Method Article
Combined Supine and Standing Imaging for Varicocele: An Improved Diagnostic Approach
In This Article
Summary
Varicocele relies heavily on angiographic diagnostic techniques for disease-related examination and assessment. In order to diagnose varicocele better, we combined supine and standing positions for varicocele imaging, and contrast-enhanced ultrasound is used for patients with inconspicuous reflux. This approach facilitates the early detection, diagnosis, and treatment of varicocele.
Abstract
Varicocele, one of the main diseases affecting male reproductive health, relies heavily on angiographic diagnostic techniques for disease-related examination and assessment. Traditional varicocele angiography often employs a supine position to facilitate the relaxation of the groin area muscles, the insertion of the angiography catheter, and imaging. However, the supine position may cause blood reflux, thus underestimating the clinical incidence of varicocele, particularly resulting in missed diagnoses of right-sided or bilateral varicoceles. To address this issue, this study proposes the combined use of supine and standing positions for varicocele imaging. The standing position increases lower abdominal pressure, making the degree of varicosity more prominent in the images. Compared to the sole use of the supine position, the method employed in this study effectively reduces the misdiagnosis rate of right-sided or bilateral varicoceles. This approach aims to facilitate the early detection, diagnosis, and treatment of varicocele, effectively reducing the potential threat of the disease to male reproductive health. It also helps improve the accuracy of disease assessment, providing more references for selecting subsequent treatment plans.
Introduction
Globally, infertility has gradually emerged as an issue of pressing concern for clinicians and researchers, with related disorders receiving significant attention. Among these, varicocele (VC) is considered one of the primary causes of male infertility, especially with an incidence rate reaching up to 80% in the secondary infertile population1. Accurate and timely diagnosis for such diseases is pivotal, as it directly dictates the subsequent choice of treatment and its efficacy.
The conventional diagnostic method for varicocele primarily relies on clinical manifestations and physical examinations2. Color Doppler ultrasound stands as the preferred method of diagnosis for varicocele, yet its detection rate is contingent on the examiner's experience3. In practice, many sonographers opt to conduct the examination solely in a supine position. However, compared to the standing position, the abdominal pressure is reduced in the supine position, potentially leading to overlooked or underestimated lesions4, which consequently influences treatment decisions and outcomes.
To more accurately diagnose varicocele, modern medical research has begun to explore additional diagnostic methods. Contrast-enhanced ultrasound (CEUS), a technique for assessing microvascular perfusion5, boasts superior vascular imaging capabilities and has been extensively applied to organs such as the liver6, breast7, and kidney8, but its application in varicoceles remains limited. This study proposes an innovative approach: combining imaging in both the supine and standing positions for varicocele. In a standing posture, due to increased lower abdominal pressure, varicosities appear more pronounced during imaging. In conjunction with contrast techniques, reflux in patients can be observed more directly. This method not only significantly enhances diagnostic accuracy and reduces the risk of missed diagnoses, but it also provides clinicians with a more comprehensive view of the disease, enabling more precise assessment and subsequently a more appropriate treatment plan. In summary, this study, aims to offer clinicians and researchers a novel and more effective diagnostic tool, addressing the growing public health concern of varicocele more effectively.
Protocol
This study received approval from the Shanghai Hospital of Planned Parenthood Research. The diagnostic criteria, surgical indications, and contraindications are in line with the expert consensus of the "Guidelines for Andrological Diagnostics and Treatment," the "Chinese Andrology Society," and the "European Association of Urology Sexual and Reproductive Health Guidelines." Patients with female partners suffering from diseases affecting fertility were excluded from this study. Informed consent was obtained from the patients enrolled in the study.
1. Instruments for operation
- Ensure the availability of sterilized instruments and other equipment mentioned in the Table of Materials.
2. Pre-examination preparations
- Ensure the patient is not allergic to the contrast agent.
- Configure the ultrasound settings using the ultrasound machine, i18LX5 probe, with a frequency of 5 MHz, a mechanical index of 0.07, dynamic range of 50-55 dB, base wave mode adjusted to the area of interest, and harmonic mode adjusted to below the area of interest.
3. Combined varicocele angiography examination
- Have the examinee first take a supine position (Figure 1).
- Use the probe perpendicular to the examinee's longitudinal axis to conduct a two-dimensional ultrasound scan from the external inguinal ring to the upper segment of the epididymal head.
- Fix the probe's view on the segment where the varicose veins are most prominent (Figure 2A) and click the ruler (distance) button to record the diameters of the veins on the right side (Figure 2B).
- Similarly, examine the left side spermatic veins.
- Instruct the patient to stand (Figure 3).
- Using the same method, measure the diameter of the spermatic veins on both sides.
- Press the Color Doppler ultrasound mode on the keyboard and turn on the Movie mode. Instruct the patient to take a Valsalva breath, select the red area on the screen, and record the venous reflux time (Figure 4).
- For patients with a standing spermatic vein diameter of >2.8 mm and no evident reflux during the Valsalva maneuver, proceed with internal spermatic venography.
- Disinfect the central vein of the left elbow with an alcohol cotton ball, and use a 5 mL syringe to ballistically inject 2.4 mL of contrast agent, followed by an injection of 5.0 mL of saline solution (Figure 5).
- Turn to Contrast-Enhanced ultrasound mode. Instruct the patient to take a Valsalva breath, record images in a contrast-enhanced ultrasound mode, and record the duration of backflow (Figure 6).
Results
From June 2022 to June 2023, our institution conducted a total of 2,789 testicular vein ultrasound examinations. Among them, the positive detection rate for varicocele was 84.51%. Specifically, 24.35% of the patients had unilateral (left) varicocele, 2.34% had unilateral (right) varicocele, and 73.31% had bilateral varicocele. Notably, in the supine ultrasound examination (Figure 1), approximately 48.45% of the patients did not show varicose veins on the right side of the spermatic cord (Figure 2), but varicocele on the right side was detected when standing (Figure 3), at the same time, blood reflux can be seen (Figure 4). Among all patients with varicocele, grade I° varicocele was the most common, accounting for 56.34% of the total number of patients. Furthermore, varicocele in all patients showed a worsening trend when standing. For 157 patients with grade I° or higher varicocele, due to the inconspicuous blood reflux, further angiographic tests were added (Figure 5). Among these 157 patients, 136 indeed observed reflux in the ultrasound angiographic images (Figure 6). The detailed examination data for these cases can be seen in Table 1. Additionally, 367 patients successfully underwent varicocelectomy at our institution, and the presence of varicocele was confirmed during surgery.

Figure 1: Supine position Please click here to view a larger version of this figure.

Figure 2: Detection of spermatic vein diameter. (A) Fix the probe's view on the segment where the varicose veins are most prominent. (B) Record the diameters of the veins on the right side. Please click here to view a larger version of this figure.

Figure 3: Standing position Please click here to view a larger version of this figure.
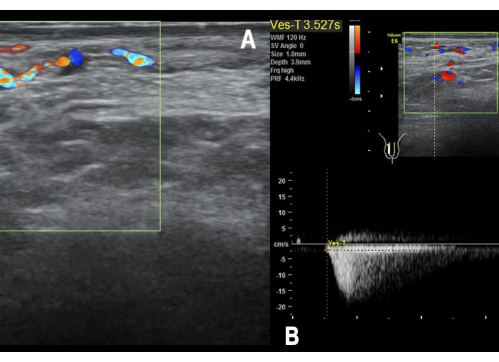
Figure 4: Venus reflux time and duration of backflow. Instruct the patient to take a Valsalva breath and (A) record the venous reflux time. The red part represents backflow. (B) Measure the duration of backflow using spectrum Doppler ultrasound. Please click here to view a larger version of this figure.

Figure 5: Contrast agent injection. Ballistically inject 2.4 mL of contrast agent. Please click here to view a larger version of this figure.
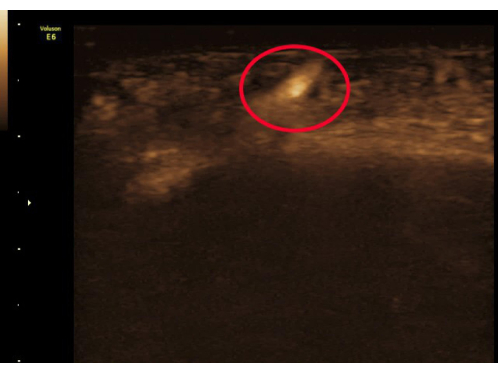
Figure 6: Recording images. Record images in a contrast-enhanced ultrasound mode and the highlighted white area indicates the presence of backflow. Please click here to view a larger version of this figure.
| Items | Value | |
| Examinations (total) (n) | 2789 | |
| Age (years), Mean ± standard deviation (range) | 32.33 ± 4.03 | |
| Varicocele patients, n (%) | 2357 (84.51%) | |
| Unilateral (left) varicocele, n (%) | 574 (24.35%) | |
| Unilateral (right) varicocele, n (%) | 55 (2.34%) | |
| Bilateral varicocele, n (%) | 1728 (73.31%) | |
| Grade I°, n (%) | 1328 (56.34%) | |
| > Grade I°, n (%) | 1029 (43.66%) | |
| Varicocele observed only in standing position, n (%) | 1142 (48.45%) |
Table 1: Characteristics of patients who underwent testicular vein ultrasound examinations.
Discussion
With the intensification of research in the realm of male reproductive health in recent years, varicocele has been recognized as one of the primary factors affecting male fertility. Although its clinical manifestations are diverse, accurate and effective diagnosis remains a pivotal step in determining therapeutic outcomes. Physical examination (PE) is extremely important in screening for varicocele; a worm-like varicose vein at the base of the scrotum can be seen in severe varicocele patients, and for mild to moderate varicocele patients, diagnosis can be made through palpation. However, a study showed that the accuracy of PE in diagnosing varicocele was 63.5%, and PE should be followed by CDU to increase diagnostic accuracy9. Scrotal ultrasound is a widely used modality for the diagnosis of varicoceles. Typical Doppler findings include venous flow at rest with intermittent or continuous flow reversal with Valsalva3. The Sarteschi and Dubin classifications are the most commonly used10,11. It is widely accepted that the progression of varicocele can lead to a decline in testicular spermatogenic function and in severe cases, even result in testicular atrophy, profoundly impairing the patient's reproductive capability12,13. Correspondingly, timely and precise early diagnosis combined with rational treatment can effectively counteract this decline in semen quality14.
While traditional supine imaging offers clinicians operational and procedural convenience, it has diagnostic limitations, especially when detecting right-sided or bilateral varicoceles, leading to potential misdiagnoses. Through our clinical observations, we found that in specific postures like the supine position, varicocele symptoms were not evident in the right spermatic vein of 1030 patients. For example, in Figure 3, the diameter of the spermatic vein is only 2 mm. However, when shifted to a standing position, these symptoms became markedly prominent (Figure 4 and Figure 6). Such diagnostic disparities induced by postural changes might be attributed to altered blood reflux and decreased intraluminal pressure in the supine posture, rendering the right varicose vein less noticeable. Furthermore, nearly all patients exhibited exacerbated varicocele severity when standing compared to the supine position. Utilizing a combined approach of supine and standing imaging not only enhances diagnostic accuracy but also aids in timely and effective assessment and treatment of varicocele, elevating the quality of medical services. This assists more patients in obtaining accurate early diagnosis and timely rational treatment, mitigating the fertility-threatening impact of the condition.
Simultaneously, contrast-enhanced ultrasound, as a technique for evaluating microvascular perfusion, has not yet been widely adopted in the diagnostic assessment of varicoceles. Conventional detection of varicocele reflux often employs color Doppler ultrasound, but this method has inherent limitations when assessing vascular reflux, particularly yielding false-negative results in scenarios of slow blood flow, thereby failing to accurately gauge the severity of varicocele. In contrast, using contrast agents, blood flow direction can be observed more clearly in contrast mode, and reflux timing can be discerned. The routine B-ultrasound phlebography for varicoceles mainly adopts the femoral vein route, which is more traumatic and less acceptable to patients. Therefore, we propose injecting the contrast agent from the left median cubital vein. This method is less invasive, more operationally convenient, and does not extend the imaging time, serving as a crucial supplementary examination for patients diagnosed with varicocele without detected reflux. This can effectively prevent erroneous evaluations of varicocele severity by physicians, which could impact subsequent treatment.
The key point of ultrasonic detection of varicocele is that the critical value of the inner diameter of the blood vessel is only for reference. The presence or absence of a reflux signal is an important basis for establishing the diagnosis. Therefore, for patients with a wider inner diameter, if no reflux is seen, further contrast-enhanced ultrasound should be performed. It takes a certain amount of time for the contrast agent to take effect, so the test cannot be performed immediately after the injection of the contrast agent. It is usually better to perform the test 5-10 min after the injection of the contrast agent. The limitation of this study is that the patient needs to change body position, so the detection time is longer compared to other methods. In addition to this, the use of contrast agents will increase medical costs.
In summary, compared to urogenital tract infections and epididymitis, the diagnosis and treatment of varicoceles appear more intricate. Nonetheless, with advancements in medical technology and research, novel diagnostic methods and treatment strategies continue to emerge, offering a broader therapeutic spectrum for patients. The combined imaging phlebography technique explored in this study can effectively avoid misdiagnoses and undeniably provides an innovative, progressive perspective for diagnosing varicoceles, also paving the way for future research and treatment directions.
Disclosures
The author has no conflicts of interest to disclose.
Acknowledgements
None.
Materials
| Name | Company | Catalog Number | Comments |
| Dianerkang Iodophor Skin Disinfectant | Shanghai Likang Disinfectant HI-Tech Co,Lid | 31005102 | For skin disinfection and the effective iodine content is from 4.5g/L~5.5g/L |
| Disposable dressing forceps | Jiaxing Zhongxin Medical Instrument Co., Ltd | MLD-01 | Holding disinfectant cotton balls for disinfection |
| Physiological saline | Shanghai Kindly Medical Instruments Co., Ltd | 2452161324 | Used for injecting contrast agents |
| Shallow probe (high frequency) | General Electric Company | Voluson E6 | Devices for transmitting and receiving ultrasonic waves |
| Sulfur hexafluoride microbubbles for injection | BRACCO INTERNATIONAL BV | SonoVue | Improve the ultrasound echo rate of blood, thereby improving the contrast between blood and surrounding tissues |
| Ultrasonic coupling agent | Shanghai Junkang Medical Equipment Co., Ltd | DS-1 | Eliminate air gaps between the probe and the detected object, improve the transmission efficiency of ultrasound |
| Ultrasound diagnostic equipment | General Electric Company | Voluson E6 | Process and display the signal received from the probe |
| Vein Detained Needle | Shanghai Kindly Medical Instruments Co., Ltd | 60017202 | Indwelling venous channels to reduce drug leakage and save time |
References
- Alsaikhan, B., Alrabeeah, K., Delouya, G., Zini, A. Epidemiology of varicocele. Asian J Androl. 18 (2), 179-181 (2016).
- Chiba, K., Ramasamy, R., Lamb, D. J., Lipshultz, L. I. The varicocele: Diagnostic dilemmas, therapeutic challenges and future perspectives. Asian J Androl. 18 (2), 276-281 (2016).
- Belay, R. E., Huang, G. O., Shen, J. K., Ko, E. Y. Diagnosis of clinical and subclinical varicocele: How has it evolved. Asian J Androl. 18 (2), 182-185 (2016).
- Punjani, N., Wald, G., Al-Hussein Alawamlh, O., Dudley, V., Goldstein, M. Standing ultrasound adds clinical utility for the diagnosis of varicoceles. J Urol. 206 (4), 1001-1008 (2021).
- Aziz, M. U., et al. Microvascular flow imaging: A state-of-the-art review of clinical use and promise. Radiology. 305 (2), 250-264 (2022).
- Fraquelli, M., et al. Contrast-enhanced ultrasound for the diagnosis of hepatocellular carcinoma in adults with chronic liver disease. Cochrane Database Syst Rev. 9 (9), Cd013483 (2022).
- Yuan, Y., et al. Clinical value of contrast-enhanced ultrasound in breast cancer diagnosis. Comput Math Methods Med. 2022, 2017026 (2022).
- Atri, M., Jang, H. J., Kim, T. K., Khalili, K. Contrast-enhanced us of the liver and kidney: A problem-solving modality. Radiology. 303 (1), 11-25 (2022).
- Cocuzza, M. S., et al. Diagnostic accuracy of physical examination compared with color doppler ultrasound in the determination of varicocele diagnosis and grading: Impact of urologists' experience. Andrology. 8 (5), 1160-1166 (2020).
- Valentino, M., Bertolotto, M., Derchi, L., Pavlica, P. Children and adults varicocele: Diagnostic issues and therapeutical strategies. J Ultrasound. 17 (3), 185-193 (2014).
- Pauroso, S., et al. Varicocele: Ultrasonographic assessment in daily clinical practice. J Ultrasound. 14 (4), 199-204 (2011).
- Pinto, K. J., Kroovand, R. L., Jarow, J. P. Varicocele related testicular atrophy and its predictive effect upon fertility. J Urol. 152 (2 Pt 2), 788-790 (1994).
- Komiya, A., Watanabe, A., Kawauchi, Y., Fuse, H. Testicular volume discrepancy is associated with decreased semen quality in infertile japanese males with varicoceles. Reprod Med Biol. 11 (3), 117-121 (2012).
- Kavoussi, P. K., et al. The impact of ipsilateral testicular atrophy on semen quality and sperm DNA fragmentation response to varicocele repair. Asian J Androl. 23 (2), 146-149 (2021).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved