Method Article
Induction of Lumbar Disc Degeneration in Rabbits Through a Transabdominal Approach
In This Article
Summary
Here, we describe a surgical protocol using needle puncture to establish rabbit lumbar disc degeneration via a transabdominal approach. Radiological checks and histological analyses were used to confirm the successful establishment of lumbar disc degeneration.
Abstract
Lower back pain is an extremely common medical issue in populations worldwide. One of the main contributors to lower back pain is intervertebral disc (IVD) degeneration. An ideal animal model of IVD degeneration is essential to study the pathophysiology of lower back pain and investigate potential therapeutic strategies. Rabbit models are reliable, economical, and easily established animal models. The retroperitoneal approach has been widely used to induce IVD degeneration in rabbit models. However, there are reported complications associated with this technique, such as the avulsion of segmental arteries and nerve root injury. In this paper, we aim to show a surgical protocol using needle puncture to establish rabbit lumbar disc degeneration via a transabdominal approach. Consequently, radiological checks and histological analyses indicated that lumbar disc degeneration was successfully established in rabbits. This surgical protocol presents the precise location of target discs and high reproducibility of IVD degeneration models with fewer complications.
Introduction
Lower back pain (LBP) is the leading cause of disability worldwide1. Intervertebral disc (IVD) degeneration (IVDD) is one of the main causes of LBP2,3,4. IVDD is a complex and incompletely understood multifactorial process that can be accelerated by different environmental and biological factors5,6,7. The pathological changes of IVDD are characterized by a disorganized IVD structure, reduced water content in the nucleus pulposus, and degradation of the surrounding extracellular matrix8,9. IVDD animal models are important for IVD-related studies9,10,11.
So far, various IVDD animal models have been established to mimic the progression of IVDD in humans. Large animals, such as bovine, sheep, goats, canine, and primate models, share some similarities with humans in terms of disc size and the cellular composition of the degenerated disc (the absence of notochordal cells, such as sheep and goats)12. However, these large models are not commonly used because of the high cost, long experimental period, poor reproducibility, and more complicated skills required to establish degeneration in these models13. By contrast, small animal models, such as rats, mice, and rabbits, are widely used in IVD-related studies because they are easier to operate on, cost-effective, and reliable10. The disc size in a rabbit is bigger than a mouse or rat, and thus, there is more disc space for manipulation in rabbits. In addition, rabbits have a high degree of homology to human IVDs, because of the similar spinal anatomical structure (facet joints, paravertebral muscles, and ligaments)14,15. Hence, rabbits are more suitable than other small animals for the establishment of IVDD models.
IVDD animal models include mechanical models (compression, instability), structural models (injury, chemical), and animal models of spontaneous degeneration16. Rabbit IVDD models are usually created by inducing injury using two different surgical approaches - the transabdominal approach17and the retroperitoneal approach18. The retroperitoneal approach of needle puncturing the target IVDs is widely used, but this approach can cause many complications, such as the avulsion of segmental arteries and nerve root injury18,19. Here, we report a rabbit IVDD model induced by needle puncturing IVDs via a transabdominal approach, aiming to provide an easy and reproducible method for establishing IVDD in rabbits.
Protocol
The experimental protocol was approved by the Animal Care and Use Committee of Xingtai General Hospital of North China Medical Health Group (Approval number: ZCKT-2021-0009). This study used healthy skeletally mature New Zealand white rabbits (female, 1 year, 3-5 kg).
1. Pre-operative preparation
- Fast the rabbits and deprive them of water for 6-8 h before general anesthesia.
- Weigh the rabbit.
- Swab the ear with 70% ethanol using a gauze sponge.
- Apply local anesthetic cream to the ears.
- Apply pressure around the base of the ear to distend the marginal ear vein.
- Sedate the rabbits using midazolam (1-2 mg/kg) by injecting into the marginal ear vein20.
- Administer the inhalation anesthesia with a mask. Set the oxygen rate to 1 L/min and the isoflurane concentration to 4%-5% to induce anesthesia.
NOTE: To judge the depth of anesthesia, pull the animal's hind leg out straight and pinch the foot hard using the thumb and forefinger. Animals should not be operated on until the withdrawal reflex has abated21. - Maintain the isoflurane concentration at 2.5%-3.5% (depending on the rabbit's weight).
2. Intra-operative procedures
- Autoclave the surgical tools (vessel clamp/forceps, tissue scissors, stitch scissors, scalpel handle, #22 scalpel blade, double-ended handheld retractor, sterile gauze, 3-0 absorbable suture, 4-0 non-absorbable braided suture, needle holder, peanut gauze [a hand-made ball-shaped gauze], 5 mL syringe, 1 mL syringe, 16 G needle, 26 G needle, a depth of 5 mm stopper) before proceeding with the surgical procedure.
- Sterilize the operating table with 75% alcohol.
- Using an electric razor and depilatory paste, shave the region defined from the lowest rib to the iliac crest level on the ventral side of the rabbit.
NOTE: Avoid damaging the nipples. - Position the rabbit on the operating table supinely and secure the limbs.
- Take the line of the iliac crest on both sides as the midpoint and draw the line 2 cm above and below as the landmarks for the surgical incision site. Mark these landmarks with a sterile pen.
- Disinfect the skin with a povidone-iodine solution twice. Place a sterile fenestrated square drape over the surgical site and a large square drape to cover the operating table. Maintain a strict aseptic environment throughout the entire procedure.
- Inject 2 mL of 2% lidocaine subcutaneously before the surgical incision to relieve post-operative pain.
- Make the incision along the landmarks using a #22 scalpel blade, and bluntly separate the fascia, muscle, and abdominal wall using curved forceps and tissue scissors.
- Enter into the peritoneal cavity until the bladder is seen. Use the double-ended handheld retractor to pull the bladder and other intestinal cavity organs to the left carefully. Then find the bifurcation of the iliac vein, and take this as the mark point for the L5-6 disc underneath it.
NOTE: Pay attention to avoid injuring any abdominal organs, especially the intestines. - Use a finger to touch the abdominal aorta pulsating on the right side of the spine and pull the blood vessels and organs to the left.
- After manipulating the protruding disc (L5-6), incise the posterior peritoneum and then use the peanut gauze to obtuse dissect the prevertebral muscle tissue.
- To confirm the correct level of the target disc and the direction of the needle, use a 26 G needle to puncture the vertebrae next to the target disc and check this under the guidance of C-arm.
- After locating the target disc, place the 16 G needle tip parallel to both the upper and lower cartilage endplates. Then, use the needle tip to puncture the IVD center to a depth of 5 mm (using a stopper), holding for 30 s.
NOTE: Take a lumbar anteroposterior and lateral x-ray to check whether the position of the needle tip is at the center of the IVD and the direction of the needle tip is parallel to the upper and lower endplates, respectively. - Repeat the same procedure for the next L6-7 disc.
- Use warm saline to irrigate the abdominal cavity and check hemorrhaging before closing the incision.
- Perform layered closure. Use 3-0 synthetic absorbable sutures to close the fascial layer continuously. Suture the full-thickness skin by using 4-0 non-absorbable braided sutures.
- Turn off the vaporizer and stop the anesthesia. Keep the rabbit under constant observation in a metabolic cage until it can move normally.
3. Post-operative management
- Inject ceftriaxone sodium (25 mg/kg) intramuscularly immediately post-surgery.
- Allow animals to move and feed freely. Continue to observe for signs of any neurological complications, such as paralysis of the legs, problems with urination and defecation, or digestive system complications.
Results
The transabdominal approach has been validated in our previous study to create IVDD rabbit models22. X-ray and magnetic resonance imaging (MRI) were performed at the 4th, 12th, and 16th weeks postoperatively. X-ray images revealed that the height of IVD L5-6 and L6-7 gradually decreased over 16 weeks following the needle puncture surgery (Figure 1A). The DHI of the needle puncture group decreased at the 4th, 12th, and 16th weeks post-surgery compared with pre-surgery23 (p < 0.05, Figure 1B).
An MRI scan of the lumbar spine was performed to evaluate the grades of IVDD24. The MRI images displayed that the signal intensity of L5-6 and L6-7 progressively decreased over 16 weeks following the needle puncture surgery (Figure 2A). The grade of IVDD gradually increased during the follow-up (p < 0.05, Figure 2B).
Histological analyses were performed at the 16th-week post-surgery according to the histological grading scale reported previously25. As shown in Figure 3A,B, the hematoxylin and eosin (H&E) staining and Safranin O-Fast green (SO/FG) staining showed a significant difference between the needle puncture group and the sham group. In the needle puncture group, notochord cells were reduced or even disappeared. Significant proliferation of chondroblast-like cells, the folding of the annulus fibrosis, replacement of fibrocartilage cells, and surrounding osteophytes were observed; the boundary between the annulus fibrosis and nucleus pulposus was severely interrupted. In addition, the deposition of proteoglycan and Type II collagen in the nucleus pulposus decreased in the needle puncture group. Moreover, histological scores of IVD degeneration in the needle puncture group were significantly higher than those in the sham group (p < 0.05, Figure 3C).
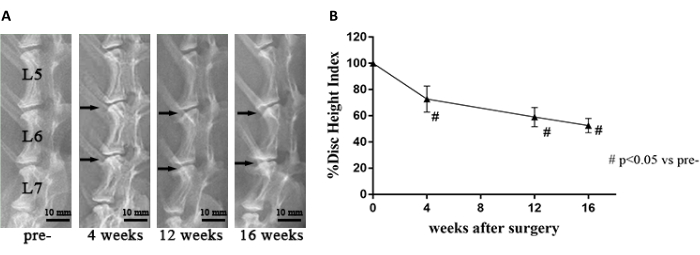
Figure 1: DHI changes of L5-6 and L6-7 in X-ray images during the 4th, 12th, and 16th weeks after the operation. (A) The needle puncture group manifests a significant narrowing of the height of IVDs at 4th week. The black arrows represent the punctured discs. (B) The disc height index (DHI) of the needle puncture group decreased gradually compared to pre-operation. # p < 0.05 vs. pre-operation (pre-). This figure has been modified with permission from Yang et al.22. Please click here to view a larger version of this figure.
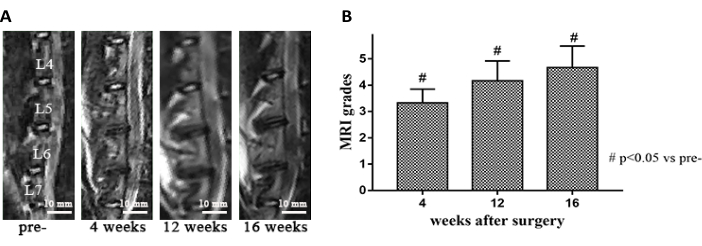
Figure 2: Pre- and post-operative MRI changes of the needle puncture group. (A) The MRI signal intensity of IVDs progressively decreased in the needle puncture group compared to pre-operation. (B) Based on MRI image analysis, the grade of intervertebral disc degeneration gradually increased. # p < 0.05 vs. pre-operation (pre-). This figure has been modified with permission from Yang et al.22. Please click here to view a larger version of this figure.
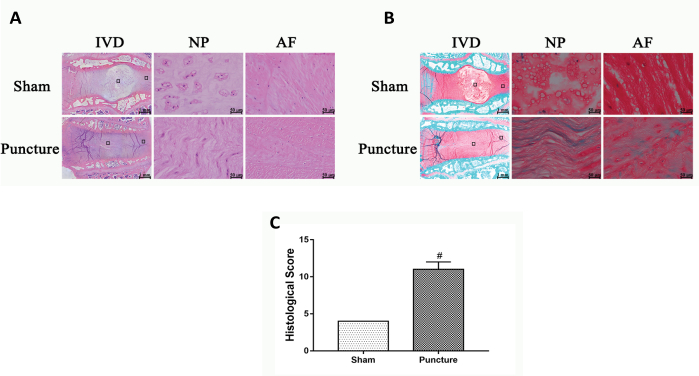
Figure 3: Histological staining in the sham group and needle puncture group. (A) H&E staining in both groups showed significant structural degeneration of the disc, including reduction of notochord cells, annulus folding, and breakdown of the boundary between the annulus and nucleus pulposus. (B) SO/FG staining showed that the deposition of proteoglycan and Type II collagen in the nucleus pulposus decreased in the needle puncture group. (C) Histological scores of the puncture group disc degeneration were significantly higher than those in the sham group. # p < 0.05 vs. the sham group. This figure has been modified with permission from Yang et al.22. Please click here to view a larger version of this figure.
Discussion
The critical steps in this protocol are the protection of the abdominal organs, the identification of the target discs, and the position and direction of the needle. The L5-6 IVD is just below the bifurcation of the iliac vein, and the L6-7 IVD is identified based on the position parallel to the iliac crest. These two markers enable precise positioning of the intervertebral disc and improve the accuracy and repeatability of surgery - which is one of the major advantages of the transabdominal approach. When the needle punctures the target discs, ensure that the position of the needle tip is in the center of IVD, and the direction of the needle tip is parallel to the upper and lower endplates to avoid damaging the endplates.
Because rabbit abdomens are soft, they are prone to deviation when determining the abdominal median incision. Interestingly, we found that the midpoint of the connection line between the two nipples and the middle incision can be performed accurately, which provides a more standardized anatomical approach and reduces unnecessary injury. In addition, the use of the peanut gauze for the separation of the prevertebral soft tissue allows faster and clearer exposure of the IVD structure with less bleeding.
The limitations of the transabdominal approach include an increased risk of intraperitoneal venous plexus rupture and mild intestinal and abdominal wall adhesion. The needle puncture group in this study had 4 rabbits, and one died. The cause of death was intraperitoneal venous plexus rupture, leading to excessive bleeding intraoperatively and postoperatively. According to our experience, if surgeons are not familiar with the surgical procedures and the anatomical structure of the rabbits, the operation time will increase, and more post-operative complications will occur. In addition, we did not use endotracheal intubation or ECG monitoring because these can greatly increase the duration of the operation and thus, cause more risks.
The retroperitoneal approach is a widely used approach but has many complications. For instance, when exposing the spine, avulsion of segmental arteries and spinal cord ischemia may occur, resulting in severe bleeding and post-operative bilateral hind leg paralysis. In addition, the needle may injure the endplate and nerve roots due to the limited visual field, which can exacerbate the degree of IVDD or accelerate the progression of IVDD, increasing the uncertainty of the experiment18,19. The transabdominal approach has some advantages over the retroperitoneal approach. To start with, the transabdominal approach can provide better visualization, and thus, surgeons can easily ensure correct needle orientation under direct vision. In addition, the bifurcation of the iliac vein and the position parallel to the iliac crest are two important anatomical marks that help precisely locate the target IVDs. In our previous study22, annulus fibrosis needle puncture can successfully induce IVDD models in rabbits via the transabdominal approach. The transabdominal approach is a better way to establish IVDD in rabbits.
Disclosures
The authors declare no competing interests or relationships that may lead to any conflicts.
Acknowledgements
This study was supported by the Natural Science Foundation of Hebei Province (No. H2021108006).
Materials
| Name | Company | Catalog Number | Comments |
| #22 scalpel blade | Huaiyin MEDICAL Instruments Co., Ltd. | AA6468 | None |
| 16-G needle, 26-G needle | Zhejiang Kangkang MEDICAL-DEVICES Co., Ltd. | 305111 | None |
| 3-0 absorbable suture | Huaiyin MEDICAL Instruments Co., Ltd. | V500431 | None |
| 4-0 non-absorbable braided suture | Huaiyin MEDICAL Instruments Co., Ltd. | R413 | None |
| 5 mL syringe, 1 mL syringe | Zhejiang Kangkang MEDICAL-DEVICES Co., Ltd. | 301942 | None |
| Double-ended handheld retractor | Huaiyin MEDICAL Instruments Co., Ltd. | 60002066 | None |
| Midazolam | Yichang Humanwell Pharmaceutical Co., Ltd. | M-908CAS | None |
| Needle holder | Huaiyin MEDICAL Instruments Co., Ltd. | HC00505336 | None |
| Peanut gauze | In-house | None | Hand-made ball-shaped gauze |
| Rabbit | Tonghui ulture Limited Liability Company | SCXK2016--002 | None |
| Scalpel handle | Huaiyin MEDICAL Instruments Co., Ltd. | AM5100678 | None |
| Stopper | In-house | None | Depth of 5 mm |
| Tissue scissors | Huaiyin MEDICAL Instruments Co., Ltd. | HC00505422 | None |
| Vaporizer | Apollo Management L.P. | BW-AM503 | None |
| Vessel clamp/forceps | Huaiyin MEDICAL Instruments Co., Ltd. | AM5102194 | None |
References
- Hartvigsen, J., et al. What low back pain is and why we need to pay attention. The Lancet. 391 (10137), 2356-2367 (2018).
- Simon, J., McAuliffe, M., Shamim, F., Vuong, N., Tahaei, A. Discogenic low back pain. Physical Medicine and Rehabilitation Clinics of North America. 25 (2), 305-317 (2014).
- Livshits, G., et al. Lumbar disc degeneration and genetic factors are the main risk factors for low back pain in women: The UK twin spine study. Annals of the Rheumatic Diseases. 70 (10), 1740-1745 (2011).
- Yang, S., Zhang, F., Ma, J., Ding, W. Intervertebral disc ageing and degeneration: The antiapoptotic effect of oestrogen. Ageing Research Reviews. 57, 100978 (2020).
- Daly, C., Ghosh, P., Jenkin, G., Oehme, D., Goldschlager, T. A review of animal models of intervertebral disc degeneration: Pathophysiology, regeneration, and translation to the clinic. BioMed Research International. 2016, 5952165 (2016).
- Li, Z., Gao, X., Ding, W., Li, R., Yang, S. Asymmetric distribution of Modic changes in patients with lumbar disc herniation. European Spine Journal. 32 (5), 1741-1750 (2023).
- Huo, Y., et al. Incidence and risk factors of lumbar plexus injury in patients undergoing oblique lumbar interbody fusion surgery. European Spine Journal. 32 (1), 336-344 (2023).
- Urban, J. P., Roberts, S. Degeneration of the intervertebral disc. Arthritis Research & Therapy. 5 (3), 120-130 (2003).
- Adams, M. A., Roughley, P. J. What is intervertebral disc degeneration, and what causes it. Spine (Phila Pa 1976). 31 (18), 2151-2161 (2006).
- Singh, K., Masuda, K., An, H. S. Animal models for human disc degeneration. The Spine Journal. 5 (6 Suppl), 267s-279s (2005).
- Mern, D. S., Walsen, T., Beierfuß, A., Thomé, C. Animal models of regenerative medicine for biological treatment approaches of degenerative disc diseases. Experimental Biology and Medicine (Maywood, N. J.). 246 (4), 483-512 (2021).
- Alini, M., et al. Are animal models useful for studying human disc disorders/degeneration. European Spine Journal. 17 (1), 2-19 (2008).
- Qian, J., et al. Selection of the optimal puncture needle for induction of a rat intervertebral disc degeneration model. Pain Physician. 22 (4), 353-360 (2019).
- Kroeber, M. W., et al. New in vivo animal model to create intervertebral disc degeneration and to investigate the effects of therapeutic strategies to stimulate disc regeneration. Spine (Phila Pa 1976). 27 (23), 2684-2690 (2002).
- Wang, Y., et al. Puncture intervertebral disc degeneration model: A standard on rabbit. Journal of Hard Tissue Biology. 29 (4), 223-230 (2020).
- Lotz, J. C. Animal models of intervertebral disc degeneration: lessons learned. Spine (Phila Pa 1976). 29 (23), 2742-2750 (2004).
- Lei, T., et al. A novel approach for the annulus needle puncture model of intervertebral disc degeneration in rabbits. American Journal of Translational Research. 9 (3), 900-909 (2017).
- Moss, I. L., et al. Retroperitoneal approach to the intervertebral disc for the annular puncture model of intervertebral disc degeneration in the rabbit. The Spine Journal. 13 (3), 229-234 (2013).
- Zhang, Y., et al. Allogeneic articular chondrocyte transplantation downregulates interleukin 8 gene expression in the degenerating rabbit intervertebral disk in vivo. American Journal of Physical Medicine & Rehabilitation. 94 (7), 530-538 (2015).
- Inglis, S., Strunk, A. Rabbit anesthesia. Lab Animal (NY). 38 (3), 84-85 (2009).
- Greenfield, E. A. Administering anesthesia to rabbits. Cold Spring Harbor Protocols. 2018 (9), (2018).
- Yang, K., et al. Comparisons between needle puncture and chondroitinase ABC to induce intervertebral disc degeneration in rabbits. European Spine Journal. 31 (10), 2788-2800 (2022).
- Hoogendoorn, R. J., Wuisman, P. I., Smit, T. H., Everts, V. E., Helder, M. N. Experimental intervertebral disc degeneration induced by chondroitinase ABC in the goat. Spine (Phila Pa 1976). 32 (17), 1816-1825 (2007).
- Pfirrmann, C. W., Metzdorf, A., Zanetti, M., Hodler, J., Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 26 (17), 1873-1878 (2001).
- Masuda, K., et al. A novel rabbit model of mild, reproducible disc degeneration by an anulus needle puncture: correlation between the degree of disc injury and radiological and histological appearances of disc degeneration. Spine. (Phila Pa 1976). 30 (1), 5-14 (2005).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved