- Anesthesia preparation
- Preoperative assessment by anesthesiologist: Perform a thorough preoperative assessment to evaluate the patient's cardiopulmonary status, allergies, and airway risk.
- Anesthetic plan: Discuss a general anesthesia plan with endotracheal. Ask the team to be prepared for potential intraoperative complications, including significant bleeding or the need for vasopressor support.
- Preoperative indocyanine green injection
NOTE: The preoperative injection of indocyanine green (ICG) serves two primary purposes: Assessment of liver function by quantifying the ICG retention rate at 15 min (ICG-R15) provides an estimation of the liver's functional reserve, which is critical for surgical planning, especially in hepatocellular carcinoma (HCC) cases. Tumor localization during surgery: Intraoperative fluorescence imaging with ICG enhances the visualization of the tumor and facilitates precise resection by clearly delineating its boundaries.- Using a sterile technique for administering ICG administer an intravenous injection through a peripheral vein. Administer the injection 24 h before surgery for accurate functional assessment with a dosage of 0.5 mg/kg body weight.
- For intraoperative tumor localization, administer a dose of 0.25 mg/kg body weight. Administer the injection 1-3 days before surgery to allow optimal fluorescence accumulation in the tumor.
- For liver function monitoring: Draw 2-3 mL of blood samples as per step 1.3.1 15 min after ICG injection to calculate the ICG-R15 value using a spectrophotometer at 805 nm.
- Calibrate the device using a blank sample (e.g., distilled water or a plasma sample without ICG). Centrifuge the blood sample at 3,000 x g for 10 min to separate plasma from blood cells. Use clear plasma for spectrophotometric analysis.
- Place the plasma sample into a quartz cuvette to ensure accurate light transmission. Insert the cuvette into the spectrophotometer and measure the optical density (OD) of the sample. Compare the OD of the sample at 15 min post-injection to the baseline OD immediately after injection.
- For intraoperative use, ensure the fluorescence imaging system is functional and calibrated to detect the emitted fluorescence during surgery.
- Observe the following precautions for ICG administration. Assess the patient for any history of allergies to ICG or iodine-containing substances. Monitor for adverse reactions such as anaphylaxis, though these are rare. Adjust the dosage if renal dysfunction or other contraindications are present.
NOTE: This protocol ensures both the preoperative functional evaluation and intraoperative tumor localization, improving the safety and precision of liver surgeries.
2. Surgical technique
- Anesthesia and patient positioning: After successful intubation and anesthesia, position the patient in the supine position. Use routine iodine tincture for abdominal disinfection and apply drapes.
- Make a 2 cm incision using a sterile scalpel below the umbilicus and insert a trocar into the abdominal cavity. Insufflate carbon dioxide gas to create a pneumoperitoneum with a pressure of 12 mmHg.
- Explore the cavity. Exploration revealed nodular sclerosis of the liver, with the tumor located in the right anterior lobe. No metastatic lesions were found in the peritoneum or other organs.
- Based on preoperative planning and intraoperative findings, a right anterior liver resection approach was chosen. After fully mobilizing the right liver ligaments, perform intraoperative ultrasound to accurately locate the tumor boundaries, hepatic veins, portal veins, bile ducts, and hepatic arteries. Place the high-frequency ultrasound probe in the appropriate liver regions to assess the tumor's size, shape, and its relationship with surrounding structures.
- Mark resection margins on the liver surface using electrocautery. Use color Doppler ultrasound to evaluate blood flow within the hepatic veins, portal veins, and hepatic arteries, ensuring clear identification of these structures and helping to avoid injury during resection.
- Closely monitor the tumor's vascularity and its proximity to major blood vessels to guide precise tumor excision and minimize complications. This real-time imaging technique enhances the safety and accuracy of liver resection, particularly in complex cases.
- Apply the Pringle maneuver with a vascular tape to occlude the hepatoduodenal ligament for 15 min intervals with 5 min reperfusion.
- Separate the right anterior Glissonean pedicle, with the Laennec's membrane used to bluntly separate the left edge of the gallbladder plate from the Glisson's pedicle root (gate IV; Figure 4A).
- Separate the right edge of the gallbladder plate above the Rouvieres groove (gate V). Separate the right anterior lobe (segments 5 and 8) along the line connecting gate IV and gate V (Figure 4B)
- Expose the gallbladder and dissect it using an ultrasonic scalpel. Use the ultrasonic scalpel, set at an appropriate frequency and power level, to separate the gallbladder from the liver bed, cutting through the tissue and simultaneously sealing small blood vessels to minimize bleeding.
- For cutting tissue, set the power typically between 30 W to 80 W. For coagulation, set between 20 W and 60 W. Set the frequency electrocautery systems to typically around 500 kHz to 1 MHz (megahertz). This frequency is chosen because it provides a balance between efficient tissue cutting and coagulation with minimal thermal damage to surrounding tissues.
- Use a liver retractor or manual retraction to gently lift the liver superiorly, exposing the gallbladder beneath it. Take care to avoid damaging the liver capsule during retraction. If peritoneal adhesions around the gallbladder are present, use blunt dissection or monopolar cautery to dissect them for clear visualization of the gallbladder and the hepatocystic triangle. Position laparoscopic instruments or surgical sponges to maintain clear exposure of the gallbladder during subsequent steps.
- Carefully isolate the cystic duct and cystic artery and divide using the ultrasonic scalpel, with any bleeding vessels secured using clips. After the gallbladder is fully detached from its attachments, remove it from the abdominal cavity through the incision.
- After resection of the gallbladder, use intraoperative ultrasound again to locate and mark the tumor boundaries and the projections of the middle hepatic vein, right hepatic vein, and right anterior liver pedicle on the liver surface. Use ICG-mediated near-infrared imaging to confirm the tumor boundaries.
- Use a 7-0 suture to occlude the right anterior liver pedicle, blocking blood flow to the right anterior lobe (segments 5 and 8). After blocking the planned resection area, inject a dose of 0.5-1.0 mg/kg of ICG intravenously, typically 15-30 min before the procedure.
- During surgery, use a near-infrared fluorescence camera to visualize the ICG uptake. The ICG counterstaining revealed that the right anterior lobe showed no fluorescence. This allowed the surgeon to accurately define the extent of resection. By utilizing this information, the surgical team was able to precisely delineate the boundary for liver resection, ensuring the tumor tissue was completely removed while preserving as much healthy liver tissue as possible.
- Based on the course of the middle hepatic vein, incise the liver capsule distally and identify the hepatic vein branches to locate the middle hepatic vein trunk. Use non-energy instruments such as forceps and suction devices to separate along the gap between Laennec's capsule and the hepatic vein.
- Clamp the veins on the resection side and cut it. Use an ultrasonic scalpel to transect the liver parenchyma. The tumor was found to be closely adherent to the middle hepatic vein and the root of the right hepatic vein but did not invade the veins (Figure 5A).
- Expose the target vessel by blunt dissection and appropriate tissue incision, ensuring the vessel is clearly visible for precise clamping. Choose an appropriately sized vessel clamp (select the type based on the vessel size and the need for clamping, commonly straight or curved clamps). Place the vessel clamp smoothly across both sides of the vessel, ensuring that the clamping area fully covers the vessel to prevent blood flow.
- Use laparoscopic dissecting forceps to continue separating the tumor from Laennec's capsule and the hepatic vein. Continue the dissection along the cephalic side of the middle hepatic vein until the roots of the right hepatic vein and the middle hepatic vein are fully exposed.
- Then, continue to dissect the surrounding tissue of the right anterior hepatic pedicle and use a stapler to transect the right anterior hepatic pedicle. Transect the liver parenchyma from the distal end between the right anterior lobe and the right posterior lobe, observing that the tumor is closely adherent to the right hepatic vein but does not invade the vein (Figure 5B).
- Use blunt dissection forceps and a suction device to separate along the Laennec capsule between the right hepatic vein and the tumor, clamp the venous tributaries on the resection side, and use an energy device to transect the liver parenchyma until the liver parenchyma on the resection side was completely transected. Complete the right anterior lobe resection, fully preserving the middle hepatic vein and the right hepatic vein (Figure 5C).
- Place the resected specimen in a specimen bag and irrigate the abdominal cavity with sterile distilled water. Check the surgical field for active bleeding, bile leakage, and gastrointestinal injury. Place drains at the liver cut surface and gallbladder fossa.
- Specimen removal and closure: Extend the umbilical incision to 5 cm and insert a wound protector. Place the resected liver lobe into a sterile specimen bag and remove it (Figure 6). Irrigate the abdominal cavity with 2 L of warm saline. Place two silicone drains (16 Fr) near the liver cut surface and gallbladder fossa. Close the abdominal wall in layers: Fascia with Vicryl 1-0 interrupted sutures and skin with Monocryl 4-0 subcuticular sutures.
3. Postoperative procedures
- Monitor vital signs and drain output daily. Perform blood tests for liver function, coagulation profiles, and electrolyte levels regularly during the first few days after surgery, specifically on postoperative days 1, 3, and 7. Remove drains once the output is serious (<50 mL/day); discharge the patient on postoperative day 7 if stable, with instructions for follow-up imaging in 1 month.
NOTE: Serous means the fluid draining from a surgical wound or drain site is clear and watery in appearance, similar to the serum part of blood. It is typically a normal type of drainage during the postoperative period, indicating the absence of infection or significant bleeding. Serous fluid is generally light yellow or pale and is composed of water, electrolytes, and small amounts of proteins. This is in contrast to other types of fluid, such as purulent (pus-like) or sanguineous (bloody) drainage, which may indicate infection or other complications. - Provide adequate pain relief using analgesics, including opioids and non-steroidal anti-inflammatory drugs (NSAIDs), with the aim of managing postoperative discomfort while minimizing side effects.
- Administer prophylactic antibiotics at the time of surgery and continue for 48 h postoperatively to reduce the risk of infections.
- Perform a follow-up contrast-enhanced CT or MRI scan within 1-3 months postoperatively to evaluate for any recurrence of tumors and assess liver function.
- Monitor serum AFP levels regularly to track for potential recurrence of hepatocellular carcinoma.
- Schedule regular follow-up visits every 3-6 months for the first 2 years and then annually thereafter, including physical exams, imaging studies, and laboratory tests, to monitor for recurrence or metastasis.
Results
For the protocol described here, the patient, a 75-year-old asymptomatic female, presented with an incidentally detected liver mass. Her medical and surgical history was unremarkable, except for hypertension. Physical examination and vital signs were within normal limits. Further diagnostic evaluations, including imaging and laboratory tests, were conducted to confirm the diagnosis and plan treatment.
On April 23, 2023, further CT and EOB-MR scans confirmed a tumor located in the S8 segment, approximately 6.5 cm x 5.5 cm in size (Figure 1A), and AFP was 95 ng/mL. The tumor was closely associated with the second hepatic portal, inferior vena cava (IVC), right hepatic vein, middle hepatic vein, right anterior branch of the portal vein (Figure 1B), and right posterior branch of the portal vein. Due to the challenging surgical difficulty, a comprehensive treatment regimen was initiated, including targeted therapy (Lenfacitinib, 8 mg QD orally), immunotherapy (Tislelizumab, 200 mg IV every 3 weeks), and HAIC (FOLFOX4).
After two cycles of treatment, the tumor size was reduced to 4.3 cm x 3.1 cm (Figure 2A,B). The tumor maintained close proximity to major vascular structures but showed clear demarcation from the second hepatic portal and inferior vena cava (Figure 3A-C). Serum tumor marker AFP was 2.29 ng/mL, and liver and kidney function and coagulation function were normal. Performance status was normal, and the Child-Pugh grade was A.
The surgery lasted 240 min, with an intraoperative blood loss of 200 mL. The patient passed gas within 24 h postoperatively. No abdominal bleeding, bile leakage, abdominal infection, incision infection, or liver failure occurred. The postoperative hospital stay was 7 days (Table 1).
Histopathological analysis of paraffin-embedded tissue sections showed moderately to poorly differentiated hepatocellular carcinoma, with approximately 76% of the cancer tissue being completely necrotic. There was no neural invasion or vascular tumor thrombus, and the resection margins were free of tumor tissue (Figure 7). The tumor stage was determined to be pT1N0M0, IB. Follow-up included liver function tests and regular CT scans, which showed no recurrence at 6 months (Figure 8).

Figure 1: Presurgical abdominal CT image of the patient. (A) An enhanced CT scan of the abdomen in the arterial phase suggests primary liver cancer in segment S8 of the liver, with unclear borders and a size of approximately 6.5 cm x 5.5 cm x 4.5 cm (Yellow arrow). (B) CT venous phase suggests that the mass was adjacent to the right hepatic vein (Blue triangle), middle hepatic vein (Blue arrow), and the root of the middle hepatic vein, with mild compression of the inferior vena cava (Blue circle). Please click here to view a larger version of this figure.
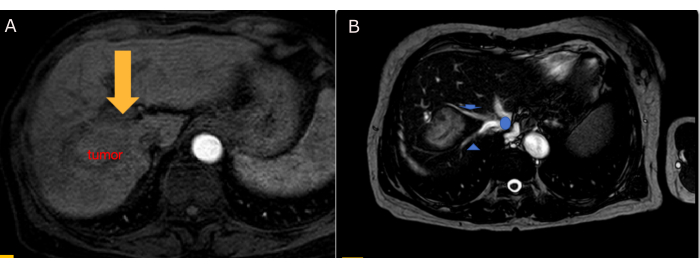
Figure 2: Post-systematic treatment abdominal EOB-MR image of the patient. (A) EOB-MR scans showed no enhancement of the tumor during the arterial phase. (B) The relationship between the tumor and the second hepatic hilum was significantly clear: right hepatic vein (Blue triangle), middle hepatic vein (Blue arrow), and inferior vena cava (Blue circle). Please click here to view a larger version of this figure.

Figure 3: Preoperative three-dimensional visualization assessment. (A) Although the tumor (Yellow arrow) was closely adjacent to the right hepatic vein (Green triangle) and middle hepatic vein (Green arrow), its relationship with the second porta hepatis was clear. (B) The relationship between the tumor (Yellow arrow) and the inferior vena cava was clear (Green circle). (C) The tumor was closely adjacent to the right anterior portal vein (Blue triangle) and right posterior portal vein (Green triangle), but it did not invade the vessels Please click here to view a larger version of this figure.
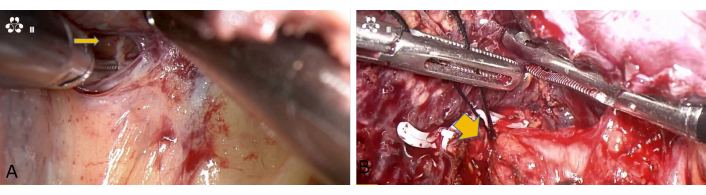
Figure 4: Dissection of the first hepatic hilum. (A) Using the Laennec membrane (Yellow arrow), separate the gate IV. (B) The right anterior lobe was separated by gate IV and gate V. Right anterior hepatic pedicle (Yellow arrow). Please click here to view a larger version of this figure.

Figure 5: Exploration of the tumor. (A) The tumor (Yellow arrow) was close to the middle hepatic vein (Green arrow) but did not invade the vein. (B The tumor (Yellow arrow) was close to the right hepatic vein (Green triangle) but did not invade the vein. (C) The middle hepatic vein (Green arrow) and right hepatic vein (Green triangle) were completely preserved. Please click here to view a larger version of this figure.
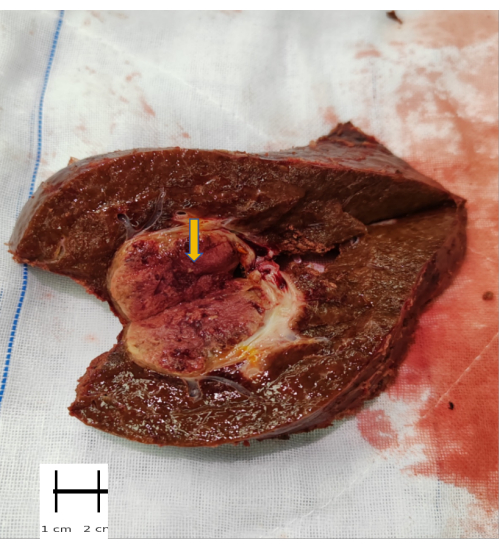
Figure 6: Excised specimen. The excised specimen includes the tumor (Yellow arrow), segments 5 and segments 8 Please click here to view a larger version of this figure.

Figure 7: Postoperative histopathological examination. Histopathological analysis of paraffin-embedded tissue sections showed moderately to poorly differentiated hepatocellular carcinoma, with approximately 76% of the cancer tissue being completely necrotic. (A) Stained tissue samples at 100 µm. (B) Stained tissue samples at 50 µm. Please click here to view a larger version of this figure.
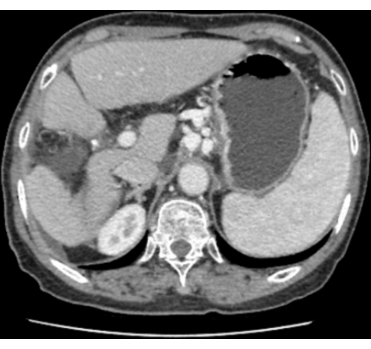
Figure 8: Postoperative CT scan. Demonstrated the successful removal of the tumor without significant recurrence or metastasis. Please click here to view a larger version of this figure.
| Operation time (min) | 240 | |
| Intraoperative blood loss (mL) | 200 | |
| First flatus (h) | 24 | |
| First postoperative liquid diet (days) | 1 | |
| Postoperative hospital stay (days) | 7 | |
| Postoperative complications (yes/no) | no | |
| Bleeding (yes/no) | no | |
| Bile leakage (yes/no) | no | |
| Abdominal infection (yes/no) | no | |
| Incision infection (yes/no) | no | |
| Pathological result | hepatocellular carcinoma | |
| Differentiation | Moderately to poorly | |
| TNM stage | pT1bN0M0 | |
| AJCC stag | IB | |
Table 1: Surgical outcomes of the patient.
Discussion
This paper demonstrates the efficacy of a multimodal treatment approach for a patient with stage IB hepatocellular carcinoma (HCC; AJCC staging: T1bN0M0). The tumor, initially measuring 6.5 cm x 5.5 cm, was closely associated with critical vascular structures, including the second hepatic hilum, inferior vena cava, right hepatic vein, middle hepatic vein, right anterior branch of the portal vein, right posterior branch of the portal vein. Given the tumor's challenging location, a comprehensive treatment strategy was necessary to optimize the patient's outcome.
In liver tumor surgery, when the tumor is closely adherent to major blood vessels such as the right hepatic vein, middle hepatic vein, and right anterior/posterior branches of the portal vein, it presents significant challenges. These blood vessels play crucial roles in liver blood supply, and their injury can lead to severe bleeding, potentially impacting liver function and increasing postoperative complications. Therefore, careful management of the tumor's relationship with these blood vessels is essential.
Since the tumor is located near critical vessels like the right hepatic vein, middle hepatic vein, and right anterior/posterior portal veins, the surgeon must ensure accurate identification and marking of these blood vessels to avoid injury. When the tumor is closely connected to major blood vessels, controlling liver blood flow is critical to preventing massive intraoperative bleeding. By applying the Pringle maneuver (temporary clamping of the hepatic artery and portal vein), the liver's blood supply can be effectively controlled, reducing bleeding during liver resection. Clamping the portal vessels for 15 min followed by a 5 min reperfusion interval helps minimize intraoperative bleeding and ensure surgical safety.
When the tumor is in close proximity to blood vessels, fine dissection techniques are paramount. Surgeons should avoid using overly aggressive energy devices that could cause unnecessary vessels and liver damage. When performing liver resection, especially if the tumor is tightly adherent to the middle hepatic vein or right hepatic vein, surgeons must take great care to avoid unintentional vessel injury. During liver resection, particularly at the junction of the right anterior lobe and the right hepatic vein, surgeons should carefully isolate liver tissue from vessels, ensuring the vessels remain intact to prevent serious bleeding. Close attention should be paid when approaching major vessels, using a combination of clamps, suction, and cutting devices for meticulous dissection.
Postoperative vascular injury and bleeding are significant complications, especially when the tumor is in close contact with major blood vessels. Close monitoring of liver function, bleeding, and potential bile leaks or other complications is essential after surgery. If bleeding or other complications arise, immediate corrective measures should be taken to prevent the worsening of the situation. When a tumor is in close contact with important liver blood vessels, the difficulty of the surgery increases significantly. Accurate preoperative assessment, real-time intraoperative imaging guidance, careful vascular dissection and resection, blood flow control (such as the Pringle maneuver), and fine liver resection techniques are key to performing the surgery successfully. By combining various technical approaches, surgeons can effectively minimize bleeding and complications, ensuring the safety and precision of liver surgery.
Initial management involved targeted therapy, immunotherapy, and hepatic arterial infusion chemotherapy (HAIC), which collectively contributed to a significant reduction in tumor size to 4.5 cm x 3.1 cm after two cycles of treatment. This reduction in size not only made the tumor more amenable to surgical resection but also minimized the risks associated with operating near vital vascular structures12,13.
The surgical approach was guided by the Laennec capsule concept, which emphasizes meticulous anatomical dissection within the hepatic capsule13,14,15. This technique was pivotal in managing the complex vascular anatomy surrounding the tumor, particularly in delineating the tumor's relationship with the right hepatic vein, middle hepatic vein, right anterior branch of the portal vein, and right posterior branch of the portal vein. Despite the tumor's proximity to these vessels, the use of the Laennec capsule concept facilitated a clear dissection plane, ensuring a safe and effective resection115,16,17.
The laparoscopic anatomical right anterior sectionectomy, performed with the Laennec capsule technique, was completed in 240 min with a total blood loss of 200 mL. The surgical margins were negative, and the patient experienced no postoperative complications, demonstrating the feasibility and safety of this approach for complex HCC cases. The patient was discharged on the 8th postoperative day, further highlighting the efficacy of this surgical strategy.
This paper underscores the importance of a multidisciplinary approach in managing complex HCC cases. The integration of targeted therapy, immunotherapy, and HAIC provided a synergistic effect that not only reduced the tumor size but also facilitated a successful surgical outcome17,18,19,20. Additionally, the Laennec capsule concept proved to be a valuable technique in managing challenging hepatic resections, offering precise dissection and improved safety profiles16,17. However, the Laennec capsule technique is not without its limitations. One potential drawback is the requirement for a high level of expertise and familiarity with the anatomical landmarks, as misidentifying the capsule or adjacent structures could lead to complications. Moreover, this technique might not be suitable for all patients, particularly those with extensive tumor involvement or poor liver function, where more aggressive surgical approaches may be necessary21.
The successful outcome reflects the potential benefits of combining advanced medical therapies with innovative surgical techniques. Future research should continue to explore and refine these multidisciplinary approaches to enhance the management of HCC, particularly in cases involving complex anatomical considerations.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This study was supported by the Guangdong Medical Science and Technology Research Fund (Grant No. B2022197).
Materials
| Name | Company | Catalog Number | Comments |
| Absorbable Suture (Vicryl) | Johnson & Johnson | V-348 | |
| Anesthesia Gas (N2O + O2) | Airgas | N2O/O2 | |
| General Anesthesia Drugs | Roche | Propofol | |
| Non-absorbable Suture (Prolene) | Ethicon | PROLENE 8698 | |
| Povidone Iodine Solution | Betadine | BP-500 | |
| Surgical Forceps | Surgical Instruments | SIC-925 | |
| Surgical Scissors | Aesculap | KLS Martin 5245 | |
| Surgical Sterile Drapes | 3M | Surgical Drapes | |
| Titanium Clips | Medtronic | Endo GIA | |
| Ultrasonic Scalpel | Ethicon | Harmonic ACE+ |
References
- Bray, F. et al . Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 68 (6), 394-424 (2018).
- Chen, W. et al. Cancer statistics in China, 2015. CA Cancer J Clinicians. 66 (2), 115-132 (2016).
- Llovet, J. M. et al. Hepatocellular carcinoma. Nat Rev Disease Primers. 7 (1), 6 (2021).
- Finn, R. S. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. New Engl J Med. 382 (20), 1894-1905 (2020).
- El-Khoueiry, A. B. et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): An open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 389 (10088), 2492-2502 (2017).
- Aoki, T. et al. Anatomical liver resection: A novel concept and detailed technical aspects. Ann Surg. 271 (2), e13-e16 (2020).
- Kiguchi, G. et al. Use of the inter-Laennec approach for laparoscopic anatomical right posterior sectionectomy in semi-prone position. Surg Oncol. 29, 140-141 (2019).
- Amin, M. B. et al. AJCC Cancer Staging Manual. Springer International Publishing (2017).
- Kudo, M. et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomized phase 3 non-inferiority trial. Lancet. 391 (10126), 1163-1173 (2018).
- Lu, Y. et al. The clinical development of tislelizumab in the treatment of cancers: A comprehensive review. Biol Targets Ther. 14, 39-48 (2020).
- Lammer, J., Malagari, K., Vogl, T. Local therapies for liver tumors: Status and perspectives. J Hepatol. 62 (5), 1377-1389 (2015).
- He, M. K. et al. Lenvatinib, toripalimab, plus hepatic arterial infusion chemotherapy versus lenvatinib alone for advanced hepatocellular carcinoma. Ther Adv Med Oncol. 13, 17588359211002720 (2021).
- Jiao, S. C. et al. Clinical activity and safety of penpulimab (Anti-PD-1) with anlotinib as first-line therapy for advanced hepatocellular carcinoma (HCC). J Clin Oncol. 38 (suppl 15), 4592-4592 (2020).
- Sugioka, A., Kato, Y., Tanahashi, Y. Systematic extrahepatic Glissonean pedicle isolation for anatomical liver resection based on Laennec's capsule: Proposal of a novel comprehensive surgical anatomy of the liver. J Hepato-Biliary-Pancreatic Sci. 24 (1), 17-23 (2017).
- Hayashi, S. et al. Connective tissue configuration in the human liver hilar region with special reference to the liver capsule and vascular sheath. J Hepato-Biliary-Pancreatic Surg. 15 (6), 640-647 (2008).
- Kiguchi, G. et al. Laparoscopic S7 segmentectomy using the inter-Laennec approach for hepatocellular carcinoma near the right hepatic vein. Surg Oncol. 31, 132-134 (2019).
- Hu, Y. et al. Laennec's approach for laparoscopic anatomic hepatectomy based on Laennec's capsule. BMC Gastroenterol. 19 (1), 194 (2019).
- Yarchoan, M. et al. Feasibility and efficacy of neoadjuvant cabozantinib and nivolumab in patients with borderline resectable or locally advanced hepatocellular carcinoma (HCC). J Clin Oncol. 39 (suppl 3), 335 (2021).
- Zhang, W. et al. A real-world study of PD-1 inhibitors combined with TKIs for HCC with major vascular invasion as the conversion therapy: A prospective, non-randomized, open-label cohort study. Ann Oncol. 31 (suppl 6), 1307 (2020).
- He, M. et al. Sorafenib plus hepatic arterial infusion of oxaliplatin, fluorouracil, and leucovorin vs sorafenib alone for hepatocellular carcinoma with portal vein invasion: A randomized clinical trial. JAMA Oncol. 5 (7), 953-960 (2019).
- Zhang, X., Tan, Z., Li, W. Challenges in laparoscopic liver resection: Review of techniques and limitations in patients with complex tumors. Hepatol Intl. 14 (2), 225-233 (2020).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved