Method Article
Microvascular Doppler Assisted Microsurgical Denervation of the Spermatic Cord in Treating Chronic Orchialgia
In This Article
Summary
Here, we present a protocol to treat chronic orchialgia by microsurgical denervation of the spermatic cord. Combined with the use of a microvascular doppler, the procedures can be more easily implemented.
Abstract
Chronic orchialgia is a common disease in department of urology and andrology. The etiology is complex, and the treatment is difficult. In severe cases, orchiectomy is even necessary. In recent years, microsurgical denervation of the spermatic cord (MDSC) is a minimally invasive and effective surgical method for the treatment of chronic orchialgia. Its greatest advantage is to preserve the testis and epididymis, avoid the possible organ resection. The key of the operation is to dissect all the fibrous tissues in the spermatic cord, while protecting the arteries (especially the testicular arteries) and several lymphatic vessels. Combined with the use of microvascular doppler in the operation, when separating the structure of spermatic cord under the microscope, the testicular arteries can be objectively and accurately protected (pulse “whistle” sound can be heard when the microvascular doppler probes the arterial surface), while artery injury and venous missed ligation can be avoided. The postoperative blood supply of the testis is also maximumly safeguarded. At the same time, we can be more fearless to cut the cremaster muscle, fatty and connective tissues surrounding the spermatic cord blood vessels and vas deferens after the arteries and lymphatic vessels being accurately protected under the microscope, finally achieve the spermatic cord completely "skeletonized" (only the testicular arteries, lymphatic vessels and vas deferens remained after the surgery). Thus we can better ensure the clinical curative effect (denervation thoroughly), avoid serious complications (testicular atrophy), and achieve better surgical results.
Introduction
Chronic orchialgia is a common disease accounting for about 2.5%–4.8% of all urology clinic visits1, which has been defined as more than 3 months of unilateral or bilateral scrotal pain interfering with daily life that ultimately leads to the pursuit of treatment2,3. The etiology is complex, and up to 50% of patients have no obvious etiology4. The exact mechanism is still unclear. Wallerian degeneration in peripheral nerves has been shown to be a potential cause of chronic pain5,6.
Microsurgical denervation of the spermatic cord (MDSC) is an effective treatment for patients with chronic orchialgia after the failure of conservative treatments, especially for patients with a positive response to spermatic cord block (defined as greater than or equal to 50% temporary reduction of pain based on VAS)7,8. The key to the operation is to dissect and ligate all the structures in the spermatic cord except the testicular arteries, a few lymphatic vessels, and the vas deferens9. Sometimes, it is difficult to divide small testicular arteries and the internal spermatic veins. It takes a bit more time to carefully dissect the arteries and preserve them.
We routinely combine the use of microvascular doppler during MDSC to avoid artery injury and venous missed ligation. A pulse “whistle” sound can be heard when the microvascular doppler probes the arterial surface while there is no sound in the veins. So, the difficulty of the surgery can be reduced, and the treatment outcomes can be improved.
Protocol
The protocol was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the ethics committee of the First Affiliated Hospital of Sun Yat-sen University. Chronic orchialgia patients who failed conservative treatment were admitted and signed informed consent.
1. Instruments for operation
- Ensure the availability of the surgical microscope and microvascular doppler.
2. Preparation for operation
- Clean and shave the inguinal/subinguinal skin and scrotum before surgery.
NOTE: Before surgery, the surgical site need not be sterilized. As a routine procedure, soap is used to clean the inguinal/subinguinal skin and scrotum, and then a razor is used for shaving the area. - Let the patient lie on the operating table in a supine position after combined spinal-epidural anesthesia.
NOTE: The anesthetist performs anesthetization. The anesthetization agents are mainly routine, while sometimes personalized. The choice and the dose of the anesthetic agent used are made by the anesthetist.
3. Procedure
- Expose and lift the spermatic cord out of the incision.
- Perform a 2 cm oblique skin incision below the external inguinal ring with a circular scalpel.
- Then, dissect the spermatic cord and deliver it through the incision with the help of appendix forceps (see Figure 1).
- Microsurgical varicocelectomy
- Bring an operating microscope into the operating field, and examine the cord under 8–12x power magnification.
- Use an electric knife to cut the external fascia and cremasteric fibers about 1 cm. Bluntly separate the internal spermatic fascia with its structures from the vas deferens and its vessels by a loop. Ligate the external spermatic vessels with 4-0 silk sutures.
- Drip 1% lidocaine solution on the spermatic cord. Use an intra-operative vascular Doppler flow detector (see Figure 2) to localize the internal spermatic arteries (pulse “whistle” sound can be heard when the microvascular doppler probes the arterial surface while there is no sound on the veins).
- Doubly ligate all of the internal spermatic veins with 4-0 silk ties and divide them. Accurately separate and preserve all identified arteries and lymphatics by loops (see Figure 3). Use microvascular doppler to distinguish arteries from veins when necessary.
- Microsurgical denervation (see Figure 4)
- Next, carefully divide the anterior cremasteric muscle. Cut off the fatty and connective tissues surrounding the spermatic cord blood vessels and vas deferens completely with an electric knife. Identify and preserve the vas deferens and its associated vessels.
- Ligate and divide the vasal veins attached to the vas deferens when the vessels enlarge. Divide the posterior cremasteric fibers and fat components.
- Finish the operation
- Skeletonize (only the testicular arteries, lymphatic vessels, and vas deferens remained after the surgery) the spermatic cord completely. Use the microvascular doppler to examine the testicular arteries again (see Figure 5).
- Then, manually place the cord back into the incision. Suture the deep tissue and skin.
Results
In total, 26 chronic orchialgia patients were admitted to the East Division of the First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China, between March 2011 and June 2021 (Table 1). The average age of the patients was 39.9 ± 13.4 years. Within this group, 23 men underwent unilateral MDSC, and three men underwent bilateral MDSC successively. Prior to MDSC, all patients underwent spermatic cord block and had a positive response. The mixture we utilized comprises 5 mL of 2% lidocaine and 40 mg of methylprednisolone. The mean operation time was 121.2 ± 36.5 min. Less bleeding was observed during the operation. No complications (testicular atrophy, hydrocele, hematomas, or wound infection) occurred after the operation. The follow-up time was 6–81 months, and the median follow-up time was 43.5 months. VAS score was used to evaluate the pain. Significant reduction of pain was defined as greater than or equal to 50% temporary pain reduction based on VAS. Complete pain-free was defined as no pain remaining and zero VAS score. Among 26 patients, 21 (80.8%) had a significant reduction in pain. 10 (38.5%) of them were even completely pain-free.
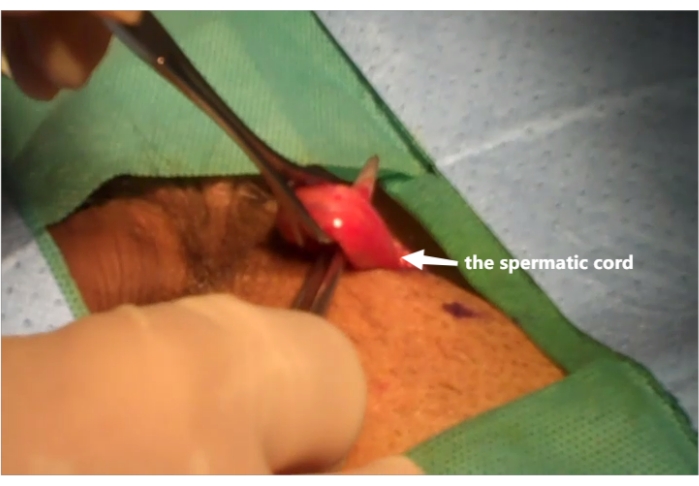
Figure 1: Elevate the spermatic cord. The spermatic cord is lifted out of the incision with the help of appendix forceps. Please click here to view a larger version of this figure.

Figure 2: Localize the internal spermatic arteries by microvascular doppler. Microvascular Doppler is used under a microscope. Please click here to view a larger version of this figure.

Figure 3: Ligate internal spermatic veins while preserving the testicular arteries and lymphatic vessels. Internal spermatic veins are doubly ligated and divided. Testicular arteries and lymphatic vessels are separated by loops. Please click here to view a larger version of this figure.
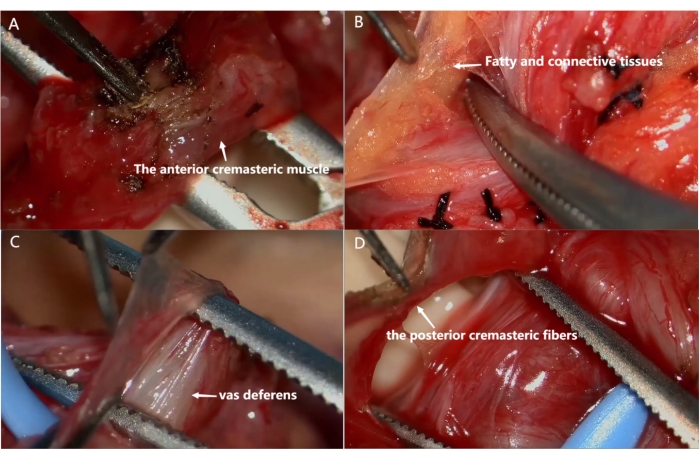
Figure 4: Microsurgical denervation of the spermatic cord. (A) Divide the anterior cremasteric muscle. (B) Divide fatty and connective tissues surrounding the spermatic cord blood vessels. (C) Separate the vas deferens and divide the connective tissues around the vas deferens. (D) Divide the posterior cremasteric fibers and fat component. Please click here to view a larger version of this figure.
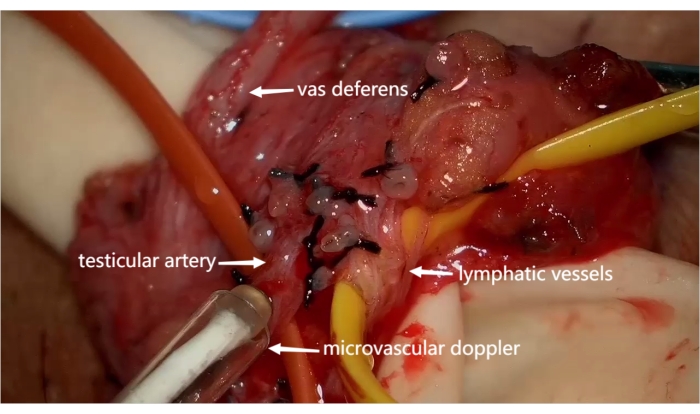
Figure 5: The spermatic cord "skeletonized" (only the testicular arteries, lymphatic vessels, and vas deferens remained). Microvascular doppler is used to examine the testicular arteries again. Please click here to view a larger version of this figure.
| Clinical data | Median | Least value | Maximjm value | |
| Enrolled No. | 26 | / | / | / |
| Significant pain relief No. (rate) | 21 (80.8%) | / | / | / |
| Completely pain free No. (rate) | 10 (38.5%) | / | / | / |
| Surgical complications No. | 0 | / | / | / |
| Age (years) | 39.9 ± 13.4 | 37.5 | 22 | 66 |
| Operation time (min) | 121.2 ± 36.5 | 117.5 | 70 | 225 |
| Follow-up time (months) | 43.6 ± 22.9 | 43.5 | 6 | 81 |
Table 1: The clinical data of chronic orchialgia patients enrolled.
Discussion
Microsurgical denervation of the spermatic cord (MDSC) is a minimally invasive surgical option for treating chronic orchialgia after the failure of conservative treatments7,8. Significant reduction or elimination of pain is reported in various studies; the pain relief rate is about 80%4,10,11. Prior to MDSC, it is recommended that the patient undergo a spermatic cord block to assess the likelihood of success of the surgery. Benson et al. has shown that a positive response to the cord block is a significant independent predictor of success for MDSC12. In bilateral chronic orchialgia patients, the more serious side is addressed first to assess MDSC. If a good response is noted, the other side is then treated by MDSC 3–6 months later10,13. In severe cases, if the pain is unchanged several months after the operation, it is only then that more drastic measures, such as orchiectomy, are considered14.
Parekattil et al. found that Wallerian degeneration (WD) occurred in 84% of chronic orchialgia patients. The densest sites of WD were distributed in the corticotropis muscle, around the vas deferens, and the internal spermatic artery in the spermatic cord15. Transection of these nerves in the cord may explain the beneficial effect of the MDSC procedure. The standard MDSC involves ligation of all the structures in the spermatic cord except the arteries and lymphatic vessels. It is quite a risky procedure that may lead to testicular atrophy, testicular loss, hydrocele, or lymphocele in some cases15. The key to the operation is to dissect the cord and preserve the arteries (especially the testicular arteries) and several lymphatic vessels.
In this study, all patients had a positive response to spermatic cord block, which showed temporary pain relief. A small subinguinal incision was made. After the spermatic cord was elevated through the incision, every procedure should be performed with the aid of a surgical microscope. Microvascular doppler was routinely used during MDSC; a pulse “whistle” sound was heard when it probed the arterial surface, while no sound was heard on the veins. First, we used it to localize the testicular arteries before we incised the internal fascia of the spermatic cord. Second, during the internal spermatic veins ligated, we used it to distinguish arteries from veins when necessary. Finally, we used it to examine the testicular arteries again at the end of the operation. Therefore, the testicular arteries were objectively and accurately protected, while artery injury and venous missed ligation were avoided. The postoperative blood supply of the testis was also maximumly safeguarded. Meanwhile, we were more fearless to cut the cremaster muscle, fatty and connective tissues surrounding the spermatic cord blood vessels, and vas deferens. The spermatic cord was completely "skeletonized" (only the testicular arteries, lymphatic vessels, and vas deferens remained after the surgery)9. Thus, we can better ensure the clinical curative effect (denervation thoroughly). The significant pain relief rate reached 80.8%, and the completely pain-free rate reached 38.5%. Mild bleeding was observed, and no complications occurred in this study.
In summary, treatment of chronic orchialgia by MDSC combined with the use of microvascular doppler is safe, minimally invasive, and effective. Since the use of microvascular doppler, artery injury and venous missed ligation can be avoided, the surgical procedures are more easily implemented. It is advantageous in spreading and application.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This study was supported by the Clinical Research Training Program, the East Division of the First Affiliated Hospital of Sun Yat-sen University (No.2019002, No.2019008).
Materials
| Name | Company | Catalog Number | Comments |
| Surgical microscope | Leica | Model M520 MC-1 | Leica operating microscope |
| Micro needle forceps | Cheng-He,NingBo | HC-A006 | microsurgery instrument |
| Micro scissors | Cheng-He,NingBo | HC-A008 | microsurgery instrument |
| Microscopic tweezers | Cheng-He,NingBo | HC-A002 | microsurgery instrument |
| Microvascular doppler | VTI | VTI 20 MHz | intra-operative vascular Doppler flow detector |
References
- Sigalos, J. T., Pastuszak, A. W. Chronic orchialgia: epidemiology, diagnosis and evaluation. Translational Andrology and Urology. 6, 37-43 (2017).
- Davis, B. E., Noble, M. J., Weigel, J. W., Foret, J. D., Mebust, W. K. Analysis and management of chronic testicular pain. Journal of Urology. 143 (5), 936-939 (1990).
- Polackwich, A. S., et al. Development of a clinically relevant symptom index to assess patients with chronic orchialgia/chronic scrotal content pain. Translational Andrology and Urology. 7, 163-168 (2018).
- Larsen, S. M., Benson, J. S., Levine, L. A. Microdenervation of the spermatic cord for chronic scrotal content pain: Single institution review analyzing success rate after prior attempts at surgical correction. Journal of Urology. 189 (2), 554-558 (2013).
- Parekattil, S. J., et al. Trifecta nerve complex: potential anatomic basis for microsurgical denervation of the spermatic cord for chronic orchialgia. Journal of Urology. 190 (1), 265-270 (2013).
- Ko, M. H., Hsieh, Y. L., Hsieh, S. T., Tseng, T. J. Nerve demyelination increases metabotropic glutamate receptor subtype 5 expression in peripheral painful mononeuropathy. International Journal of Molecular Sciences. 16 (3), 4642-4665 (2015).
- Levine, L. Chronic orchialgia: evaluation and discussion of treatment options. Therapeutic Advances in Urology. 2 (5-6), 209-214 (2010).
- Parekattil, S. J., Gudeloglu, A. Robotic assisted andrological surgery. Asian Journal of Andrology. 15 (1), 67-74 (2013).
- Tu, X. A., et al. Microsurgical denervation of the spermatic cord for treatment of idiopathic chronic orchialgia. Chinese Medical Journal (English). 125 (15), 2784-2786 (2012).
- Calixte, N., et al. Targeted robotic assisted microsurgical denervation of the spermatic cord for the treatment of chronic orchialgia or groin pain: A single center, large series review. Journal of Urology. 199 (4), 1015-1022 (2018).
- Parekattil, S. J. Targeted microsurgical denervation of the spermatic cord for chronic orchialgia: the current standard of care. Current Urology Reports. 21 (11), 47 (2020).
- Benson, J. S., Abern, M. R., Larsen, S., Levine, L. A. Does a positive response to spermatic cord block predict response to microdenervation of the spermatic cord for chronic scrotal content pain. Journal of Sexual Medicine. 10 (3), 876-882 (2013).
- Oh, P. J., Bajic, P., Lundy, S. D., Ziegelmann, M., Levine, L. A. Chronic scrotal content pain: a review of the literature and management schemes. Current Urology Reports. 22 (2), 12 (2021).
- Rönkä, K., Vironen, J., Kokki, H., Liukkonen, T., Paajanen, H. Role of orchiectomy in severe testicular pain after inguinal hernia surgery: audit of the Finnish Patient Insurance Centre. Hernia. 19 (1), 53-59 (2015).
- Parekattil, S. J., Ergun, O., Gudeloglu, A. Management of chronic orchialgia: Challenges and solutions - The current standard of care. Research and Reports in Urology. 12, 199-210 (2020).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved