Case Report
Management of Failed Latarjet and Off-tract Hill-Sachs Lesion: Arthroscopy-assisted Remplissage and Open Eden-Hybinette Procedure
In This Article
Summary
Here, we describe a modified technique for arthroscopy-assisted Remplissage and open Eden-Hybinette procedure for patients with failed Latarjet and off-tract Hill-Sachs lesions.
Abstract
This case report describes a 49-year-old former semi-professional judo player with recurrent right shoulder instability following his first dislocation in 2006. He underwent two unsuccessful arthroscopic Bankart repairs due to improper anchor positioning. In March 2020, an open Latarjet procedure was performed to address his ongoing instability, but he suffered another dislocation in January 2023 after a fall. Physical examination revealed a full range of motion, normal rotator cuff strength, and a positive apprehension test. X-rays showed a broken coracoid bone block, screw displacement, and a significant Hill-Sachs lesion. CT confirmed resorption of the previous coracoid graft and an off-track Hill-Sachs lesion. The patient underwent revision surgery, combining an arthroscopic-assisted Remplissage with an Eden-Hybinette procedure. One year postoperatively, the patient reported improved outcomes. Managing recurrent shoulder instability after failed surgeries is challenging. While the Latarjet procedure has a 10% recurrence rate, revision options such as distal tibial allograft and Eden-Hybinette procedures offer promising results. This case emphasizes the importance of combined surgical approaches and individualized treatment plans, particularly for patients with significant humeral bone loss, to enhance stability and reduce recurrent instability.
Introduction
Recurrent shoulder instability is a demanding condition, especially in patients with previous surgical interventions1,2,3. Soft tissue procedures such as Bankart repair, capsulorrhaphy, Remplissage, and bony procedures such as Eden-Hybinette4, Trillat5, Bristow6, and Latarjet procedure7,8,9,10 were developed. However, there are still reports for failed Latarjet procedure necessitating alternative revision surgical strategies11,12. This case study describes a patient with a failed Latarjet procedure managed with an arthroscopy-assisted Remplissage and open Eden-Hybinette procedure. The objective is to explore the details of surgical technique, rationale, and outcomes of this combined approach.
CASE PRESENTATION
A 49-year-old male, a previous semi-professional Judo player with an ISI score13 10 of 5, presented with recurrent right shoulder instability following his first-time dislocation in 2006 after a fall on the stairs. He underwent two failed arthroscopic Bankart repairs in 2006 and 2007 with an imperfect anchor position. Due to the unsolved condition, he underwent an open Latarjet procedure in March 2020. Figure 1 demonstrated the preoperative and postoperative X-ray following Latarjet procedure. In January 2023, the patient experienced another fall from multiple stairs, resulting in a dislocation of the right shoulder again.
Diagnosis, assessment, and plan
He returned to our outpatient clinic for follow-up. During the physical examination, he demonstrated a full shoulder range of motion (ROM), a normal strength of the rotator cuff, and no signs of scapular dyskinesis or hyperlaxity; all neurovascular exams were within normal limits. The apprehension test was positive, and the sulcus sign was grade 1. X-rays revealed a breakage of the coracoid bone block and screw displacement around the axillary pouch, and a huge Hill-Sachs lesion (HSL) (Figure 2A,B). The computer tomography (CT) imaging confirmed their resorption of the previous coracoid grafts and an off-track HSL as the size of the HSL was 44.5 units which is larger than the glenoid tract of 43.4 units (Figure 2C,D). Due to the repeated positive apprehension, the patient underwent revision surgery, which included an arthroscopy-assisted Remplissage procedure14 to address the HSL and open Eden-Hybinette procedure4 with autologous iliac crest grafting, secured with two cannulated screws. Loose screws from previous surgeries were removed.
Protocol
This study was approved by the Ethics Committee of our institution and informed consent was obtained from the patient.
- Put the patient in a beach chair position with an arm holder under general anesthesia and interscalene nerve block.
- Create posterior, posterolateral, anterior, and anterolateral portals with a No. 11 blade (Figure 3A).
- Perform a thorough arthroscopic exam with a 4-mm, 30-degree-angled arthroscope to define the location of the Hill-Sachs lesion from the anterior portal.
- Clean the subacromial bursae with a 5.5 mm shaver blades. Shuttle the arthroscope through the anterolateral portal to evaluate the size of the Hill-Sachs lesion intraarticularly (Figure 3B).
- Debride the exposed proximal humerus bone bed (Figure 3C).
- Insert an all-suture Y-Knot RC anchor at the deepest part of the Hill-Sachs lesion (Figure 3D).
- Make three mattress sutures by piercing the musculotendinous junction of the infraspinatus tendon with the birdbeak suture passer (Figure 3E).
NOTE: Do not tie the knots until the completion of the open Eden-Hybinette procedure (Figure 3F). - For the open Eden-Hybinette procedure, perform the deltopectoral approach along the previous wound.
- Define the subscapularis through the deltopectoral interval and split the lower third of the musculotendinous junction of the subscapularis.
- Vertically cut the capsule and expose the anterior glenoid.
- Remove previous loose screws (Figure 4A).
- Use a burr to create a flat bleeding surface on the anterior glenoid for graft placement.
- Harvest a 3 cm x 1 cm x 1.5 cm tricortical iliac crest autograft (Figure 4B,C) from a 5 cm incision
- Secure the tricortical iliac crest autograft with two 4.5 mm cannulated screws (Figure 4D).
- Confirm the graft is flush to the glenohumeral joint line under arthroscopy (Figure 4G).
- After the open procedure, tie the Remplissage knots.
- Introduce the arthroscope into the glenohumeral joint to confirm the filling of the Hill-Sachs lesion (Figure 3H).
- Make sure the tricortical iliac crest bone graft is flush with the anterior glenoid (Figure 3H).
2. Rehabilitation
- Immobilize the operated arm with a sling for the first 2-3 weeks.
- Instruct the patient to gradually resume activities as long as they do not trigger pain.
- Educate the patient on a home-based, self-rehabilitation exercises since the first postoperative day, followed by the protocol designed by a sports physician15.
- Allow return to sports and strengthening exercises by an experienced physiotherapist 3 months after surgery.
Results
One year postoperatively, the patient's reported outcomes showed significant improvements. The Oxford Shoulder Instability Score improved from 26 to 54, the QuickDASH score decreased from 63.6 to 11.4, and the WOSI score dropped from 78.4 to 15.1. One-year postoperative X-rays showed full incorporation of the bone graft without evidence of osteolysis (Figure 5A). A computer tomography scan was performed 12 months postoperatively to evaluate the bone union between the graft and host bone (Figure 5B).

Figure 1: X-rays of the patient before and after the Latarjet procedure. (A) Anteroposterior view X-ray before, (B) axillary view X-ray before, (C) anteroposterior view X-ray after, and (D) axillary view X-ray after the procedure. (A,B) The previous anchor position was too high before the procedure. (C,D) After the open Latarjet procedure, the two cannulated screws were used to fix the coracoid autograft. Please click here to view a larger version of this figure.

Figure 2: X-rays and computer tomography imaging following the failed Latarjet procedure. (A) Anteroposterior X-ray. The two compression screws were dislodged at the axillary pouch (arrowhead). A huge Hill-Sachs lesion (arrow) was observed both in the AP and axillary view with anterior subluxation of the humerus. (B) Axillary X-ray of the patient following the dislocation of the Latarjet procedure. (C) The resorption of the previous coracoid graft and (D) an off-track bipolar lesion were observed in the CT scan. Please click here to view a larger version of this figure.
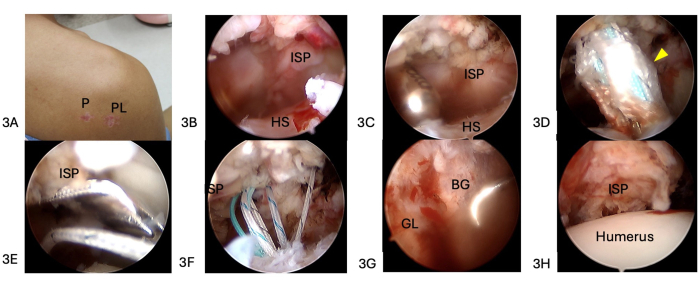
Figure 3: The arthroscopy-assisted Remplissage procedure. (A) Posterior, posterolateral, anterior, and anterolateral portals are made. (B) The arthroscope was shuttled through the anterolateral portal to evaluate the size of the Hill-Sachs lesion intraarticularly. (C) Debridement of the exposed proximal humerus bone bed. (D) An all-suture Y-Knot RC anchor (arrowhead) was inserted at the deepest part of the Hill-Sachs lesion. (E) Three mattress sutures were made by piercing the the musculotendinous junction of the infraspinatus tendon with the birdbeak suture passer. (F) The knots were not tied until the completion of the open Eden-Hybinette procedure. (G) The confirmation of the Remplissage procedure filling of the Hill-Sachs lesion. (H) Flush of the iliac crest bone graft onto the anterior glenoid. Abbreviations: P = posterior; PL = posterolateral; HS = Hill-Sachs; ISP = infraspinatus; GL = glenoid; BG = bone graft. Please click here to view a larger version of this figure.

Figure 4: The open Eden-Hybinette procedure. (A) Remove previous loose screws. (B,C) A 3 cm x 1 cm x 1.5 cm iliac crest autograft was harvested. (D) Secure the iliac autograft with two 4.5 mm cannulated screws. Please click here to view a larger version of this figure.

Figure 5: Postoperative X-ray and computed tomography at one-year follow-up showed a reduced joint line and full incorporation of the bone graft. (A) Anteroposterior X-ray. (B) Axial view of the computed tomography demonstrated the full incorporation of the tricortical iliac crest bone graft. Please click here to view a larger version of this figure.
Discussion
Decision-making following a failed Latarjet procedure
Numerous studies have confirmed the efficacy of the Latarjet procedure in treating recurrent anterior shoulder instability16. Despite the generally high success rates, there remains a possibility of recurrent instability following the procedure17,18,19. Previous research has reported recurrence and reoperation rates around 10%20,21,22.
Failure in Latarjet procedure is characterized by the recurrence of shoulder dislocation or subluxation, nonunion, malposition, or resorption of the coracoid bone block19,23,24. Additionally, issues such as symptomatic hardware, a painful or unstable shoulder, and the onset or worsening of glenohumeral osteoarthritis may also occur22,25,26. These complications often necessitate revision surgery. Several studies have also highlighted that athletes under 20 years old,27 participating in contact sports, and having a concomitant HSL can increase the likelihood of recurrence following open stabilization and other bony augmentation procedures28,29,30.
Previous literature has proposed several graft options, including the iliac crest (Eden-Hybinette procedure)31, distal clavicle32, distal tibia allograft33, and scapular spine34. The tricortical iliac crest autograft is a viable graft option for revision glenoid reconstruction after a failed Latarjet procedure35. The anterior superior iliac spine (ASIS) autograft offers substantial bone stock and abundant cancellous bone, promoting successful union. Its dense cortical structure further supports its suitability for revisional glenoid bone augmentation30,36.
A recent meta-analysis18 reviewing treatment options for recurrent instability after a failed Latarjet procedure concluded that the Eden-Hybinette procedure is the most popular and safest option. This procedure has demonstrated good to excellent clinical outcomes and satisfaction rates, ranging from 67% to 89%18. The Eden-Hybinette procedure is preferred by most orthopedic surgeons, especially when failure is attributed to complications with the coracoid graft. The study also found that revision procedures, such as the Eden-Hybinette, had similar rates of major postoperative complications to those of initial Latarjet procedures, with both being relatively low. The meta-analysis18 reported a recurrence rate of instability at 8.6%37,38 following these revision procedures. Therefore, according to our analysis, the Eden-Hybinette procedure is considered the most rational choice for addressing a failed Latarjet procedure.
Rationale for combining the free bone block procedure with Remplissage
Since Itoi et al.39 introduced the concept of on-track and off-track lesions, numerous researchers have focused on this topic, developing various solutions40. One such approach is the Remplissage procedure41,42, which is used to address bony defects in the humerus.
A systematic review41 of the Remplissage procedure concluded that, from a biomechanical perspective, the arthroscopic Remplissage procedure consistently prevents engagement of the HSL43,44,45. However, while the potential impact of the Remplissage procedure on the shoulder's range of motion is a concern, there are still debates from studies to substantiate this concern46,47. While the free bone block (FBB) procedure is effective at reducing the recurrence of glenohumeral instability, a subset of patients with significant humeral bone loss remains at risk for recurrent instability, even when the length of the glenoid track is increased.
Calvo et al.48 reported that 11.8% of patients with bipolar bone loss had remaining off-track lesions at a 2-year follow-up after undergoing an arthroscopic Latarjet procedure. Patients with a persistent off-track lesion were found to be at a higher risk of experiencing recurrent subluxations49. This highlights that patients with HSL may require additional procedures to address their humeral bone loss despite having undergone an FBB procedure. Abboud et al. also reported that patients treated with a combined open Latarjet and arthroscopic Remplissage in their group had good to excellent patient-reported outcomes, without recurrent dislocations50. Lin et al. developed the PIT Risk Score, which considers significant prognostic factors for recurrent shoulder instability following primary arthroscopic Bankart repair and evaluates the role of Remplissage augmentation for on-track shoulders based on a patient's risk profile. They found that when the Bankart repair was augmented with Remplissage, it decreased 10 points of PIT Risk Score, making patients with extreme risk to a moderate risk. Thus, it is reasonable to combine a FBB procedure with Remplissage in patients undergoing revision for off-track shoulder instability.
The importance of sling effect in revision surgeries
Tricortical Iliac crest graft reconstruction is less advantageous than coracoid transfer biomechanically due to the absence of the 'sling effect. However, tricortical iliac crest grafts have been reported to effectively restore stability in high-risk populations and as a revision technique following failed Latarjet procedures35. Studies have shown that the outcomes of grafts mentioned above are comparable to those of the Latarjet procedure, raising questions about the necessity of the 'sling effect' when addressing bone loss31,51.
According to Callegari et al.52, incorporating Remplissage with an FBB procedure minimized translation, bringing it closer to the intact condition, and increased the force required for dislocation compared to using only a FBB or the Latarjet procedure in a bipolar bone loss model with an off-track HSL. In a similar vein, Hartzler et al.52 highlighted the importance of the Remplissage procedure for off-track lesions, particularly in the context of the engagement patterns of HSLs with a 15% glenoid defect. A systematic review53 found no differences in recurrent instability, progression of osteoarthritis, complication rates, or return to sport between the Latarjet and FBB groups. In the current study, adding a Remplissage to an FBB procedure led to comparable resistance to translation and the highest force required to dislocate the glenohumeral joint. Although Remplissage has not traditionally been augmented with a FBB procedure, its addition may increase the stiffness of the construct and the requirement of a higher force to cause further dislocation, which may help reduce the rate of recurrent instability, especially in cases where a previous Latarjet procedure has failed.
To our knowledge, previous literature discussing failed Latarjet procedures lacks consensus18, likely due to the low failure rate and the absence of an agreed-upon revision method. We present this case report to demonstrate that the FBB procedure combined with arthroscopic Remplissage is feasible and results in favorable clinical outcomes.
Recurrent shoulder instability post Latarjet procedure presents a significant challenge. The combination of the arthroscopy-assisted Remplissage and open Eden-Hybinette procedure offers a viable alternative for patients with significant bone loss and failed previous surgeries. This case underscores the importance of tailored surgical strategies to optimize outcomes in complex shoulder instability cases.
Disclosures
The authors have no conflicts of interest to declare.
Acknowledgements
The authors gratefully thank the Taiwan Minister of Science and Technology and Linkou Chang Gung Memorial Hospital for the financial support of this study (Grant: MOST 111-2628-B-182A-016, NSTC112-2628-B-182A-002, CMRPG5K0092, CMRPG3M2032, CMRPG5K021, SMRPG3N0011)
Materials
| Name | Company | Catalog Number | Comments |
| 4 mm, 30°-angled arthroscope | Stryker Endoscopy, Michigan, USA | For arthroscopic visualization | |
| 4.5 mm cannulated screws | Synthes, Switzerland | For graft fixation | |
| 5.5 mm shaver blades, Dyonics | Smith & Nephew, Andover, MA | For arthroscopic debridement | |
| Y-Knot RC all-suture anchor | ConMed Linvatec, Largo, FL | Triple-loaded all suture anchors. Increase the repair area of Remplissage procedure |
References
- Barlow, J. D., Grosel, T., Higgins, J., Everhart, J. S., Magnussen, R. A. Surgical treatment outcomes after primary vs recurrent anterior shoulder instability. J Clin Orthop Trauma. 10 (2), 222-230 (2019).
- Novakofski, K. D. et al. Nonoperative management of anterior shoulder instability can result in high rates of recurrent instability and pain at long-term follow-up. J Shoulder Elbow Surg. 31 (2), 352-358 (2022).
- Lau, B. C. et al. Surgical treatment for recurrent shoulder instability: Factors influencing surgeon decision making. J Shoulder Elbow Surg. 30 (3), e85-e102 (2021).
- Flurin, P. H., Antoni, M., Métais, P., Aswad, R. Revision of failed Latarjet with the Eden-Hybinette surgical technique. Orthop Traumatol Surg Res. 106 (2), 223-227 (2020).
- Gerber, C., Terrier, F., Ganz, R. The trillat procedure for recurrent anterior instability of the shoulder. J Bone Joint Surg Br. 70 (1), 130-134 (1988).
- Longo, U. G. et al. Latarjet, Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: Systematic review and quantitative synthesis of the literature. Arthroscopy. 30 (9), 1184-1211 (2014).
- Brophy, R. H. Marx, R. G. The treatment of traumatic anterior instability of the shoulder: Nonoperative and surgical treatment. Arthroscopy. 25 (3), 298-304 (2009).
- Shaha, J. S. et al. Redefining "critical" bone loss in shoulder instability: Functional outcomes worsen with "subcritical" bone loss. Am J Sports Med. 43 (7), 1719-1725 (2015).
- Shanley, E. et al. Return to sport as an outcome measure for shoulder instability: Surprising findings in nonoperative management in a high school athlete population. Am J Sports Med. 47 (5), 1062-1067 (2019).
- Allain, J., Goutallier, D., Glorion, C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 80 (6), 841-852 (1998).
- Domos, P., Lunini, E., Walch, G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 10 (1), 15-24 (2018).
- Delgado, C., Valencia, M., Martínez-Catalán, N., Calvo, E. Management of the failed Latarjet procedure. J Shoulder Elbow Surg. 33 (12), 2859-2866 (2024).
- Balg, F. Boileau, P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 89 (11), 1470-1477 (2007).
- Wolf, E. M. Arianjam, A. Hill-Sachs Remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg. 23 (6), 814-820 (2014).
- Roulet, S. et al. Immediate self-rehabilitation after open Latarjet procedures enables recovery of preoperative shoulder mobility at 3 months. Knee Surgery, Sports Traumatology, Arthroscopy. 27 (12), 3979-3988 (2019).
- Khan, U., Torrance, E., Hussain, M., Funk, L. Failed Latarjet surgery: Why, how, and what next? JSES Int. 4 (1), 68-71 (2020).
- Tytherleigh-Strong, G. M. Morrissey, D. I. Failed Latarjet procedure treated with a revision bone block stabilization using a suture-button fixation. J Shoulder Elbow Surg. 26 (4), e102-e107 (2017).
- Buda, M. et al. Failed Latarjet procedure: A systematic review of surgery revision options. J Orthop Traumatol. 22 (1), 24 (2021).
- Provencher, M. T. et al. Management of the failed Latarjet procedure: Outcomes of revision surgery with fresh distal tibial allograft. Am J Sports Med. 47 (12), 2795-2802 (2019).
- Ferlic, D. C. Digiovine, N. M. A long-term retrospective study of the modified Bristow procedure. Am J Sports Med. 16 (5), 469-474 (1988).
- An, V. V., Sivakumar, B. S., Phan, K., Trantalis, J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 25 (5), 853-863 (2016).
- Griesser, M. J. et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: A systematic review. J Shoulder Elbow Surg. 22 (2), 286-292 (2013).
- Di Giacomo, G. et al. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: A computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg. 20 (6), 989-995 (2011).
- Gupta, A., Delaney, R., Petkin, K., Lafosse, L. Complications of the Latarjet procedure. Curr Rev Musculoskelet Med. 8 (1), 59-66 (2015).
- Hovelius, L., Sandstrom, B., Sundgren, K., Saebo, M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: Study i--clinical results. J Shoulder Elbow Surg. 13 (5), 509-516 (2004).
- Mizuno, N., Denard, P. J., Raiss, P., Melis, B., Walch, G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg. 23 (11), 1691-1699 (2014).
- Provencher, M. T., Midtgaard, K. S., Owens, B. D., Tokish, J. M. Diagnosis and management of traumatic anterior shoulder instability. J Am Acad Orthop Surg. 29 (2), e51-e61 (2021).
- Gwathmey, F. W., Jr. Warner, J. J. Management of the athlete with a failed shoulder instability procedure. Clin Sports Med. 32 (4), 833-863 (2013).
- Schroder, D. T., Provencher, M. T., Mologne, T. S., Muldoon, M. P., Cox, J. S. The modified bristow procedure for anterior shoulder instability: 26-year outcomes in naval academy midshipmen. Am J Sports Med. 34 (5), 778-786 (2006).
- Ranalletta, M. et al. Autologous tricortical iliac bone graft for failed Latarjet procedures. Arthrosc Tech. 8 (3), e283-e289 (2019).
- Moroder, P. et al. Neer award 2019: Latarjet procedure vs. Iliac crest bone graft transfer for treatment of anterior shoulder instability with glenoid bone loss: A prospective randomized trial. J Shoulder Elbow Surg. 28 (7), 1298-1307 (2019).
- Kwapisz, A., Fitzpatrick, K., Cook, J. B., Athwal, G. S., Tokish, J. M. Distal clavicular osteochondral autograft augmentation for glenoid bone loss: A comparison of radius of restoration versus Latarjet graft. Am J Sports Med. 46 (5), 1046-1052 (2018).
- Provencher, M. T., Ghodadra, N., Leclere, L., Solomon, D. J., Romeo, A. A. Anatomic osteochondral glenoid reconstruction for recurrent glenohumeral instability with glenoid deficiency using a distal tibia allograft. Arthroscopy. 25 (4), 446-452 (2009).
- Kuan, F.-C. et al. Morphometric and biomechanical comparison of the scapular spine and coracoid graft in anterior shoulder instability. American J Sports Med. 50 (13), 3625-3634 (2022).
- Mittal, R. Jain, S. Eden-Hybinette procedure for revision surgery in recurrent anterior shoulder instability in epilepsy. Indian J Orthop. 55 (3), 728-733 (2021).
- Auffarth, A. et al. The J-bone graft for anatomical glenoid reconstruction in recurrent posttraumatic anterior shoulder dislocation. Am J Sports Med. 36 (4), 638-647 (2008).
- Willemot, L. et al. Analysis of failures after the Bristow-Latarjet procedure for recurrent shoulder instability. Int Orthop. 43 (8), 1899-1907 (2019).
- Lunn, J. V., Castellano-Rosa, J., Walch, G. Recurrent anterior dislocation after the Latarjet procedure: Outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elbow Surg. 17 (5), 744-750 (2008).
- Itoi, E. 'On-track' and 'off-track' shoulder lesions. EFORT Open Rev. 2 (8), 343-351 (2017).
- Hurley, E. T. et al. Anterior shoulder instability part II-Latarjet, Remplissage, and glenoid bone-grafting-an international consensus statement. Arthroscopy. 38 (2), 224-233.e226 (2022).
- Lazarides, A. L., Duchman, K. R., Ledbetter, L., Riboh, J. C., Garrigues, G. E. Arthroscopic Remplissage for anterior shoulder instability: A systematic review of clinical and biomechanical studies. Arthroscopy. 35 (2), 617-628 (2019).
- Hurley, E. T. et al. Remplissage for anterior shoulder instability with Hill-Sachs lesions: A systematic review and meta-analysis. J Shoulder Elbow Surg. 29 (12), 2487-2494 (2020).
- Werner, B. C. et al. Medial posterior capsular plication reduces anterior shoulder instability similar to Remplissage without restricting motion in the setting of an engaging Hill-Sachs defect. Am J Sports Med. 45 (9), 1982-1989 (2017).
- Garcia, G. H. et al. Biomechanical comparison of acute Hill-Sachs reduction with Remplissage to treat complex anterior instability. J Shoulder Elbow Surg. 26 (6), 1088-1096 (2017).
- Degen, R. M., Giles, J. W., Johnson, J. A., Athwal, G. S. Remplissage versus Latarjet for engaging Hill-Sachs defects without substantial glenoid bone loss: A biomechanical comparison. Clin Orthop Relat Res. 472 (8), 2363-2371 (2014).
- Buza, J. A., 3rd, Iyengar, J. J., Anakwenze, O. A., Ahmad, C. S., Levine, W. N. Arthroscopic Hill-Sachs Remplissage: A systematic review. J Bone Joint Surg Am. 96 (7), 549-555 (2014).
- Nourissat, G., Kilinc, A. S., Werther, J. R., Doursounian, L. A prospective, comparative, radiological, and clinical study of the influence of the "Remplissage" procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med. 39 (10), 2147-2152 (2011).
- Calvo, C., Calvo, J., Rojas, D., Valencia, M., Calvo, E. Clinical relevance of persistent off-track Hill-Sachs lesion after arthroscopic Latarjet procedure. Am J Sports Med. 49 (8), 2006-2012 (2021).
- Freshman, R., Lurie, B., Garcia, G., Liu, J. Understanding the Remplissage: History, biomechanics, outcomes, and current indications. Curr Rev Musculoskelet Med. 17 (7), 282-291 (2024).
- Abboud, J., Moussa, M. K., Boushnak, M. O., Rahal, M. J. H., Robial, N. Belt and suspender technique for bipolar bone loss in shoulder instability. JSES Rev Rep Tech. 2 (3), 354-359 (2022).
- Frank, R. M. et al. Outcomes of Latarjet versus distal tibia allograft for anterior shoulder instability repair: A matched cohort analysis. Am J Sports Med. 46 (5), 1030-1038 (2018).
- Callegari, J. J. et al. The addition of Remplissage to free bone block restores translation and stiffness compared to bone block alone or Latarjet in a bipolar bone loss model. Arthroscopy. 38 (9), 2609-2617 (2022).
- Gilat, R. et al. Outcomes of the Latarjet procedure versus free bone block procedures for anterior shoulder instability: A systematic review and meta-analysis. Am J Sports Med. 49 (3), 805-816 (2021).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved