Method Article
Unilateral Biportal Endoscopy for the Treatment of Lumbar Disc Herniation
In This Article
Summary
Presented here is a step-by-step surgical protocol of unilateral biportal endoscopy (UBE), a minimally invasive approach for treating lumbar disc herniation. By using two ports, surgical accuracy and flexibility are enhanced. This article provides a comprehensive description of UBE and highlights the practical application of this approach in clinical practice.
Abstract
Unilateral biportal endoscopy (UBE) is a minimally invasive spinal surgery technique increasingly employed in treating degenerative lumbar diseases, such as lumbar disc herniation, lumbar spinal stenosis, and spondylolisthesis. In UBE, two independent yet interconnected surgical channels are established-one for the endoscope and the other for surgical instruments-providing a broad and clear surgical field of view. UBE offers several advantages over traditional open surgery, including reduced tissue damage, shorter hospital stays, and faster recovery times. Additionally, it combines the benefits of microscopic surgery and interlaminar endoscopy, enhancing flexibility, accuracy, and reliability during the procedure. The learning curve for UBE is shorter than that for transforaminal endoscopy, as the surgical processes closely resemble those of conventional open surgery. Despite its favorable clinical outcomes, such as reduced blood loss and shorter hospitalization, UBE carries potential complications, including epidural hematoma, dural injury, and compression of the outlet nerve root. To mitigate these risks, it is crucial to ensure appropriate patient selection, apply the correct surgical technique, and engage in careful postoperative monitoring. This article provides a detailed summary of the step-by-step surgical techniques used in UBE for treating lumbar disc herniation. It serves as a comprehensive guide to enhance practitioners' understanding of UBE. The presentation also underscores the importance of rigorous training and expertise to ensure optimal patient outcomes.
Introduction
Degenerative disc disease (DDD), also known as lumbar spinal stenosis or herniation, is a prevalent condition affecting the spinal column and stands as the primary reason for spinal surgery, particularly among elderly patients1,2,3. Standard surgical approaches for addressing lumbar disc herniation and stenosis have historically involved wide laminectomy and decompression surgery4,5. However, both procedures entail significant trauma, pain, and prolonged recovery times.
In recent years, minimally invasive spinal surgery has gained preference over open spinal surgery due to its associated benefits, including reduced trauma, diminished pain, and faster recovery6. Percutaneous endoscopic surgery is a frequently utilized minimally invasive technique, employing an endoscope to operate through small incisions in the skin. While this method offers numerous advantages over traditional surgery, technical challenges may arise, especially in cases of severe stenosis or when bilateral decompression is necessary7.
Unilateral double-door endoscopic surgery, initially developed by Campin and Sampson in 1986, has garnered increasing attention8,9. A crucial innovation in the technique was proposed and documented by D'Antoni in 199610, with substantial enhancements resulting from recent advances in double-channel technology11,12,13. Unilateral biportal endoscopic decompression (UBE) represents a percutaneous endoscopic procedure that allows surgeons to operate without constraints on the size of the working tube or channel. In UBE, two small incisions made on either side of the spinous process facilitate the completion of the operation. The use of a high-definition endoscope, coupled with continuous irrigation using normal saline, ensures a clear view of the surgical field and precise decompression6,14.
Overall, UBE stands as a significant advancement in the realm of minimally invasive spinal surgery. Its numerous advantages over traditional surgery, such as enhanced precision, reduced tissue trauma, and expedited recovery times, position it as a promising technique for addressing DDD and other spinal conditions. Indeed, studies have reported satisfactory results using UBE for treating DDD15. As double-channel technology progresses, UBE is poised to become the preferred method among spinal surgeons, aiming to provide their patients with the highest standard of care.
Protocol
This study received approval from the Ethical Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (SAHZU). Full compliance with ethical standards was consistently observed throughout the study duration. Informed written consent was obtained from all participating patients. The inclusion criteria for patients encompassed lumbar disc herniation and lateral recess stenosis, with the primary clinical presentation being unilateral lower limb neurological symptoms. Conversely, the exclusion criteria included lumbar canal stenosis with bilateral lower limb neurological symptoms, lumbar spondylolisthesis, lumbar tumors, and lumbar infections. Details of all the surgical tools and equipment are listed in the Table of Materials.
1. Patient positioning and anesthesia
- Following standard clinical practices, position the patients in the prone position for the administration of general anesthesia. Intravenous premedication with midazolam (1-2 mg) and/or fentanyl (25-150 µg) is recommended. After preoxygenation with 100% oxygen, induce anesthesia intravenously using propofol (1.5-2.0 mg/kg), with optional lidocaine (20-100 mg) and fentanyl (50-250 µg) (following institutionally approved protocols).
- Attain muscle relaxation for endotracheal intubation (for direct or video laryngoscopy) using rocuronium (0.6-1.2 mg/kg) or succinylcholine (1 mg/kg). Maintain anesthesia with propofol (75-200 mg/kg per min) or sevoflurane (1.0% to 2.0% in 40% to 70% oxygen)16.
NOTE: The precise concentration of the anesthetic agents should be determined by an experienced anesthesiologist based on the patient's condition.
- Attain muscle relaxation for endotracheal intubation (for direct or video laryngoscopy) using rocuronium (0.6-1.2 mg/kg) or succinylcholine (1 mg/kg). Maintain anesthesia with propofol (75-200 mg/kg per min) or sevoflurane (1.0% to 2.0% in 40% to 70% oxygen)16.
- Examine the patient's head for lateral tilt and ensure it does not interfere with tracheal intubation.
- Position the patient's arms comfortably on armrests located at their sides.
- Utilize cushioning to pad the patient's knees, preventing pressure points and discomfort.
- Elevate the patient's toes by padding under their shins to promote proper blood flow. Avoid the nerve pressure (Figure 1A).
- Place a cushion on the chest and pubic symphysis junction to suspend the abdomen. Gradually tilt the operating table with the head higher and the legs lower to align the target intervertebral disc as vertically as possible.
2. Skin marking and incision
- Utilizing C-arm fluoroscopy, identify the working space by targeting the superior sacral notch, the junction between the lateral aspect of the superior articular process and the sacral ala, through anteroposterior and lateral fluoroscopic views17.
- Mark the junction between the spinous process and the lower facet joint with a red line. Mark the horizontal line at the root of the spinous process with a green line. The intersection of these lines serves as the marker point.
- Create left and right incisions at the head and tail ends of the marker point for endoscope entry and instrument access. Maintain the incisions approximately 3 cm apart, with each entry length around 1.5 cm.
NOTE: The specific incision size may vary based on the surgeon's preference and patient anatomy. Consider these factors when determining the appropriate incision size for individual patients. - Ensure that the center of both incisions is 1 cm lateral to the target area to ensure accuracy (Figure 1E).
- If the iliac crest obstructs the caudal incision, create the incision medially to avoid the crest.
3. Drape preparation and connecting instruments
- Clean the surgical site with an antiseptic solution and drape the patient using sterile surgical drapes and iodine film to maintain sterility (Figure 1F-H).
- Ensure continuous saline flushing during UBE surgery, with careful attention to waterproofing and drainage treatment of the top sheet to prevent hypothermia (Figure 1I).
NOTE: Position the saline bag 50-70 cm above the surgical field to maintain the required hydrostatic pressure, typically set between 30-50 cm of water. - Establish a sterile field by opening all necessary sterile packages to prevent contamination.
- Wear sterile gloves and gowns to maintain a sterile environment.
- While preserving sterility, connect all necessary instruments and devices to their respective ports or power sources.
- Ensure that all cables and tubing are securely connected and will not be accidentally dislodged during surgery.
- Verify that all instruments work correctly before commencing the surgical procedure.
4. Establishing the working space
NOTE: UBE necessitates two small incisions-one for arthroscopic insertion and continuous saline irrigation, and the other for instrument access and saline outflow (Figure 1J-L).
- Utilize a dilator to progressively expand the paraspinal muscles layer by layer, gently pushing soft tissues away to create space. With the introduction of saline, the space is formed and ready for use (Figure 1M). Employ fluoroscopic guidance to pass serial dilators through the working portal and obturator.
- Verify the availability of all necessary equipment and ensure correct connections (Figure 1N).
- Advance the sheath to the target point through the portal (Figure 1O). Ensure that the sheath and serial dilator are placed in a triangular position at the target point using a C-arm fluoroscopic view.
- Maintain continuous irrigation of both portals with saline to ensure a clear surgical view.
- Confirm the correct positioning of both portals.
- Employ plasma blades (RF electrodes or ablation electrodes) to coagulate soft tissue and muscles to remove anatomical structures.
- Identify the surgical landmark-the root of the spinous process of L5.
5. Bone excision and soft tissue removal
- Employ a high-speed drill and Kerrison rongeur to resect the lower edge of the L5 vertebral lamina, proceeding laterally to the inner edge of the inferior articular process (Figure 2A,B).
- Continue the removal of bony landmarks until the ligaments are released from the bony structures.
- Use Kerrison forceps from the inside out to excise the ligamentum flavum tissue until the extradural fat is exposed, carefully performing cauterization for hemostasis (Figure 2C).
- Eliminate the fatty tissue surrounding the nerves and dura mater, identifying the exiting nerve roots and the dura mater (Figure 2D).
NOTE: As shown in Figure 2D, nerve roots can be identified by removing the fatty tissue around the nerves and dura mater.
6. Extraction of herniated annulus fibrosus and nucleus pulposus tissue
- Verify the position of the nerve roots.
- Employ a nerve root retractor to gently retract the nerve roots inward, exposing the herniated intervertebral disc tissue (Figure 2E-G).
- Utilize straight or curved pituitary rongeurs to remove fragments of the disc nucleus pulposus (Figure 2H-I).
- Ensure the complete removal of protruding intervertebral disc and osteophyte tissues to prevent nerve root compression (Figure 2J).
- Carefully cauterize the surrounding tissues to ensure no significant bleeding points in the field of view (Figure 2K-L).
- Observe the general view of the herniated disc nucleus, as depicted in Figure 1P.
7. Closure of the incision
- Turn off the water inlet: Before closing the incision, ensure all water sources are turned off to prevent contamination.
- Check for bleeding points: Examine the surgical site for any active bleeding points. If identified, control bleeding with pressure and/or cautery as needed.
NOTE: Be mindful of the potential risk of postoperative epidural hematoma, particularly in the absence of a Redivac drain. This is a crucial consideration, especially for those new to the field. - Suture the incision: Close the incision using a sterile 4-0 or 5-0 surgical suture, employing a technique suitable for the type of incision and the involved tissues. Ensure knots are securely tied and buried beneath the skin.
NOTE: Administer local closure therapy with a subcutaneous injection of ropivacaine. - Dress the wound: Apply sterile dressings to the closed incision site to prevent contamination and promote healing.
8. Postoperative follow-up procedures
- Initial postoperative assessment: Perform an initial assessment within 24 h post-surgery to examine the wound and monitor vital signs.
- Wound care and management: Instruct patients or caregivers on wound care, including recognizing signs of infection.
- Medication management: Prescribe pain relief and necessary antibiotics, guiding proper usage.
- Activity and rehabilitation: Restrict specific activities and recommend physical therapy or other rehabilitation measures at the appropriate time.
- Follow-up appointments: Schedule follow-up appointments to track healing progress and address any concerns.
- Patient education and support: Supply information resources on postoperative care and recovery, and inform patients about available support services.
- Emergency protocols: Furnish emergency contact details and educate patients on when urgent medical assistance is needed.
Results
From December 2020 to February 2022, a study assessed the efficacy and safety of unilateral biportal endoscopy (UBE) decompression therapy in treating patients with lumbar disc herniation and lateral recess stenosis. 104 patients (40 males and 64 females) with a mean age of 41.49 ± 16.01 years were enrolled. Of these patients, 81 cases (77.88%) had lumbar disc herniation, while 23 cases (22.12%) had lateral recess stenosis. The study group had an average follow-up period of 15.91 ± 5.69 months, and the mean surgical intervention time was 56.85 ± 12.11 min. Surgical levels ranged from L4-5 to L5-S1, with 26 cases at L4-5 and 78 cases at L5-S1 (Table 1). According to the MacNab criteria18, most patients achieved good to excellent outcomes, with 58 patients (55.77%) achieving an excellent outcome, 39 patients (37.50%) achieving a good outcome, and 7 patients (6.73%) achieving a fair outcome. No poor outcomes were reported (Table 1).
Furthermore, postoperative Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) scores14 showed significant improvement compared to preoperative scores, indicating symptom relief and an improvement in the quality of life for patients. Specifically, the VAS score decreased from 7.77 ± 0.89 preoperatively to 2.46 ± 1.30 at the last follow-up (p < 0.001), while the ODI score decreased from 52.25 ± 13.95 preoperatively to 19.68 ± 8.14 postoperatively (p < 0.001) (Table 2).
Importantly, there was no neurological deterioration or serious complications such as dura tear, nerve root injury, postoperative hematoma requiring reoperation, or infection within one year after surgery. Postoperative magnetic resonance imaging (MRI) showed significant improvement in compression-related anatomical findings, while clinical evaluation was used to assess symptom improvement. This finding further supports the safety and effectiveness of lumbar UBE surgery (Figure 3).

Figure 1: UBE preparations. (A) The patient is positioned in a prone stance. (B-D) Skin marked with red (outer edge) and green (target area) lines. (E) Incision markers for the working portal, spaced approximately 3 cm apart. (F-H) The patient was draped with sterile surgical drapes and iodine film for sterility. (I) Waterproofing and drainage treatment of the top sheet. (J-L) Incision creation. (M) Surgical space created using a dilator. (O) The scopic sheath advanced to the target point, ensuring a triangular position with the serial dilator. (P) General view of the prominent nucleus pulposus. Please click here to view a larger version of this figure.

Figure 2: UBE surgical steps. (A) Grinding upwards from the inferior edge of the ipsilateral lamina to the ligament attachment point. (B) Lamina removal in the surgical area using lamina bite forceps. (C) Removal of the superficial layer of the ligament, preserving the deep layer as nerve-protecting tissue. (D) Identification of the exiting nerve root. (E,F) Exposure of the annulus below the root. (G,H) Complete removal of the bulging disc and osteophytes. (I-K) Careful coagulation for hemostasis to avoid bleeding. (L) General view of the L5 nerve root after complete release. Please click here to view a larger version of this figure.
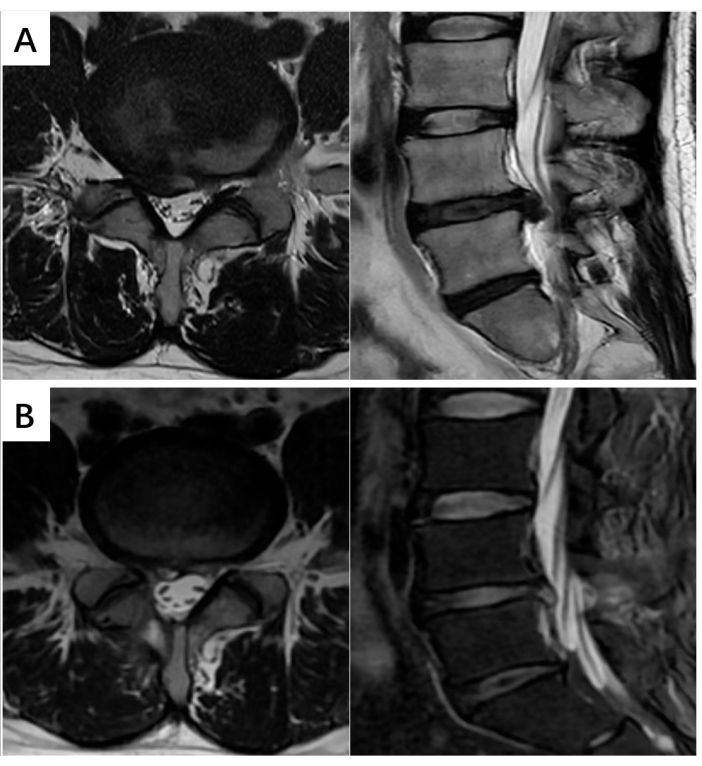
Figure 3: MR images of lumbar disc herniation. (A) Preoperative T2-weighted sagittal and axial images showing high-grade spinal canal stenosis and intervertebral disc herniation at the L4-L5 level. (B) Postoperative T2-weighted sagittal and axial images revealing successful alleviation of spinal cord compression symptoms. Please click here to view a larger version of this figure.
| Factors | Patients (n = 104) |
| Age (years) | 41.49± 16.01 |
| Sex | |
| M | 40 |
| F | 64 |
| Diagnosis | |
| Lumbar Disc Herniation, n(%) | 81, 77.88% |
| Lateral Recess Stenosis, n(%) | 23, 22.12% |
| Levels involved | |
| L4-L5 | 26 |
| L5-S1 | 78 |
| Follow-up period (months) | 15.91 ± 5.69 |
| Operation time (min) | 56.85 ± 12.11 |
| MacNab criteria, n(%) | |
| Excellent | 58, 55.77% |
| Good | 39, 37.50% |
| Fair | 7, 6.73% |
Table 1: Patient characteristics. Values are presented as mean ± standard deviation unless otherwise indicated.
| Parameter | Preoperative | Final follow up | P value |
| Visual analogue scale (VAS) | 7.77 ± 0.89 | 2.46 ± 1.30 | <0.001 |
| Oswestry disability index (ODI) | 52.25 ± 13.95 | 19.68 ± 8.14 | <0.001 |
Table 2: Preoperative and final follow-up assessment of VAS and ODI. Values are presented as mean ± standard deviation. P <0.05 was extremely significant statistically.
Discussion
The conventional standard treatment for lumbar disc herniation is lumbar microscopic discectomy, with a conventional laminectomy, to remove the affected disc4. This method poses a risk of postoperative spinal instability and persistent back pain. Percutaneous transforaminal endoscopic discectomy is a minimally invasive technique that limits soft tissue damage and protects the posterior ligamentous complex and other biomechanical systems. Several studies have demonstrated its effectiveness in treating degenerative lumbar spine conditions. However, despite these promising results, whether minimally invasive discectomy is superior to traditional surgery remains unclear due to insufficient evidence18,19.
UBE is a minimally invasive spinal surgery with several advantages over microscopic discectomy of the lumbar spine, such as better preservation of bone and muscle structure, a shorter hospital stay, and a smaller incision. Surgeons have now contributed several technological advancements towards this method, including a unilateral access dual-channel strategy, a shift from a lateral to a prone position for the patient, and radiofrequency ablation tips (plasma tips) to enhance soft tissue processing. In addition, the surgical indications for UBE have expanded to include spinal stenosis, foraminal stenosis, and extreme lateral disc herniation. With the introduction of decompression fusion techniques, UBE can now be used to treat several degenerative diseases of the lumbar, cervical, and thoracic spine, aided by specialized surgical instruments and standardized procedures.
In 2018, Kim and colleagues conducted a retrospective study involving 141 patients with DDD who underwent single-segment discectomy18. The VAS scores of the UBE group were superior to those of the lumbar microscopic discectomy group as early as 1 week after surgery, indicating the potential of UBE in this setting. As an innovative surgical approach developed by combining several surgical techniques, UBE provides unrestricted access to the contralateral region and even the intervertebral foramen, thus allowing the use of specialized instruments such as laminar occlusion forceps, bone chisels, circular saws, and retractable grinding drills. This unique feature makes it a promising option for treating DDD with minimal invasion. Moreover, the flexibility of the technique and easy operability allow the surgeon to use both hands, facilitating surgical intervention. The large field of view for microscopic surgery, the self-contained light source, and the clear structure recognition allow UBE to be readily adopted by surgeons with open surgery experience. The enhanced visibility also ensures precise and accurate surgical interventions. While significant practice is required to achieve proficiency in creating a working space for the musculoskeletal gap, once the working space is established, the surgeon can complete the intervention with minimal disruption to the surrounding tissues.
In this study, based on the MacNab criteria18, more than half of the patients (55.77%) achieved an excellent outcome, 37.50% a good outcome, and 6.73% a fair outcome. No poor outcomes were reported. Significant improvements in postoperative versus preoperative VAS and ODI scores14 were also determined, as evidenced by statistically substantial decreases consistent with symptom relief and enhanced quality of life. Importantly, no neurological deterioration or serious complications, such as dural tear, nerve root injury, postoperative hematoma requiring reoperation, or infection, were reported within 1 year after surgery. Postoperative MRI showed significant improvements in the anatomical findings related to compression. Together, these results support the safety and effectiveness of UBE decompression for treating lumbar disc herniation and lateral recess stenosis.
However, the drawbacks of UBE that may lead to surgical complications must also be noted. These include the risk of excessive hydrodilation pressure in the epidural space, which can impact the nervous system, and the prolonged use of cold saline, which may induce hypothermia20. Therefore, proper preventive measures should be taken, such as managing epidural cooling or infusion duration, to minimize potential adverse effects20. When peeling and excising the yellow ligament, it is advisable first to use a nerve dissector to separate it from the dura mater to avoid dural damage. When using a nerve root retractor to pull the nerve root, it is recommended first to separate the adhesion between the nerve root and surrounding tissues using a nerve dissector to prevent dural tearing. The segments affected by lumbar disc herniation in our study patients were L4/5 and L5/S1. In contrast, there was no involvement of the intervertebral discs from L1 to L4, contributing to the preservation of the facet joints and providing sufficient space for the operation. Surgeons should have a thorough understanding of the potential risks of UBE to minimize complications.
Although UBE shows promise as a minimally invasive surgical technique for treating DDD, further research is needed to assess its long-term effectiveness and safety compared to traditional surgical methods. With the continued development of surgical techniques, it is hoped that UBE will become an increasingly effective option for patients with DDD.
Disclosures
The authors have nothing to disclose.
Acknowledgements
None.
Materials
| Name | Company | Catalog Number | Comments |
| 4-0 or 5-0 Polydioxanone | Shandong Weigao Group Medical Polymer Co. , Ltd. | 9270504 | Their PDS sutures are typically used for soft tissue approximation and ligation. |
| Electric grinder | Guizhou Zirui Technology Co. , Ltd. | 04-14-08 | Grinding removes lamina bone and exposes ligamentum flavum tissue |
| Kerrison Rongeur Forceps | Xi'an Surgical Medical Science and Technology Co. , Ltd. | 04-03-03 | Used for biting dead bones or repairing bone stumps. |
| Minimally invasive spinal surgery channel expansion tube | Xi'an Surgical Medical Science and Technology Co. , Ltd. | 04-17-13 | Used to expand the surgical field of view. |
| Nerve stripping ion | Xi'an Surgical Medical Science and Technology Co. , Ltd. | 04-18-01 | Used for stripping or separating nerve root tissue |
| Periosteal stripping ion | Xi'an Surgical Medical Science and Technology Co. , Ltd. | 04-18-01 | Used to peel off or separate the periosteum and soft tissue attached to the bone surface. |
| Plasma Surgical Blade (RF electrode/ablation electrode) | Xi'an Surgical Medical Science and Technology Co. , Ltd. | 6825-01-03 | Used to ablate soft tissue such as muscle and fascia, or to clot the surface of muscle and nerve tissue |
| Spinal surgery using nerve hooks | Xi'an Surgical Medical Science and Technology Co. , Ltd. | 04-04-01 | Used in orthopedic surgery to expose the surgical field of view, or to peel, stretch, or occlude nerve roots during orthopedic surgery. |
References
- Hu, Q. F., Pan, H., Fang, Y. Y., Jia, G. Y. Percutaneous endoscopic lumbar discectomy for high-grade down-migrated disc using a trans-facet process and pedicle-complex approach: A technical case series. Eur Spine J. 27, 393-402 (2018).
- Katz, J. N., Zimmerman, Z. E., Mass, H., Makhni, M. C. Diagnosis and management of lumbar spinal stenosis: A review. JAMA. 327 (17), 1688-1699 (2022).
- Wu, P. H., Kim, H. S., Jang, I. T. Intervertebral disc diseases part 2: A review of the current diagnostic and treatment strategies for intervertebral disc disease. Int J Mol Sci. 21 (6), 2135 (2020).
- Rasouli, M. R., Rahimi-Movaghar, V., Shokraneh, F., Moradi-Lakeh, M., Chou, R. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. 4 (9), (2014).
- Issack, P. S., Cunningham, M. E., Pumberger, M., Hughes, A. P., Cammisa, F. P. Degenerative lumbar spinal stenosis: Evaluation and management. J Am Acad Orthop Surg. 20 (8), 527-535 (2012).
- Ahn, Y. Current techniques of endoscopic decompression in spine surgery. Ann Transl Med. 7, 169 (2019).
- Choi, C. M. Biportal endoscopic spine surgery (bess): Considering merits and pitfalls. J Spine Surg. 6 (2), 457-465 (2020).
- Choi, C. M., Chung, J. T., Lee, S. J., Choi, D. J. How i do it? Biportal endoscopic spinal surgery (bess) for treatment of lumbar spinal stenosis. Acta Neurochir (Wien). 158 (3), 459-463 (2016).
- Kambin, P., Sampson, S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res. 207, 37-43 (1986).
- De Antoni, D. J., Claro, M. L., Poehling, G. G., Hughes, S. S. Translaminar lumbar epidural endoscopy: Anatomy, technique, and indications. Arthroscopy. 12 (3), 330-334 (1996).
- Aygun, H., Abdulshafi, K. Unilateral biportal endoscopy versus tubular microendoscopy in management of single level degenerative lumbar canal stenosis: A prospective study. Clin Spine Surg. 34 (6), E323-E328 (2021).
- Kim, J. E., Choi, D. J. Unilateral biportal endoscopic decompression by 30 degrees endoscopy in lumbar spinal stenosis: Technical note and preliminary report. J Orthop. 15 (2), 366-371 (2018).
- Park, J. H., Jun, S. G., Jung, J. T., Lee, S. J. Posterior percutaneous endoscopic cervical foraminotomy and diskectomy with unilateral biportal endoscopy. Orthopedics. 40 (5), e779-e783 (2017).
- Sun, S., Wang, L., Xue, Y. 34;Inside disc out" discectomy for the treatment of discogenic lumbar spinal canal stenosis under the intervertebral foramen endoscope. Orthop Surg. 15 (1), 355-361 (2023).
- Heo, D. H., Lee, D. C., Park, C. K. Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: Biportal endoscopy, uniportal endoscopy, and microsurgery. Neurosurg Focus. 46 (5), E9 (2019).
- De Biase, G., et al. Spinal versus general anesthesia for minimally invasive transforaminal lumbar interbody fusion: Implications on operating room time, pain, and ambulation. Neurosurg Focus. 51 (6), 3 (2021).
- Park, M. K., et al. Unilateral biportal endoscopy for decompression of extraforaminal stenosis at the lumbosacral junction: Surgical techniques and clinical outcomes. Neurospine. 18 (4), 871-879 (2021).
- Kim, S. K., Kang, S. S., Hong, Y. H., Park, S. W., Lee, S. C. Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: A multicenter, retrospective analysis. J Orthop Surg Res. 13 (1), 22 (2018).
- Lubelski, D., et al. Is minimal access spine surgery more cost-effective than conventional spine surgery. Spine (Phila Pa). 39 (22), S65-S74 (2014).
- Bui, A. T., et al. Indications for and outcomes of three unilateral biportal endoscopic approaches for the decompression of degenerative lumbar spinal stenosis: A systematic review. Diagnostics (Basel). 13 (6), 1092 (2023).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved