Method Article
A Retrospective Study on Endoscopic Surgery for the Treatment of Paravertebral Abscess in Spinal Tuberculosis Patients
In This Article
Summary
This study evaluated endoscopic debridement for treating paravertebral abscesses in patients with spinal tuberculosis. Compared to conventional surgery, it significantly improved surgery time, blood loss, hospital stay, pain relief, and neurological outcomes, with fewer complications and no recurrences. These findings highlight its efficacy and safety. Further long-term studies are recommended.
Abstract
Spinal tuberculosis (TB) remains a significant global health concern, necessitating the development of innovative treatment strategies. This clinical study aimed to evaluate the efficacy and safety of endoscopic debridement as a minimally invasive approach for treating paravertebral abscesses in patients with spinal tuberculosis. A total of 52 patients diagnosed with paravertebral tuberculosis abscesses were enrolled in this retrospective study. Patients were assigned to two groups: the endoscopic debridement group (n = 30) and the conventional open surgery group (n = 22), based on the type of surgery they received. Clinical outcomes were assessed at baseline, post-treatment, and follow-up visits at regular intervals, including surgery time, intraoperative blood loss, total hospital stay duration, pain relief, and neurological improvement. The results of this study demonstrate that endoscopic debridement is a highly effective treatment for paravertebral abscesses in patients with spinal TB. Patients in the endoscopic debridement group experienced significant improvements in surgery time, intraoperative blood loss, total hospital stay duration, pain relief, and neurological improvement compared to those in the conventional open surgery group. Additionally, the endoscopic approach resulted in fewer complications, such as wound infections and postoperative instability, with no cases of recurrence observed during the follow-up period. Therefore, this clinical study highlights the potential of endoscopic debridement as a safe and effective treatment modality for spinal tuberculosis. The technique not only effectively eliminates infected tissue but also ensures faster patient recovery and reduces postoperative complications. Additional research and long-term follow-up studies are necessary to confirm the long-term effectiveness and safety of endoscopic debridement as the standard treatment for spinal tuberculosis.
Introduction
The risk of tuberculosis is increasing in the last decade due to the rise in drug-resistant tuberculosis bacterial strains and the prevalence of patients living with HIV. An estimated 10 million new cases of tuberculosis and 1.6 million deaths due to tuberculosis were reported globally in 2021 alone, an increase from 1.5 million in 20201. Tuberculosis of the bone and joints accounts for about 1%-2% of all patients with tuberculosis, and spinal tuberculosis accounts for 50% of all skeletal tuberculosis cases2. Spinal tuberculosis often causes pain and symptoms of systemic tuberculosis poisoning. In severe cases, it can lead to kyphotic deformity due to vertebral erosion, spinal cord injury, and paralysis. Active diagnosis and treatment can help relieve symptoms and create favorable conditions for neural recovery3,4.
The literature on treatments for thoracic and lumbar tuberculosis outlines several protocols, including a regimen of anti-TB drugs such as isoniazid, pyrazinamide, rifampicin, and ethambutol, various surgical approaches like anterior radical debridement with graft fusion or posterior debridement with fusion and fixation, as well as minimally invasive methods. Anti-TB chemotherapy is established as the principal treatment for spinal tuberculosis (ST). Surgery is recommended for cases demonstrating clear vertebral instability, non-response to chemotherapy, increasing spinal deformity, severe neurological deficits, or large paravertebral abscesses (PA) with or without compression of the epidural space. Reports indicate that 10% to 43% of spinal tuberculosis cases are complicated by severe kyphosis and neural functional damage, necessitating surgical treatment primarily to remove the lesion and relieve nerve compression5,6. The goal has always been to choose a safe, effective, and less invasive method for the treatment of spinal tuberculosis7,8. Minimally invasive spine surgeries (MIS) are frequently employed to treat degenerative spinal disorders. Among these, full endoscopic surgeries-an established subset of MIS-are effectively utilized for managing disc herniations and spinal stenosis. Nonetheless, their effectiveness in the debridement of vertebral tuberculosis lesions remains underexplored9,10.
Since January 2016, Urumqi Friendship Hospital has implemented minimally invasive anterior debridement to treat lumbar tuberculosis with paravertebral abscess. To provide a reference for future clinical practice, we compared the results of this unique method with traditional posterior fixation combined with anterior debridement techniques.
Protocol
All procedures involved in the current study were approved by the ethical committee of Urumqi Friendship Hospital, and all patients agreed to the publication of their clinical material, provided their identity is not revealed. From January 2018 to January 2023, clinical and radiological materials, as well as blood work of patients treated with anterior debridement for lumbar tuberculosis with paravertebral abscess, were retrospectively analyzed. The diagnosis of spinal tuberculosis was confirmed by T-SPOT tests, spinal MRI and CT tests, and tissue acid-fast bacilli culture tests4,7,8. The commercial details of the equipment involved in this study are listed in the Table of Materials.
1. Preoperative preparation
- Conduct routine laboratory examinations, including ESR, CPR, and TB antibody tests for all patients upon admission.
- Perform X-ray, CT, and MRI examinations for surgical planning.
NOTE: Figure 1A,B depicts a representative sagittal and horizontal MRI view confirming the presence of tuberculosis. - Record basic information, including VAS back pain scores11, Oswestry Disability Index (ODI)12, and spinal cord ASIA scores13.
- Administer four antituberculosis drugs (isoniazid, rifampicin, ethambutol, streptomycin/pyrazinamide) for 4 weeks prior to the operation.
- Monitor the liver function closely during treatment.
- Schedule surgery when the patients' general condition is suitable for intervention and when the erythrocyte sedimentation rate (ESR) is lower than 40 mm/h.
2. Surgical procedure of endoscopic debridement
- Anesthesia and positioning
- Administer general anesthesia (following institutionally approved protocols) and perform tracheal intubation14.
- Place the patient in the prone position on the operating table.
- Surgical site preparation
- Thoroughly disinfect the surgical area to maintain aseptic conditions.
- Cover the patient with a sterile towel to ensure a sterile field around the surgical site.
- Incision planning
- Use C-arm X-ray fluoroscopy to accurately determine the exact point for the surgical incision.
- After identifying the precise location, make a small incision at the determined point, ensuring minimal tissue disruption.
- Assessment and debridement planning
- Assess the severity of the infection and the extent of tissue damage through visual and imaging inspection.
- Based on this assessment, plan the range of debridement necessary to effectively treat the infection.
- Endoscopic debridement procedure
- Use the C-arm X-ray machine to determine the surface projection of the lesion space. Select the right-sided foraminal level of the lesion as the needle puncture site.
- Angle the puncture needle at 20-35 degrees relative to the torso of the affected spine to facilitate soft tissue pathway expansion along the needle toward the spinal canal.
- After confirming the position fluoroscopically, make a 5 mm incision with a pointed scalpel and establish a subcutaneous tunnel through the incision.
- Begin the procedure by thoroughly eradicating the paravertebral abscess to eliminate the primary source of infection.
- Perform surgical treatment for lumbar spinal tuberculosis, which includes spinal canal decompression, neurolysis, disc radiofrequency ablation, and intervertebral space catheter insertion3,5,10.
- Under continuous irrigation with sterile saline, use nucleotomy forceps and biopsy forceps through the foraminal endoscope to remove purulent secretions and caseous necrotic tissue, and to excise sequestrum, thoroughly cleaning the lesion.
- Collect tissue samples from the lesion for bacteriological culture, drug sensitivity testing, and pathological examination. Achieve complete relief of the front edge of the nerve and dura mater sac.
- After resecting the lesion, implant an appropriate autologous bone graft, typically harvested from the posterior iliac crest, between the vertebrae, verifying the efficacy of the graft fixation by X-ray.
- Administer localized antibiotic treatment by placing 2 g of streptomycin and 0.3 g of isoniazid directly into the affected area to enhance infection control and support healing.
- Insert a drainage tube into the surgical site to allow for postoperative drainage of fluids, reducing the risk of fluid accumulation and subsequent infection.
- Close the incision carefully, ensuring that all layers are securely sutured using size 1 sutures to support optimal healing and minimize the risk of postoperative complications.
NOTE: Figure 1C shows an extracted diseased tissue following endoscopic surgery.
- Use the C-arm X-ray machine to determine the surface projection of the lesion space. Select the right-sided foraminal level of the lesion as the needle puncture site.
3. Postoperative care following endoscopic debridement
- Monitor postoperative drainage closely, and remove the drainage tube once the output is less than 5 mL per day, typically within 2-4 weeks.
- Continue the patient on a regimen of standard antituberculosis therapy, consisting of a combination of Isoniazid (0.3 g, once daily), Rifampin (0.45 g, once daily), Pyrazinamide (0.5 g, three times daily), and Ethambutol (0.75 g, once daily) for the first 2 months. Follow this with a combination of Isoniazid (0.3 g, once daily) and Rifampin (0.45 g, once daily) for the next 4 months.
- Review the patient regularly with follow-up imaging and blood tests to monitor healing and promptly detect any signs of complication.
4. Traditional posterior debridement
- Administer general anesthesia (following institutionally approved protocols) and position the patient prone on the operating table.
- Disinfect the surgical area thoroughly and cover it with a sterile towel to maintain a sterile field. Utilize C-arm X-ray fluoroscopy to determine and mark the incision site. Make a longitudinal incision of 10-15 cm along the central line of the spine.
- Carefully expose the affected vertebrae along with 1-2 adjacent normal vertebrae above and below the targeted area. Thoroughly wash the abscess with normal saline to clear any purulent material and debris.
- Administer localized antibiotic treatment by placing 2 g of streptomycin and 0.3 g of isoniazid directly into the focus area to ensure eradication of bacterial infection.
- Insert a drainage tube into the surgical site for postoperative drainage. Close the incision using size 1 sutures in layers, ensuring secure wound closure to facilitate healing and minimize the risk of infection.
- Post-operatively, monitor the drainage output and remove the drainage tube when the volume is reduced to less than 50 mL per day. Continue standard postoperative protocols, including antituberculosis therapy and regular follow-up imaging and blood tests, to ensure proper healing and monitor for any signs of complications.
5. Postoperative care following traditional posterior debridement
- Remove the drainage tube when the daily drainage volume is less than 20 mL, typically 5-7 days after surgery.
- Continue the patient on a regimen of standard antituberculosis therapy, consisting of a combination of Isoniazid (0.3 g, once daily), Rifampin (0.45 g, once daily), Pyrazinamide (0.5 g, three times daily), and Ethambutol (0.75 g, once daily) for the first 2 months. Follow this with a combination of Isoniazid (0.3 g, once daily) and Rifampin (0.45 g, once daily) for the next 4 months.
- Obtain X-ray films 3 months, 6 months, and 1 year after the operation.
- Check blood ESR and liver and kidney functions on time during follow-up.
6. Outcome assessment
- Record the operative time, intraoperative hemorrhage, and postoperative drainage volume of both groups during and immediately after the surgery.
- Observe the VAS score11, ASIA grade13, ODI12, operation time, intraoperative hemorrhage, hospital stay duration, postoperative complications, and bone graft fusion ratio before the surgery and during follow-up.
7. Statistical analysis
- Use a statistical analysis software to analyze the data.
- Express the measurement data as mean ± standard deviation.
- Apply independent sample t-tests for comparison of measurement data and Chi-square tests for nominal data. Consider P < 0.05 as the norm for statistical significance.
Results
Fifty-two patients, including 28 males and 24 females, aged 18 to 73 years (50.2 ± 10.5) were included in the current study. Thirty patients were treated with minimally invasive anterior debridement and fusion (minimally invasive surgery group), while 22 patients underwent traditional open surgery (conventional surgery group). In the minimally invasive surgery group, there were 17 males and 13 females, aged 24-72 years (51.4 ± 9.1), including 18 single vertebral bodies and 12 double vertebral bodies. In the conventional surgery group, there were 13 males and 9 females, aged 18-65 years (48.6 ± 9.6), with 14 single vertebral bodies and 8 double vertebral bodies. There was no significant difference observed between the two groups in age, symptom duration, preoperative complications, and the number of involved vertebral segments (P > 0.05, Table 1). There was no significant difference observed between the two groups in age, symptom duration, preoperative complications, and the number of involved vertebral segments (P > 0.05).
Patients were followed up for 12-30 months (15.3 ± 3.2). With the gradual control of infection and pain, the erythrocyte sedimentation rate (ESR) of most cases decreased within one month after the operation. Although the ESR remained high in four patients with wound infections, it approached normal levels during the reexamination three months after surgery.
The total operative time was 74.3 ± 18.6 min in the minimally invasive group and 155.8 ± 29.4 min in the conventional surgery group. The difference between the two groups was statistically significant (P < 0.01). The volume of intraoperative hemorrhage was 81.0 mL ± 27.8 mL in the minimally invasive surgery group and 242.3 mL ± 45.3 mL in the conventional surgery group, with a statistically significant difference (P < 0.01). The Visual Analog Scale (VAS) score and Oswestry Disability Index (ODI) of the two groups improved significantly at three months and at the last follow-up compared to preoperative levels (P < 0.01, Table 2). Both the VAS score11 and ODI12 were better in the early postoperative period and at the last follow-up in the minimally invasive surgery group compared to the conventional surgery group (P < 0.05, Table 2). The operative time was longer in the conventional surgery group compared to the minimally invasive group; the volume of intraoperative hemorrhage was significantly lower in the minimally invasive group than in the conventional surgery group. The VAS score and ODI of the two groups improved significantly at three months and at the last follow-up compared to preoperative levels; both the VAS score and ODI were better in the early postoperative period and at the last follow-up in the minimally invasive surgery group compared to the conventional surgery group.
According to the ASIA classification13, there were six patients with spinal cord dysfunction before surgery. In the minimally invasive surgery group, there were two patients with grade D, while in the conventional surgery group, there were three patients with grade D and one patient with grade C. Except for one patient with grade D in the conventional surgery group, all other patients recovered to grade E.
The imaging data from the last follow-up showed that all patients achieved complete bone fusion. One patient in the conventional surgery group had a wound infection and was discharged after 2 weeks of dressing changes and antibacterial treatment. Postoperative lung infections were found in one patient in the conventional surgery group and in one patient in the minimally invasive surgery group. Additionally, there was one patient with gastrointestinal discomfort after surgery in the conventional surgery group. All complications were resolved with non-surgical intervention.
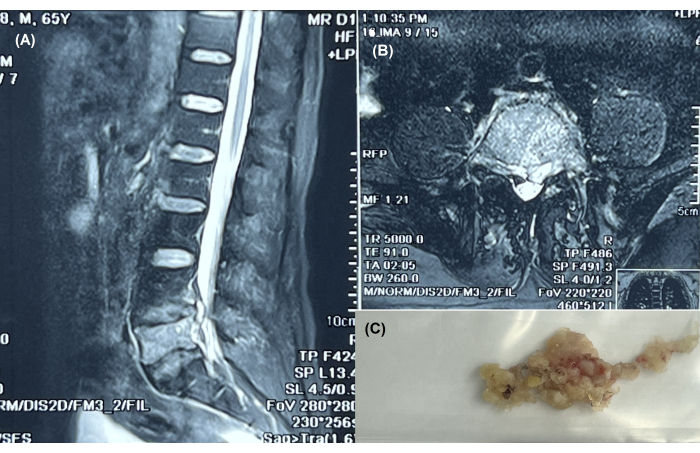
Figure 1: Endoscopic treatment of tuberculosis at L4-S1. (A) Sagittal MRI view of the spine showing tuberculosis at the L4-S1 level in a 65-year-old patient with paravertebral abscess. (B) Horizontal MRI view confirming the presence of tuberculosis at the same level. (C) Extracted diseased tissue following endoscopic surgery. Please click here to view a larger version of this figure.
| Minimally invasive | Conventional | t/X2 value | P value | ||
| Male/female | 17/13 | 13-09-2024 | 0.03 | 0.81 | |
| Age | 51.4 ± 9.1 | 48.6 ± 9.6 | 1.1 | 0.3 | |
| Symptom duration (months) | 5.5 ± 2.0 | 4.8 ± 1.3 | 1.58 | 0.12 | |
| Complications | Cardiovascular | 8 | 6 | 0.07 | 0.8 |
| Diabetes | 7 | 5 | 0.02 | 0.89 | |
| Osteoporosis | 9 | 7 | 0.26 | 0.61 | |
| Involved vertebrae | Single | 18 | 14 | 0.71 | 0.79 |
| Double | 12 | 8 | |||
Table 1: Comparison of patient demographics and preoperative characteristics. There was no significant difference between the two groups in terms of age, symptom duration, preoperative complications, and the number of involved vertebral segments (P > 0.05).
| Minimally invasive | Conventional | t value | P value | ||
| Operation time, min | 74.3 ± 18.6 | 155.8 ± 29.4 | 6 | <0.01 | |
| Intraoperative hemorrhage (mL) | 81.0 ± 27.8 | 242.3 ± 45.3 | 15.8 | <0.01 | |
| Time for hospital stay (days) | 10.8 ± 2.8 | 15.2 ± 4.4 | 4.4 | <0.01 | |
| VAS score | Before surgery | 5.6 ± 1.0 | 6.1 ± 1.0 | 2 | 0.08 |
| 3 months after surgery | 2.0 ± 0.9 | 3.5 ± 0.8 | 6.4 | <0.01 | |
| At last follow up | 1.1 ± 0.7 | 2.4 ± 0.5 | 7.1 | <0.01 | |
| ODI | Before surgery | 50.2 ± 8.4 | 53.1 ± 8.7 | 1.2 | 0.24 |
| 3 months after surgery | 22.9 ± 8.1 | 30.3 ± 6.5 | 3.5 | <0.01 | |
| At last follow up | 3.3 ± 1.4 | 6.5 ± 2.1 | 6.4 | 0.01 | |
| ESR | Before surgery | 38.1 ± 16.7 | 42.2 ± 15.9 | 0.91 | 0.37 |
| At last follow up | 24.5 ± 9.3 | 21.2 ± 8.3 | 1.32 | 0.19 | |
| CRP | Before surgery | 66.0 ± 25.7 | 67.2 ± 19.8 | 0.18 | 0.86 |
| At last follow up | 26.8 ± 7.6 | 28.1 ± 9.3 | 0.53 | 0.6 | |
Table 2: Surgical outcomes of minimally invasive vs. conventional surgery. Surgery duration was longer in the minimally invasive group compared to the conventional surgery group. The volume of intraoperative hemorrhage was significantly lower in the minimally invasive group than in the conventional surgery group. The VAS score and ODI for both groups improved significantly at 3 months and at the last follow-up compared to preoperative values. Both VAS score and ODI were better in the early postoperative period in the minimally invasive surgery group than in the conventional surgery group, as well as at the last follow-up.
Discussion
The spine is one of the most common locations for tuberculosis, besides the lungs. If not treated in a timely manner, nerve function can be compromised, potentially leading to paralysis and other complications. The combination of anti-tuberculous drugs and surgical intervention is widely accepted as the approach to treat severe spinal tuberculosis. Surgical treatment is the most direct and effective method for these patients. The purpose of surgical treatment for spinal tuberculosis is to clear the abscess, restore stability to the spine, and relieve compression of the spinal cord and nerve roots15,16,17. Traditional open surgery involves significant trauma to the patient, substantial blood loss during the procedure, and an increased risk of postoperative infection, along with a prolonged hospital stay and lower overall treatment effectiveness. This surgical approach also has certain limitations and may not be suitable for patients with poor tolerance or compromised physical conditions18,19,20.
With the development of imaging technology and endoscopic techniques, minimally invasive spinal surgery has gradually replaced open surgeries. This technique features smaller incisions, higher safety, and lower levels of pain, making it suitable for various patients21,22. In cases of thoracic or lumbar tuberculosis with a paravertebral abscess but without severe neurological damage or significant kyphotic distortion, minimally invasive abscess debridement and drainage, along with chemotherapy, may provide a better treatment strategy. In the current study, we examined the efficacy of combining percutaneous catheter drainage with chemotherapy. The results indicated that the early Visual Analog Scale (VAS) score11 and Oswestry Disability Index (ODI)12 in the minimally invasive surgery group were better than those in the conventional surgery group. This improvement could be attributed to several factors: minimally invasive anterior abscess removal can avoid extensive tissue damage, protect the posterior column, and prevent injury to the spinal cord and nerve roots.
The results of this study are consistent with previous reports. In the study by Zhang et al.23, 106 patients with paraspinal abscesses due to spinal tuberculosis were treated using computed tomography-guided percutaneous catheter drainage and percutaneous catheter infusion chemotherapy. They found a significantly reduced erythrocyte sedimentation rate three months after surgery and solid bone fusion during an average follow-up of 7.21 years. In the study by Liu et al.24, 17 patients with upper cervical spine tuberculosis were treated using endoscopic anterior cervical debridement combined with posterior fixation and fusion. Significant postoperative neurological improvement was achieved in all patients, with most achieving excellent or good results as measured using the Kirkaldy-Willis criteria. However, few studies have compared the effectiveness and safety of minimally invasive endoscopic surgeries with traditional open-surgical approaches.
While providing direct evidence on the application of minimally invasive surgical treatment for paraspinal abscesses in patients with spinal tuberculosis, this study has several limitations. This is a retrospective study involving a relatively small number of patients, and the follow-up time is short compared to the studies by Zhang and Liu19,20. Multi-center studies with larger sample sizes are necessary for a more objective evaluation of this surgical technique.
In summary, it is essential to choose an appropriate operative measure to treat paravertebral abscesses in patients with spinal tuberculosis to achieve early and complete functional recovery without recurrence of infection. Anterior minimally invasive debridement and bone graft fusion in the treatment of lumbar tuberculosis with severe paraspinal abscesses have significant advantages over conventional methods in terms of early postoperative functional recovery and pain improvement. It is a safe and effective technique for the treatment of lumbar tuberculosis.
Disclosures
The authors declare no competing financial interests or other conflicts of interest.
Acknowledgements
None.
Materials
| Name | Company | Catalog Number | Comments |
| C-arm fluoroscope | GE Healthcare | https://www.gehealthcare.com/products/surgical-imaging/c-arms-for-orthopedics | |
| Endoscope | JIOMAX (Germany) | https://www.joimax.com/en/products/ | used for the surgeical procedure |
| SPSS | IBM, Chicago, IL | version 24.0 | software for statistocal analysis |
References
- Bagcchi, S. WHO's global tuberculosis report 2022. The Lancet Microbe. 4 (1), e20 (2023).
- Leowattana, W., Leowattana, P., Leowattana, T. Tuberculosis of the spine. World J Orthop. 14 (5), 275-293 (2023).
- Kilinc, F., Setzer, M., Behmanesh, B. Surgical management and clinical outcome of cervical, thoracic and thoracolumbar spinal tuberculosis in a middle-European adult population. Sci Rep. 13 (1), 7000 (2023).
- Na, S., Lyu, Z. S., Zhang, S. Diagnosis and treatment of skipped multifocal spinal tuberculosis lesions. Orthopaed Surg. 15 (6), 1454-1467 (2023).
- Arifin, J., Biakto, K. T., Johan, M. P. Clinical outcomes and surgical strategy for spine tuberculosis: A systematic review and meta-analysis. Spine Deform. 12 (2), 271-291 (2024).
- Deng, F., Chen, B., Guo, H. Effectiveness and safety analysis of titanium mesh grafting versus bone grafting in the treatment of spinal tuberculosis: a systematic review and meta-analysis. BMC Surg. 23 (1), 377 (2023).
- Li, Z., Wang, J., Xiu, X. Evaluation of different diagnostic methods for spinal tuberculosis infection. BMC Infect Dis. 23 (1), 695 (2023).
- Talebzadeh, A. T., Talebzadeh, N. Diagnosis, management, and prognosis of spinal tuberculosis: A case report. Cureus. 15 (2), e35262 (2023).
- Ruparel, S., Tanaka, M., Mehta, R. Surgical management of spinal tuberculosis-the past, present, and future. Diagnostics. 12 (6), 1307 (2022).
- Lokhande, P. V. Role of full endoscopic procedures in management of tuberculosis of spine[m]//tuberculosis of the spine. Springer Nat. 2022, 309-324 (2022).
- Ogon, M., Krismer, M., Söllner, W. Chronic low back pain measurement with visual analogue scales in different settings. Pain. 64 (3), 425-428 (1996).
- Fairbank, J., Pynsent, P. The oswestry disability index. Spine. 25 (22), 2940-2953 (2000).
- Curt, A., Keck, M., Dietz, V. Functional outcome following spinal cord injury: Significance of motor-evoked potentials and ASIA scores. Arch Phys Med Rehabil. 79 (1), 81-86 (1998).
- Barash, P. G. . Clinical anesthesia. , (2009).
- Boussaid, S., M'rabet, M., Rekik, S. Spinal tuberculosis: Features and early predictive factors of poor outcomes. Mediterr J Rheumatol. 34 (2), 220 (2023).
- Mandar, B., Menon, V. K., Sameer, P. Evolution of surgery for active spinal tuberculosis in adults: A narrative review. J Orthopaed Rep. 3 (3), (2024).
- Yang, K., Feng, C., Zheng, B. Single-posterior revision surgery for recurrent thoracic/thoracolumbar spinal tuberculosis with Kyphosis. Operative Neurosurg. 25 (1), 59-65 (2023).
- Duan, D., Cui, Y., Gong, L. Single posterior surgery versus combined posterior-anterior surgery for lumbar tuberculosis patients. Orthopaed Surg. 15 (3), 868-877 (2023).
- Upadhyaya, G. K., Sami, A., Patralekh, M. K. Surgical management of paediatric thoracolumbar tuberculosis by a combination of anterior and posterior versus posterior only approach: A systematic review and meta-analysis. Global Spine J. 13 (1), 188-196 (2023).
- Liu, Y., Liu, Q., Duan, X. One-stage posterior transpedicular debridement, hemi-interbody and unilateral-posterior bone grafting, and instrumentation for the treatment of thoracic spinal tuberculosis: a retrospective study. Acta Neurochir. 166 (1), 65 (2024).
- Jitpakdee, K., Liu, Y., Heo, D. H. Minimally invasive endoscopy in spine surgery: Where are we now. Eur Spine J. 32 (8), 2755-2768 (2023).
- Tang, K., Goldman, S., Avrumova, F. Background, techniques, applications, current trends, and future directions of minimally invasive endoscopic spine surgery: A review of literature. World J Orthoped. 14 (4), 197 (2023).
- Zhang, Z., Hao, Y., Wang, X. Minimally invasive surgery for paravertebral or psoas abscess with spinal tuberculosis- A long-term retrospective study of 106 cases. BMC Musculoskelet Disord. 021, 1-9 (2020).
- Liu, Z., Xu, Z., Zhang, Y. Endoscopy-assisted anterior cervical debridement combined with posterior fixation and fusion for the treatment of upper cervical spine tuberculosis: A retrospective feasibility study. BMC Musculoskelet Disord. 23 (1), 126 (2022).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved