Method Article
Treating Osteoporotic Spinal Fractures in Elderly Patients via a Modified Clinical Bone Cement Injection Technique
In This Article
Summary
Presented here is a modified procedure for minimally invasive injections of bone cement to treat osteoporotic spinal fractures in elderly patients.
Abstract
The minimally invasive injection of bone cement (MIIBC) is an effective way to treat senile osteoporotic spinal fractures (OSF) in clinical practice. However, the intraspinal dura and nerves may be damaged when the puncture needle passes through the pedicle. Therefore, in this protocol, the puncture site was optimized during the surgery, selecting the same 1-2 cm away from the surface projection of the diseased vertebra. The needle was punctured along the lateral cortex of the pedicle from the junction of the pedicle and the vertebral body into the vertebral body. Meanwhile, bone cement was used as a filling material, and the MIIBC was performed by a percutaneous puncture at the external edge of the pedicle under C-arm fluoroscopy. This modified puncture site is far away from the spinal canal as possible, thereby reducing the risk of the puncture needles penetrating the spinal canal and damaging the nerves and dura mater. In conclusion, a modified MIIBC by percutaneous lateral pedicle puncture can effectively relieve pain in elderly patients with OSF.
Introduction
Osteoporosis is a common disease among middle-aged and elderly women. Statistics show that about 54% of postmenopausal women have abnormal bone density, and the chance of vertebral fracture over the age of 50 is about 32%1. Osteoporotic spinal fractures (OSF) occur most commonly in women and are mainly compression fractures caused by direct or indirect external forces1,2. After the fracture, the sagittal balance of the spine is broken, resulting in vertebral deformation, diffuse lumbar and back pain, and kyphosis2. In addition, some patients also experience abdominal pressure and breathing difficulties3. Clinical trials have reported that the key to the treatment of OSF is the restoration of bone continuity4. Without effective and timely treatment for OSF patients, it is easy for spinal deformities, secondary nerve injury, spinal canal stenosis, angulation deformity, delayed fracture healing, and bone nonunion to occur, and the lives of the patients may even be threatened5.
Current clinical treatments for OSF include conservative treatment and surgical treatment6. Although the conservative treatment of OSF can provide temporary relief of the symptoms, the course of treatment is long, and the recovery of the injured vertebral height is poor7. Overall, the traditional conservative treatment of OSF requires patients to stay in bed for a long time, and its overall efficacy is not ideal. For now, clinical, surgical treatment for OSF embraces traditional open internal fixation, Sextant minimally invasive pedicle screw fixation, percutaneous vertebroplasty (PVP), and percutaneous kyphoplasty (PKP)8. Similar to the conservative treatment of long-term bed rest, traditional open internal fixation can lead to aggravated osteoporosis, deep venous thrombosis of the lower limbs, lung infection, urinary tract infection, calculi and decubitus, and other complications, which seriously affect the quality of life of the patient and cause a high disability rate9. Nevertheless, Sextant minimally invasive pedicle screw fixation is a complicated operation with a long operation time, and the operation itself can further aggravate secondary injury of the diseased vertebra10. Obviously, the characteristics of lost vertebral bone density in senile OSF patients are more likely to lead to screw loosening and even removal, resulting in the failure of the internal fixation surgery11.
As commonly used clinical treatments for a senile osteoporotic spinal fracture, PVP and PKP can restore vertebral function and improve the mobility of patients with higher surgical safety and better postoperative pain relief. However, the merits and demerits of both in treating osteoporotic spinal compression fractures are still debated. High-pressure perfusion in PVP surgery can cause leakage of the bone cement into the vertebrae, thus damaging the spinal cord and nerve roots and reducing the surgical effect to a certain extent12. Compared with PVP, PKP can observably reduce and avoid the risk of bone cement leakage, but the operation is longer13. Inevitably, the use of a balloon to dilate the diseased vertebra during PKP surgery also carries a potential risk of secondary vertebral injury14. Therefore, in this study, on the basis of PVP, elderly patients with OSF were treated by optimizing the puncture site during surgery, thus avoiding the risk of the spinal cord and nerve injury caused by the puncture itself. In this protocol, the case of a 68-year-old female patient with OSF who underwent a modified minimally invasive injection of bone cement (MIIBC) for the treatment of a seventh thoracic vertebra fracture is presented in detail.
Protocol
The surgical operation using MIIBC for the treatment of an osteoporotic fracture of the seventh thoracic vertebra in a 68-year-old woman was approved by the Ethics Committee of Linfen People's Hospital of Shanxi Medical University (T20220829006). The patient provided written informed consent.
1. Collection and recording of the patient's medical history
- Communicate with the patient to determine the history of trauma, heavy lifting, bumpy rides, jerking, or even coughing.
NOTE: The main clinical manifestations of OSF are as follows: (1) pain, which can be acute or chronic lumbago and back pain or body pain and even obvious limitations in rolling up and down activities and walking activities; (2) spinal deformation, which is mainly manifested as kyphosis, lateral curvature, shortened height, a humpback, and thoracic deformity. In cases of spinal cord compression, severe complications may occur, such as paraplegia and abdominal compression, which may affect cardiopulmonary function.
2. Pre-surgical examinations
- Physical examination
- Check for percussion pain and pressing pain in the chest, waist, and back. Check the lower extremities for sensory and motor changes.
- Magnetic resonance imaging (MRI)
- Perform MRI (see Table of Materials) to identify acute or old vertebral fractures, as shown in Figure 1.
NOTE: Newly fractured vertebrae show obvious edema around the tissue. Surgery is prohibited for old vertebra fractures.
- Perform MRI (see Table of Materials) to identify acute or old vertebral fractures, as shown in Figure 1.
- X-ray examination
- Perform an X-ray (see Table of Materials) to examine the vertebral changes and bone density in the cuneiform lesions, as shown in Figure 2.
- Computed tomography (CT) examination
- Perform CT (see Table of Materials) to examine the integrity of the posterior wall of the fractured vertebra, and determine if a vertebral fracture mass is present in the vertebral canal, as shown in Figure 3.
- Bone mineral density (BMD) examination
- Perform dual-energy X-ray absorptiometry (DXA) (see Table of Materials) to measure the BMD of the spine, as shown in Figure 4.
3. Patient positioning
- Place a chest pad (see Table of Materials) under the patient's chest to maintain the patient in a prone position. Place a soft pad (see Table of Materials) under the lower leg to bend the knee to 20°. See Figure 5 for the specific details on the patient positioning.
NOTE: Remind the patient to relax the thoracolumbar and back muscles to facilitate the later puncture operation.
4. Surgical procedure
- Perform intraoperative digital radiography (DR) and puncture localization.
- Fix the Kirschner wire (see Table of Materials) on the body surface, and use the C-arm of the DR machine (see Table of Materials) for intermittent imaging to identify and label the surface projection of the diseased pedicle, as shown in Figure 6.
NOTE: The location of the diseased pedicle should be evaluated comprehensively based on the results of step 3.1, step 4.1, step 5.1, and step 6.1.
- Fix the Kirschner wire (see Table of Materials) on the body surface, and use the C-arm of the DR machine (see Table of Materials) for intermittent imaging to identify and label the surface projection of the diseased pedicle, as shown in Figure 6.
- Perform needle puncture and bone cement injection.
- Locate the injection point at 1-2 cm outside the surface projection of the outer edge of the pedicle. Perform full invasive anesthesia with 2% lidocaine (see Table of Materials) along the skin of the puncture site toward the pedicle, as shown in Figure 7.
NOTE: The puncture point is not at the body surface projection of the injured pedicle but is 1-2 cm outside the body surface projection on the outer edge of the pedicle. - Under lateral DR imaging, adjust the orientation of the puncture needle to be consistent with the midline of the seventh thoracic vertebra, and strike the puncture needle to the outer edge of the pedicle with a surgical hammer (see Table of Materials). Next, push the puncture needle to the anterior vertebral 1/3 junction under lateral DR imaging.
NOTE: When the tip of the puncture needle reaches the posterior edge of the vertebral body, the DR imaging above the prone position should show that the puncture needle passes right over the outer edge of the pedicle. When the puncture needle reaches the anterior 1/3 junction of the vertebral body, the DR imaging above the prone position should indicate that the tip of the puncture needle is located in the center of the vertebral body. - Fill the syringe with the prepared viscous bone cement (see Table of Materials), and slowly inject it into the vertebra under lateral DR imaging. Insert the pillow inner to push the bone cement remaining inside the puncture needle (see Table of Materials) into the vertebral body.
- Pull out the puncture needle by turning it backward. After pressing the puncture site for 3-5 min, wrap the puncture site with sterile surgical gauze (see Table of Materials), as shown in Figure 8.
NOTE: Bone cement should be freshly prepared when being used. If obvious leakage is found during the injection of the bone cement, the injection should be terminated immediately.
- Locate the injection point at 1-2 cm outside the surface projection of the outer edge of the pedicle. Perform full invasive anesthesia with 2% lidocaine (see Table of Materials) along the skin of the puncture site toward the pedicle, as shown in Figure 7.
5. Postoperative care
- Administer oxygen, and monitor the vital signs of the patient in a supine position for 6 h after surgery.
NOTE: On the first day after surgery, the patient can stand and walk under the protection of the lumbar support device. If the thoracolumbar X-ray re-examination is normal, the patient can be discharged from the hospital 2-3 days after surgery.
Results
The OSF patient selected for the modified MIIBC had no history of trauma, heavy lifting, bumpy rides, jerking, or even coughing. Further physical examination showed that the patient had no percussion pain or pressing pain in the chest, waist, or back and had normal sensation and movement in the lower limbs. A new vertebral fracture was first identified in the seventh thoracic vertebra with perivertebral edema using MRI imaging (Figure 1). After that, the X-ray examination demonstrated a vertebral wedge injury and reduced vertebral density in the seventh thoracic vertebra (Figure 2). Conforming with this, the CT results also confirmed that the integrity of the posterior wall of the fractured seventh thoracic vertebra was destroyed, and no fracture material had entered the spinal canal (Figure 3). DXA data from the lumbar spine again suggested that the patient had decreased BMD, as shown by the T-score of less than −2.5 (Figure 4 and Table 1). Together, the above data indicated that the patient had symptoms of OSF at the seventh thoracic vertebra and was eligible for surgical treatment with modified MIIBC.
According to the patient's operative posture, as shown in Figure 5, intraoperative DR imaging was used to assist in determining the body surface projection of the pedicle of the seventh thoracic vertebra (Figure 6). Meanwhile, the surface location of the surgical puncture for the modified MIIBC was markedon the back of the patient (Figure 6). After routine surgical site disinfection, the local puncture site was exposed (Figure 7). Guided by intraoperative DR imaging from the side of the patient and from above the patient in the prone position, the puncture needle was discreetly delivered to the pedicle of the seventh thoracic vertebra (Figure 7). Next, the prepared bone cement was slowly injected into the diseased pedicle (Figure 8). Finally, the puncture site was pressed and bandaged after the surgery (Figure 8).
After modified MIIBC surgery in 20 elderly patients with OSF, an increase in the anterior and middle vertebral height was found compared with pre-operative treatment. Moreover, the Cobb angle was reduced, suggesting that modified MIIBC can effectively relieve symptoms in elderly patients with OSF (Table 2).
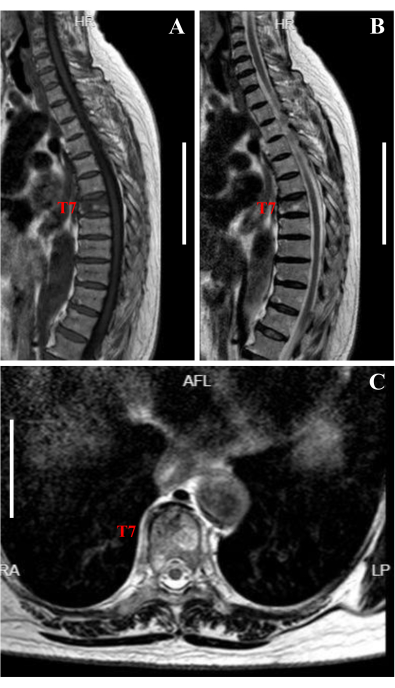
Figure 1: Pre-operative MRI spinal image. (A) The sagittal T1 image showed low-signal and wedge-shaped vertebral changes in the seventh thoracic vertebra (T7) compared to the normal vertebra. Scale bar: 10 cm. (B) The sagittal T2 image of the diseased seventh thoracic vertebra disclosed locally high signals, indicating a fresh fracture and compression of the vertebral height. Scale bar: 10 cm. (C) The coronal T2 image showed a localized hyper-signal in the diseased seventh thoracic vertebra, suggesting a fresh fracture. The posterior wall of the diseased vertebra was intact, and the spinal cord was not compressed in the spinal canal. Scale bar: 6 cm. Please click here to view a larger version of this figure.
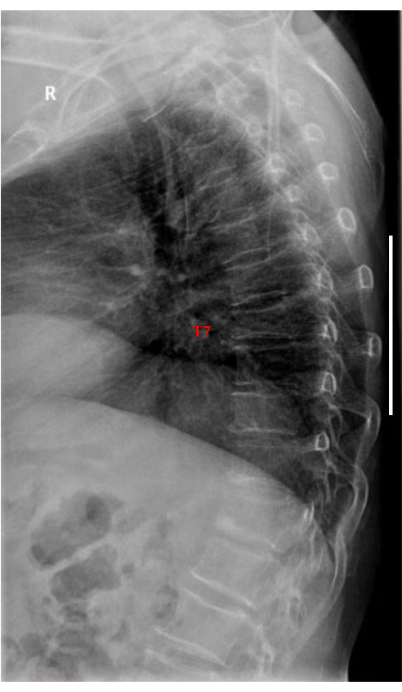
Figure 2: Pre-operative X-ray spinal and bone density image. DR imaging of the thoracic vertebra showed the lateral collapse and compression of the seventh thoracic vertebra but could not distinguish between old and fresh fractures. Scale bar: 11 cm. Please click here to view a larger version of this figure.

Figure 3: Pre-operative CT spinal image. Sagittal (A, scale bar: 11 cm), Coronal (B, scale bar: 11 cm), and transverse (C, scale bar: 8 cm) imaging showed that the posterior wall of the vertebral body was intact, with no fracture mass entering the spinal canal. Please click here to view a larger version of this figure.

Figure 4: Pre-operative DXA spinal BMD image of the lumbar vertebrae. DXA imaging determined the vertebral body area (cm2), the bone mineral content (g), and the BMD (g/cm2) from the first to the fourth lumbar vertebrae (L1 to L4). The value of BMD (g/cm2) = bone mineral content (g)/area (cm2). Coefficient of variation of the total BMD = 1.0%; acf = 1.037; bcf = 1.006; TH = 8.213. Scale bar: 5 cm. Please click here to view a larger version of this figure.

Figure 5: Patient positioning for the MIIBC. The patient lies prone on the operating table with relaxed thoracolumbar and back muscles and bends their knee 20° to facilitate the operator's puncture operation during the process of the MIIBC. Please click here to view a larger version of this figure.

Figure 6: Intraoperative DR image and puncture localization. (A) Panoramic view of the DR vertebral imaging. (B) The diseased vertebrae in the DR image. (C) Body surface projection marker of the diseased vertebrae. Scale bar: 1.7 cm. Please click here to view a larger version of this figure.

Figure 7: The whole process of the minimally invasive puncture. (A) Thorough sterilization of the back surgery area. (B) Exposure of the local surgical window. (C) Local anesthesia of the tissue surrounding the puncture. (D) Location-based puncture. (E) Reconfirmation of the position using an intraoperative DR image. (F) DR imaging of the puncture needle position from the side of the patient. Scale bar: 3.4 cm. (G) DR imaging of the puncture needle position from above the patient in the prone position. Scale bar: 3.4 cm. Please click here to view a larger version of this figure.
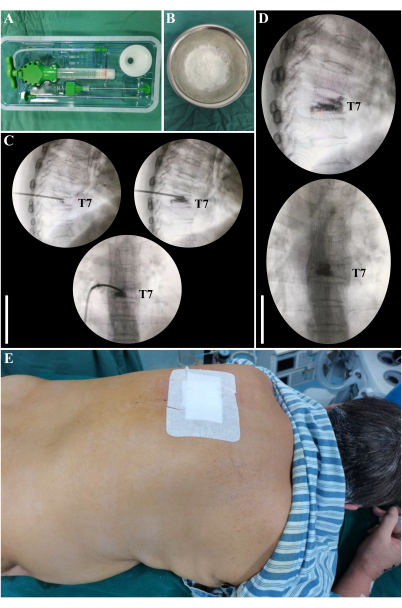
Figure 8: Intraoperative dynamic continuous injection of bone cement guided by DR imaging. (A) Bone cement injection set. (B) Bone cement item. (C) DR imaging-guided continuous injection of bone cement. Scale bar: 6 cm. (D) Reconfirmation of the bone cement injection site by DR imaging from the side of the patient (panel top) and from above the patient in the prone position (panel below). Scale bar: 5 cm. (E) Sterile surgical bandage at the puncture site. Please click here to view a larger version of this figure.
Table 1: Health status results of the first to fourth lumbar vertebrae based on DXA examination. Please click here to download this Table.
Table 2: Data of the diseased vertebrae in 20 elderly patients with OSF before and after performing the modified MIIBC. Please click here to download this Table.
Discussion
Traditional open internal fixation is used with patients who have the neurological symptoms of a vertebral compression fracture and a fractured mass entering the spinal canal and pressing on the spinal cord and nerve roots15. This technique is especially suitable for individuals with severe violent vertebral trauma, such as from a car accident or falling from height. This kind of emergency surgery usually requires spinal canal decompression, which has a long operation time and a large area of trauma16. During surgery under general anesthesia, the vertebra must be exposed, meaning there is a high risk of bleeding17. At the same time, some normal tissues need to be destroyed to relieve the compression of the nerve and spinal cord18. Unfortunately, despite the longer post-operative rehabilitation, the damaged nerve function may not recover completely. Sextant minimally invasive pedicle screw fixation with general anesthesia is suitable for patients under 60 years of age without neurological symptoms who have vertebral compression fractures in which fracture fragments have not entered the spinal canal19. The advantage of this technique is that the proper intraoperative position correction of compression fractures can enhance the internal fixation and facilitate early ambulation. However, the intraoperative screw may damage the spinal canal, nerve, and spinal cord, and the internal screw needs to be removed 1 year after surgery.
For elderly patients with osteoporotic vertebral compression fractures caused by coughing and bending, PVP is a more reasonable and sensible clinical option20. After minimally invasive surgery under local anesthesia, the patient can get out of bed and walk with perceptible pain relief. However, bone cement can unpredictably leak into the spinal canal and damage the nerves and spinal cord. PKP has similar indications and surgical risks compared to PVP and can better correct and reset fractured vertebrae, but PKP has the disadvantage of higher costs21.
Across patients, there are large anatomical differences in the vertebral pedicle, as the vertebral pedicle in some patients is congenitally thin; in these patients, the traditional puncture needle entering the vertebral body through the vertebral pedicle may break into the spinal canal, thus damaging the dural sac and causing cerebrospinal fluid leakage or nerve injury. To reduce these complications, in this protocol, the puncture needle is inserted into the vertebral body along the lateral side of the pedicle cortex. In this way, the puncture needle approach can be moved away from the spinal canal, thus reducing the risk of cerebrospinal fluid leakage or nerve damage. In conclusion, the modified MIIBC for the treatment of OSF in elderly patients shows good clinical outcomes, as indicated by the increased vertebral height and reduced Cobb angle after surgery in this study (Table 2). The modified MIIBC may be a more appropriate surgical option for patients over 55 years of age with osteoporotic vertebral compression fractures, intact vertebral posterior walls, vertebral metastases, and vertebral hemangioma. In contrast, it is not recommended for individuals who have vertebral compression fractures that compress the nerves and spinal cord and neurological symptoms or spinal stenosis requiring decompression. Compared with existing surgical procedures, the modified MIIBC significantly avoids or reduces the potential risk of intraoperative nerve and spinal cord injury. However, the clinical indications, contraindications, and potential postoperative risks of this procedure still require more clinical exploration. Meanwhile, it is worth conducting further clinical trials to determine whether a modified MIIBC via a bilateral injection through the vertebra may be more effective.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This work was supported by the Key Medical Research Project of Shanxi Province (2020XM51).
Materials
| Name | Company | Catalog Number | Comments |
| Bone cement | Heraeus Medical GmbH | 61805335 | |
| Chest pad | Hengshui Hejia Medical Device Co., Ltd. | 1.00297E+13 | |
| Computed tomography instrument | General Electric Company | Discovery CT750 HD | |
| Dualenergy X-ray absorptiometry | General Electric Company | Discovery XR656 | |
| Kirschner wire | Tianjin Yutong Medical Device Factory | 210401 | |
| Lidocaine | Shiyao Silver Lake Pharmaceutical Co., Ltd. | C22B042 | |
| Nuclear magnetic resonance apparatus | General Electric Company | Achieva 1.5T | |
| Povidone iodine solution | Wen Shui Greatly Industrial Co., Ltd. | 20220801 | |
| Puncture needle | Dragon Crown Medical Co., Ltd. | 22040601 | |
| Soft pad | Yueyang Zhengyang Medical Device Co., Ltd. | HRT445 | |
| Sterile covering | Suqian Hongzhilong E-commerce Co., Ltd. | 56200331882 | |
| Sterile surgical gauze | Hainuo Group Co. Ltd. | 7918087 | |
| Surgical hammer | Hengshui Wankai Trading Co., Ltd. | 5.20808E+11 | |
| Syringe | Shandong Weigao Group Medical Polymer Co., Ltd. | 20220101 | |
| Vertebroplasty bone cement filler set | Shenzhen Hanqiang Medical Device Co., Ltd. | TF210301 | |
| X-ray instrument | Shenzhen Rayvision Technology Co., Ltd. | ALC-200H |
References
- Zhang, B., Li, T., Wang, Z. Efficacy and complications of different surgical modalities of treating osteoporotic spinal compression fracture in the elderly. American Journal of Translational Research. 14 (1), 364-372 (2022).
- Kang, C. N., et al. et al.Cumulative incidence and factors associated with subsequent vertebral compression fractures: A nationwide population-based study. World Neurosurgery. 161, e90-e100 (2022).
- Yao, X., Liu, M., Jin, F., Zhu, Z. Comprehensive analysis of differentially expressed circular RNAs in patients with senile osteoporotic vertebral compression fracture. BioMed Research International. 2020, 4951251 (2020).
- Zhai, W., et al. The clinical effect of percutaneous kyphoplasty for the treatment of multiple osteoporotic vertebral compression fractures and the prevention of new vertebral fractures. International Journal of Clinical and Experimental Medicine. 8 (8), 13473-13481 (2015).
- Yin, H., He, X., Yi, H., Luo, Z., Chen, J. Analysis of the causes on poor clinical efficacy of kyphoplasty performed in unilateral transpedicular puncture for the treatment of senile osteoporotic vertebral compression fractures. Scientific Reports. 9 (1), 1498 (2019).
- Qin, Z., et al. Transpedical interbody bone grafting in the treatment of senile osteoporotic vertebral fracture. Pakistan Journal of Medical Sciences. 33 (5), 1166-1170 (2017).
- Xu, J. C., Wu, G. H., Zhou, L. L., Yang, X. J., Liu, J. T. Two unilateral puncturation comparative analyses of multiple-level fresh osteoporotic vertebral body compression fractures treated with percutaneous vertebroplasty guided by C-arm fluoroscopy or in senile patients. European Review for Medical and Pharmacological Sciences. 21 (7), 1456-1461 (2017).
- Anderson, P. A., Froyshteter, A. B., Tontz, W. L. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. Journal of Bone and Mineral Research. 28 (2), 372-382 (2013).
- Brodano, G. B., et al. Vertebroplasty: Benefits are more than risks in selected and evidence-based informed patients. A retrospective study of 59 cases. European Spine Journal. 20 (8), 1265-1271 (2011).
- Yu, D., et al. on the effect of different surgical methods on the treatment of senile osteoporotic spinal compression fractures and the influencing factors of complications. Evidence-Based Complementary and Alternative Medicine. 2021, 1599470 (2021).
- Demir, S. O., Akin, C., Aras, M., Köseoğlu, F. Spinal cord injury associated with thoracic osteoporotic fracture. American Journal of Physical Medicine & Rehabilitation. 86 (3), 242-246 (2007).
- Li, H., et al. Effects of rosuvastatin and zoledronic acid in combination on the recovery of senile osteoporotic vertebral compression fracture following percutaneous vertebroplasty. Journal of International Medical Research. 48 (5), (2020).
- Kobayashi, K., Shimoyama, K., Nakamura, K., Murata, K. Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. European Radiology. 15 (2), 360-367 (2005).
- Sun, Z. G., et al. Assessment of percutaneous vertebroplasty and percutaneous kyphoplasty for treatment of senile osteoporotic vertebral compression fractures. China Journal of Orthopaedics and Traumatology. 23 (10), 734-738 (2010).
- Spiegl, U. J., et al. The conservative treatment of traumatic thoracolumbar vertebral fractures. Deutsches Arzteblatt International. 115 (42), 697-704 (2018).
- Muratore, M., Ferrera, A., Masse, A., Bistolfi, A. Osteoporotic vertebral fractures: predictive factors for conservative treatment failure. A systematic review. European Spine Journal. 27 (10), 2565-2576 (2018).
- Robinson, Y., Heyde, C. E., Försth, P., Olerud, C. Kyphoplasty in osteoporotic vertebral compression fractures--guidelines and technical considerations. Journal of Orthopaedic Surgery and Research. 6, 43 (2011).
- Majumdar, S. R., et al. Interventions to increase osteoporosis treatment in patients with 'incidentally' detected vertebral fractures. The American Journal of Medicine. 125 (9), 929-936 (2012).
- Cimatti, M., et al. Pure percutaneous pedicle screw fixation without arthrodesis of 32 thoraco-lumbar fractures: Clinical and radiological outcome with 36-month follow-up. European Spine Journal. 22, S925-S932 (2013).
- Dai, F. Q., Du, Y., Luo, L. X., Zhang, Y. Q. Treatment of serious burst thoracolumbar fracture with posterior pedicle screw fixation, transpedicular bone grafting and vertebral canaloplasty. China Journal of Orthopaedics and Traumatology. 23 (7), 504-506 (2010).
- Movrin, I., Vengust, R., Komadina, R. Adjacent vertebral fractures after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: A comparison of balloon kyphoplasty and vertebroplasty. Archives of Orthopaedic and Trauma Surgery. 130 (9), 1157-1166 (2010).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved