Method Article
Application of Stand-Alone Oblique Lateral Interbody Fusion in L4-5 Lumbar Diseases
In This Article
Summary
This study describes the application of oblique lateral interbody fusion in lumbar spinal surgeries.
Abstract
Lumbar spine diseases often cause lower back pain, lower extremity pain, numbness, and paresthesia. In severe cases, intermittent claudication may occur, affecting the quality of life of patients. Surgery is often required when conservative treatment fails, or when patients' symptoms become unbearable. Surgical treatments include laminectomy and discectomy, as well as interbody fusion. The main purpose of laminectomy and discectomy is to relieve nerve compression; however, recurrence is common due to spinal instability. Interbody fusion improves stability while relieving nerve compression and significantly reduces the risk of recurrence compared to non-fusion surgery. Nonetheless, conventionally posterior intervertebral fusion requires separation of the muscles to expose the operated segment, which causes more trauma to the patient. In contrast, the oblique lateral interbody fusion (OLIF) technique achieves spinal fusion with minimal trauma to the patients and shortens the recovery time. This article introduces procedures of stand-alone OLIF surgery performed in the lumbar spine, providing a reference for other spine surgeons.
Introduction
Lumbar spine disorders are a global economic concern, with affected patients experiencing lower quality of life1. The treatment of lumbar spine diseases can be divided into two categories: conservative and surgical treatment. Conservative treatment includes rest, oral nonsteroidal drugs, massage, and physical therapy. For instance, studies have shown that estrogen can be used to delay degeneration of the intervertebral disc, thus providing a basis for its treatment of lumbar spine disease2,3. For patients who have failed in conservative treatment, surgery is typically required to treat lumbar spine diseases. Among the surgical methods used for this cohort, interbody fusion is generally preferred.
Briefly, the techniques reported consist of anterior lumbar interbody fusion (ALIF), direct lateral interbody fusion (DLIF), extreme lateral interbody fusion (XLIF), oblique lateral interbody fusion (OLIF), posterior lumbar interbody fusion (PLIF), and transforaminal lumbar interbody fusion (TLIF)4,5. Among these surgical approaches, OLIF has its unique advantages. In comparison with DLIF and XLIF, OLIF has been shown to reduce the incidence of postoperative hip flexion weakness and thigh numbness6,7. Moreover, compared with ALIF, surgeries with OLIF have a lower risk of both postoperative retrograde ejaculation and damage of blood vessels anterior to the vertebral body8. Nonetheless, it is worth mentioning that PLIF and TLIF techniques exhibit a good operative field, which could reduce damage to important structures; the placement of pedicle screws used by these methods could reduce the probability of non-fusion of the interbody cage. Nonetheless, compared with OLIF, PLIF and TLIF require intraoperative muscle dissociation and stretching the muscle for an extended period of time, which could result in increased intraoperative blood loss, slow wound healing, and prolonged patient recovery time9,10,11.
By harnessing the OLIF approach, the intervertebral site can be accessed through the space between the anterior border of the psoas muscle and the major abdominal vessels. The surgery is performed by removing the diseased disc and implanting an interbody cage. Because of the reduced damage to muscle, OLIF can minimize intraoperative blood loss and operation time, shortening patients' postoperative recovery. In addition, earlier studies have shown that the placement of interbody cages can boost restoration of the disc height and patients' physiological curvature of the spine6,12,13,14,15,16. In the present study, the surgical procedures of stand-alone OLIF for the treatment of L4-5 lumbar diseases are introduced in detail.
Protocol
This study has been approved by the Ethics Committee of the Third Hospital of Hebei Medical University. The patients signed informed consent, consented to be filmed, and allowed the investigators to use their surgical data.
1. Patient selection
- Select patients based on the following inclusion criteria.
- Select patients for whom conservative treatment time was longer than 3 months and to which the patients responded poorly.
- Select patients whose symptoms and signs were consistent with the imaging findings.
- Select patients whose magnetic resonance imaging (MRI) of the lumbar spine shows a width greater than 1 cm between the psoas muscle and the anterior border of the vertebral artery.
- Select patients with no significant variants on abdominal vascular examination.
- Apply the following exclusion criteria.
- Exclude patients with spinal canal infection and tumor complications.
- Exclude patients with spinal stenosis due to severe facet joint hyperplasia and prolapse of the nucleus pulposus.
- Exclude patients with severe lumbar spondylolisthesis greater than grade III.
- Exclude patients with a history of abdominal surgery.
2. Preoperative preparation
- Instruct the patient to undergo lumbar computed tomography (CT), lumbar MRI, and lumbar X-ray examination. Perform cardiovascular and cerebrovascular, and abdominal vascular examinations to identify and better manage risk factors to ensure safety of the operation17,18.
- Advise the patient on skin preparation of the surgical site preoperatively, with a fasting requirement of 12 h before the surgery.
- On the day of the operation, after the administration of general anesthesia with endotracheal intubation, place the patient on the operating table in a right-sided lateral decubitus position.
- Insert a cushion beneath the right abdomen, which is slightly tilted backward depending on the target intervertebral disc, in order to obtain adequate access to the physiologic OLIF corridor between the psoas muscle and the vena cava anteriorly.
- Choose the left abdomen of the patient as the surgical area.
- Ensure that the patient remains in the correct position for the surgery. Secure the patient with tape and confirm the operation stage.
3. Starting the operation
- Place a square locator on the left abdomen of the patient. Ensure the upper and lower edges of the locator correspond to the upper and lower vertebral bodies of the diseased intervertebral disc, and the anterior and posterior edges correspond to the anterior and posterior edges of the diseased intervertebral disc.
- Confirm the projection of the target segment on the patient's skin with X-ray fluoroscopy. Mark the surgical site (Figure 1).
- After identifying the surgical site, disinfect the incision area, lay sheets, and prepare surgical instruments.
- Make a 4-5 cm skin incision parallel to the external oblique muscle fibers. Separate the aponeurosis of the external oblique muscle, the transverse abdominis, and the transverse abdominal fascia bluntly with fingers (Figure 2).
- Use long-handled forceps to clamp the peanut-like gauze mass to expose the surgical intervertebral space between the abdominal vascular sheath and the psoas major muscle.
- After completing exposure of the target intervertebral space, insert Kirschner wire and perform intraoperative X-ray examinations to confirm that the exposed segment is the surgical segment (Figure 3A).
- After completing identification of the intervertebral space, insert the dilation tubes successively for expansion. Confirm the position of the expansion channel by intraoperative X-ray (Figure 3B).
- Attach the retractor to the operating table using the universal arm and operating table clips. Ensure that the channel does not move during the surgery, and then place the working light.
- Use a long-handled sharp knife to remove the annulus fibrosus, and long-handled nucleus pulposus forceps to remove the diseased disc tissue (Figure 3C).
- Clean the intervertebral space with a scraper and curette to clear the residual disc tissue in the surgical segment.
- After cleaning the intervertebral space, use a spreader to open a collapsed intervertebral space.
- Use a bone rasp to remove the cartilage layer on the surface of the endplate until the bony surface bleeds.
- Place an appropriately sized intervertebral exploration device into the disc. Perform intraoperative X-ray fluoroscopies to determine the appropriate fusion device size (Figure 3D,E).
- After determining the appropriate device size, add allogeneic bone to the interbody cage of the same size and implant the cage under X-ray fluoroscopy (Figure 3F,G).
- After placing the interbody cage, suture the wound layer by layer. Use No. 10, No. 4, and No. 1 thread to suture the muscle, fascia, and surgical incision, respectively (Figure 3H). Compress the surgical incision with gauze.
- Prescribe an anti-inflammatory (cefazolin) once a day for 3 days to prevent infection after the patient returns to the ward. Use antithrombotic drugs (low-molecular weight heparin sodium) to prevent deep vein thrombosis of the lower limbs on the 2nd postoperative day, once a day for 3 days.
4. Postoperative care
- Instruct the patient to rest in bed. Perform deep vein color Doppler on the third postoperative day.
- Instruct the patient to walk on the ground with the assistance of a lumbar brace, usually within 3 days post-operation if the deep vein color Doppler shows no deep vein thrombosis in the lower extremities.
- Change the antithrombotic medication to twice daily if an intramuscular vein thrombosis is present on a deep vein ultrasound of the lower extremities.
- Contact Vascular Surgery for treatment if the deep vein ultrasound of the lower extremities shows a deep vein thrombosis. Perform the lower-extremity rehabilitation exercise as reported previously19,20.
Results
Studies from other groups have shown that, compared to other methods, OLIF surgery has the advantages of a shorter operative time and less intraoperative blood loss (Table 1). Importantly, patients who undergo OLIF surgery recover faster than the commonly used TLIF surgery group12,21,22. Our research group has monitored 42 patients with degenerative lumbar spondylolisthesis (DLS) undergoing OLIF surgery for more than 1 year. The results have shown improvements in visual analog scale (VAS) scores in patients with DLS treated with OLIF compared to preoperative VAS scores, and significant improvements in ventral and dorsal disc heights in OLIF patients as well as segmental lordotic angle and lumbar lordotic angle compared with preoperative outcomes16 (Figure 4). Similar to results published from previous groups, the intervertebral disc height and the intervertebral foramen height of the patients in the OLIF group were higher than those in the TLIF group12,21.
In a previous study of 56 patients who underwent OLIF, one patient developed a psoas major abscess and intervertebral space infection, and one patient developed cage subsidence at the end follow-up16. In a study by Hung et al., 5 of 21 patients treated with OLIF developed cage subsidence22. Sheng treated 38 patients with OLIF and found that two patients had postoperative hip flexion weakness and one patient had postoperative sensory disturbance, but both resolved within 6 months21. In a study by Li et al, where 35 patients were treated with OLIF, one patient had postoperative ileus and one patient had postoperative thigh and numbness, but these symptoms resolved within a short time12.

Figure 1: Selection of the patient's surgical stage and positioning. (A) Preoperative X-ray positioning. (B) The localizer is used to estimate the skin projection point before surgery. Please click here to view a larger version of this figure.

Figure 2: Intraoperative blunt dissection of abdominal muscles to expose the target intervertebral disc. (A,B) Images show the surgeon dissecting the muscle bluntly with the fingers. Please click here to view a larger version of this figure.
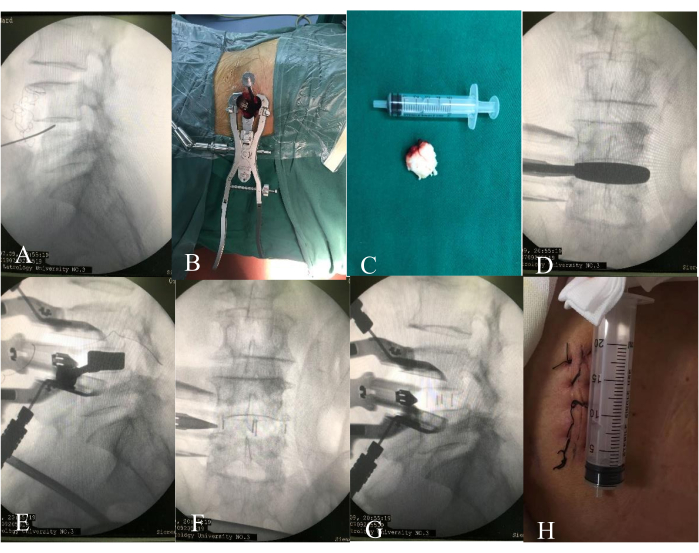
Figure 3: OLIF intraoperative procedures. (A) Intraoperative fluoroscopy to clarify the surgical segment. (B) Working channel. (C) Removal of the target intervertebral disc. (D,E) Intraoperative lumbar vertebrae fluoroscopy to clarify the size of the cage. (F,G) X-ray examination after interbody cage placement. (H) Suture surgical incision. Please click here to view a larger version of this figure.
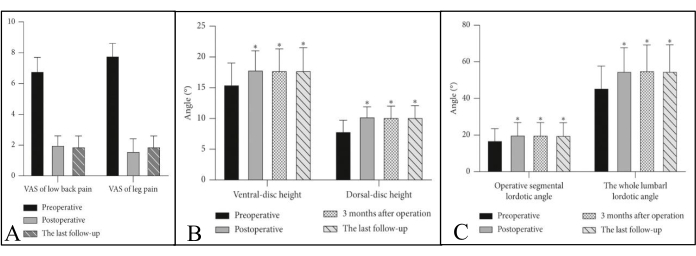
Figure 4: Representative results from a previous study of 42 patients with OLIF. (A) Patients with OLIF had improved postoperative VAS scores compared to preoperative. Lower back pain decreased immediately after OLIF. Compared with preoperative, the postoperative VAS significantly scores decreased (p < 0.05). The visual analog scale (VAS) ranges from 0 to 10, with 0 being no pain and 10 being the most severe pain. (B,C) The postoperative imaging results of OLIF patients were significantly improved compared with before surgery. (B) The mean postoperative ventral disc height and dorsal disc height increased significantly compared with preoperative (p < 0.05). (C) A significant postoperative increase was also observed in the mean operative segmental lordotic angle and the whole lumbar lordotic angle (p < 0.05). Radiological and clinical parameters were all compared using the independent-sample t-test. p < 0.05 was considered statistically significant. This figure has been modified from Huo et al.16. Please click here to view a larger version of this figure.
| Ref. | Surgery technique | Operation time (min) | Blood loss (mL) | Disc height (mm) | Hospital stay (days) | ||||
| 12 | OLIF/TLIF | 186.44 ± 36.5/ 199 ± 59.64 (p>0.05) | 55.94 ± 57.37/ 190 ± 66.33 (p<0.05) | 12.45 ± 1.91/ 10.58 ± 1.26 (p<0.05) | 7.06 ± 2.51/ 12.87 ± 2.60 (p<0.05) | ||||
| 21 | OLIF/MIS-TLIF | 90.79 ± 7.93/100.2 ± 14.95 (p<0.05) | 63.95 ± 23.31/186.36 ± 80.19 (p<0.05) | 0.31 ± 0.57/0.13 ± 0.27 (p<0.05)* | 5.21 ± 1.26/7.22 ± 1.58 (p<0.05) | ||||
| 22 | OLIF/MIS-TLIF | 93.95 ± 14.84/136.38 ± 31.18 (p<0.05) | 90.48 ± 19.74/167.32 ± 35.93 (p<0.05) | 10.52 ± 1.4/10.37 ± 1.11 (p>0.05) | 4.05 ± 1.56/6.39 ± 1.41 (p<0.05) | ||||
| * indicates disc height changes before and after surgery. | |||||||||
Table 1: Comparison of OLIF and TLIF treatment effects.
Discussion
Since formally introduced by Silvestre in 201223, OLIF has gradually attracted the attention of spine surgeons due to the various advantages over other methods used in treating lumbar spine diseases6,12,13,16,21,22. OLIF significantly improved patients' disc height and lordotic angle, which may be due to the more complete clearance of the diseased disc and the larger intervertebral fusion placement compared to the traditional posterior surgery, which facilitated the restoration of the physiological curvature of the spine12,16,21. Long-term postoperative follow-up of OLIF patients showed no significant difference in clinical symptom relief compared to posterior TLIF surgery, but significantly reduced operative time and intraoperative bleeding in patients6. Furthermore, OLIF can be used as a potential approach to treat lumbar infectious diseases, as this method can thoroughly remove lesions and achieve good therapeutic effects24,25. As a minimally invasive interbody fusion, OLIF causes less intraoperative trauma to patients and significantly relieves symptoms. Hence, OLIF can be considered a safer alternative to other surgical techniques. Nonetheless, despite the numerous advantages of OLIF, a full understanding of OLIF-related risks and additional care, which are critical to the surgery success, are highlighted below.
First, the selection criteria of patients should be reviewed carefully. For patients with a history of abdominal surgery, abdominal scar tissues can increase the complexity of performing another surgery. Hence, adequate preoperative examination is highly recommended. Preoperative MRI examination can determine the size of the OLIF working corridor, as a smaller corridor would increase the difficulty of surgery and affect the prognosis of patients26,27. Our study confirmed that when the anterior edge of the left psoas muscle exceeds the anterior edge of the surgical segment, it increases the risk of lumbar plexus injury (LPI) associated with OLIF surgery27. It has also been suggested that a gap width less than 1 cm between the psoas muscle and the anterior vertebral artery is not suitable for OLIF28. Preoperative abdominal vascular examination can determine whether there is variation in the abdominal great vessels18, as well as the blood vessels of the patient's vertebral body segments, which can provide a reference for selecting appropriate size of the interbody cage used in OLIF.
Another important category is patients with obesity. The accumulation of abdominal fat in obese patients may affect the surgical field of vision. Compared with the traditional posterior approach, OLIF places greater demands on the surgical skills of surgeons. In a study of 238 patients undergoing OLIF surgeries, obese patients with OLIF at stage L5-S1 required a longer operative time than non-obese patients (273.75 ± 90.07 min vs. 223.55 ± 57.93 min), and the complication rate of surgical approach-related sequelae in obese patients was higher than that in non-obese patients29. Therefore, surgeons should fully understand the related risks for obese patients and strengthen the nursing care for these patients following OLIF surgery. Our study has shown that systematic postoperative lower extremity exercise can promote the recovery of patients after OLIF surgery30. Thus, we think lower-limb exercises may benefit patients with obesity after OLIF surgery.
On that note, special care for all patients requiring surgery at the L5-S1 level should be considered. This is advised because the L5-S1 level is affected by the iliac vessels and iliac crest, so it is challenging for some spine surgeons to perform OLIF at L5-S1. The risk of vascular injury in L5-S1 is higher in OLIF than that in ALIF31. In recent years, with the development of related techniques and the invention of special traction devices, OLIF surgery in the L5-S1 level has been gradually increasing32.
Separately, during OLIF surgery, surgeons should minimize the duration of surgery and reduce traction on the psoas muscles. This is due to the fact that patients undergoing OLIF have a certain likelihood of experiencing intraoperative dural tear, symptoms of dysuria, numbness in the front of the thigh, and retrograde ejaculation after surgery33. Because OLIF surgery goes through the abdomen, some patients may experience postoperative abdominal distension due to intraoperative pulling of the intestinal canal. Therefore, OLIF surgery should be performed in a cautious manner to reduce damage to the blood vessels, nerves, related tissues, and to achieve better surgical effects.
Patients with stand-alone OLIF may have a certain probability of cage sedimentation. Previous studies have shown that the occurrence of cage sedimentation ranges from 2.9% to 10%34,35. In addition, due to postmenopausal osteoporosis, some elderly female patients have poor interbody fusion ability, and the interbody cage in some patients may not fuse or even shift in the intervertebral space25. Hence, OLIF surgery-assisted posterior percutaneous screw placement is needed in such cases. This post-OLIF surgical approach can improve the interbody fusion rate, decrease the pressure of the interbody cage on the upper and lower endplates, and reduce complications associated with non-fusion36,37.
It is worth noting that due to the right decubitus position for OLIF patients, accurate disc positioning is required. Compared with the prone position, OLIF patients have greater spinal flexibility. The patient's target disc needs to be precisely located during OLIF surgery. In addition, the interbody cage inserted during OLIF surgery is larger, and thus multiple fluoroscopies are needed to adjust and optimize the position of the cage to achieve better radiological outcomes38. Although the development of intraoperative 3D navigation techniques can assist surgeons in careful positioning of the interbody cage, the consequence of radiation exposure from intraoperative imaging in OLIF patients still requires further study30.
It is worth noting that, in addition to the advantages and the considerations we need to take into account above, OLIF surgery also has disadvantages. To start with, compared with the traditional posterior approach, there is a tendency to damage abdominal blood vessels, the lumbar plexus, and other structures during OLIF surgery. In addition, as a minimally invasive surgery, the surgical field of OLIF is more limited than that of posterior surgery. Therefore, it is necessary to maintain a good surgical field during the operation for the smooth progress of OLIF surgery. However, stand-alone OLIF has a higher incidence of cage subsidence compared to posterior screw-assisted fixation of OLIF, and this is an important factor in postoperative revision.
Disclosures
The authors declare that there are no conflicts of interest in this study.
Acknowledgements
None.
Materials
| Name | Company | Catalog Number | Comments |
| Bipolar electrocoagulation tweezers | Juan'en Medical Devices Co.Ltd | BZN-Q-B-S | 1.2 x 190 mm |
| Bone rasp | DePuy Synthes | 03.809.849 | 35 x 8 mm |
| Cefazolin | Cspc Pharmaceutical Group Limited | 1.0 g | |
| Computed Tomography | PHILIPS | ||
| Curette | Qingniu | 20739.01 | 300 x Ø9 x 5° |
| Curette | DePuy Synthes | 03.809.873 | 6 mm |
| Dilation tubes | DePuy Synthes | 03.809.913 | 140 mm |
| High frequency active electrodes | ZhongBangTianCheng | GD-BZ | GD-BZ-J1 |
| Interbody cage | DePuy Synthes | 08.809.273S | 55 x 22 x 13 mm |
| Intervertebral exploration device | DePuy Synthes | 03.809.233 | 13 mm |
| Kirschner wire | Qingniu | ||
| Lighting cable | DePuy Synthes | 03.612.031 | |
| Lighting sheet | DePuy Synthes | 03.809.925S | |
| Low Molecular Weight Heparin Sodium Injection | Cspc Pharmaceutical Group Limited | 0.4 mL | |
| MRI | PHILIPS | ||
| Scraper | DePuy Synthes | 03.809.833 | 13 mm |
| Spreader | DePuy Synthes | 03.809.877 | 50 x 13 mm |
| Surgical film | 3L | SP4530 | 45 x 30 cm |
| Ultrasound Color Doppler | PHILIPS | ||
| Universal arm | DePuy Synthes | 03.809.941 | |
| Universal arm operating table clips | DePuy Synthes | 03.809.942 | |
| X-ray machine | GE healthcare |
References
- Ravindra, V. M., et al. Degenerative lumbar spine disease: estimating global incidence and worldwide volume. Global Spine Journal. 8 (8), 784-794 (2018).
- Wang, H., et al. 17β-Estradiol alleviates intervertebral disc degeneration by inhibiting NF-κB signal pathway. Life Science. 284, 119874 (2021).
- Yang, S., Zhang, F., Ma, J., Ding, W. Intervertebral disc ageing and degeneration: The antiapoptotic effect of oestrogen. Ageing Research Reviews. 57, 100978 (2020).
- Patel, D. V., Yoo, J. S., Karmarkar, S. S., Lamoutte, E. H., Singh, K. Interbody options in lumbar fusion. Journal of Spine Surgery. 5, S19-S24 (2019).
- Xu, D. S., et al. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Annals of Translational Medicine. 6 (6), 104 (2018).
- Kim, W. K., Son, S., Lee, S. G., Jung, J. M., Yoom, B. R. Comparison of lateral interbody fusion and posterior interbody fusion for discogenic low back pain. Turkish Neurosurgery. 32 (5), 745-755 (2022).
- Li, J., et al. Efficacy and safety of a modified lateral lumbar interbody fusion in L4-5 lumbar degenerative diseases compared with traditional XLIF and OLIF: a retrospective cohort study of 156 cases. BMC Musculoskeletal Disorders. 23 (1), 217 (2022).
- Chung, H. W., Lee, H. D., Jeon, C. H., Chung, N. S. Comparison of surgical outcomes between oblique lateral interbody fusion (OLIF) and anterior lumbar interbody fusion (ALIF). Clinical Neurology and Neurosurgery. 209, 106901 (2021).
- Kang, G. H., et al. Surgical treatment for degenerative lumbar disease with neurologic deficits: comparison between oblique lumbar interbody fusion and posterior lumbar interbody fusion. Korean Journal of Neurotrauma. 18 (2), 277-286 (2022).
- Hu, Z. -. J., et al. Effect of pure muscle retraction on multifidus injury and atrophy after posterior lumbar spine surgery with 24 weeks observation in a rabbit model. European Spine Journal. 26 (1), 210-220 (2015).
- Kawaguchi, Y., Matsui, H., Tsuji, H. Back muscle injury after posterior lumbar spine surgery. Part 2: Histologic and histochemical analyses in humans. Spine. 19 (22), 2598-2602 (1994).
- Li, R., Shao, X., Li, X., Liu, Y., Jiang, W. Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: Minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine. 100 (3), e23783 (2021).
- Du, X., et al. Oblique lateral interbody fusion versus transforaminal lumbar interbody fusion in degenerative lumbar spondylolisthesis: a single-center retrospective comparative study. BioMed Research International. 2021, 6693446 (2021).
- Champagne, P. O., et al. Sagittal balance correction following lumbar interbody fusion: a comparison of the three approaches. Asian Spine Journal. 13 (3), 450-458 (2019).
- Mun, H. Y., Ko, M. J., Kim, Y. B., Park, S. W. Usefulness of oblique lateral interbody fusion at L5-S1 level compared to transforaminal lumbar interbody fusion. Journal of Korean Neurosurgical Society. 63 (6), 723-729 (2020).
- Huo, Y., et al. Oblique lumbar interbody fusion with stand-alone cages for the treatment of degenerative lumbar spondylolisthesis: a retrospective study with 1-year follow-up. Pain Research and Management. 2020, 9016219 (2020).
- Buckland, A. J., et al. Anterior column reconstruction of the lumbar spine in the lateral decubitus position: anatomical and patient-related considerations for ALIF, anterior-to-psoas, and transpsoas LLIF approaches. European Spine Journal. 31 (9), 2175-2187 (2022).
- Berry, C. A. Oblique lumbar interbody fusion in patient with persistent left-sided inferior vena cava: case report and review of literature. World Neurosurgery. 132, 58-62 (2019).
- Liu, S. K., et al. The effect of systematic lower-limb rehabilitation training in elderly patients undergoing lumbar fusion surgery: a retrospective study. Oncotarget. 8 (68), 112720-112726 (2017).
- Yang, S. D., et al. The effect of lower limb rehabilitation gymnastics on postoperative rehabilitation in elderly patients with femoral shaft fracture: A retrospective case-control study. Medicine. 95 (33), e4548 (2016).
- Sheng, S. -. R., et al. Minimally invasive surgery for degenerative spondylolisthesis: transforaminal or oblique lumbar interbody fusion. Journal of Comparative Effectiveness Research. 9 (1), 45-51 (2020).
- Hung, S. F., et al. Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Scientific Reports. 11 (1), 12783 (2021).
- Silvestre, C., Mac-Thiong, J. M., Hilmi, R., Roussouly, P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine Journal. 6 (2), 89-97 (2012).
- Fan, W., et al. One-stage freehand minimally invasive pedicle screw fixation combined with mini-access surgery through OLIF approach for the treatment of lumbar tuberculosis. Journal of Orthopaedic Surgery and Research. 17 (1), 242 (2022).
- Du, X., et al. Evaluation of the efficacy of OLIF combined posterior internal fixation for single-segment lumbar tuberculosis: a single-center retrospective cohort study. BMC Surgery. 22 (1), 54 (2022).
- Boghani, Z., et al. Variability in the size of the retroperitoneal oblique corridor: A magnetic resonance imaging-based analysis. Surgical Neurology International. 11, 54 (2020).
- Huo, Y., et al. Incidence and risk factors of lumbar plexus injury in patients undergoing oblique lumbar interbody fusion surgery. European Spine Journal. 32 (1), 336-344 (2023).
- Molinares, D. M., Davis, T. T., Fung, D. A. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs: an MRI study. Journal of Neurosurgery: Spine. 24 (2), 248-255 (2016).
- Xi, Z., et al. The effect of obesity on perioperative morbidity in oblique lumbar interbody fusion. Journal of Neurosurgery: Spine. , 1-8 (2020).
- Wang, H., et al. Clinical rehabilitation effect of postoperative lower-limb training on the patients undergoing OLIF surgery: a retrospective study. Pain Research and Management. 2010, 1065202 (2020).
- Chung, N. S., Jeon, C. H., Lee, H. D., Kweon, H. J. Preoperative evaluation of left common iliac vein in oblique lateral interbody fusion at L5-S1. European Spine Journal. 26 (11), 2797-2803 (2017).
- Orita, S., et al. Technical and conceptual review on the L5-S1 oblique lateral interbody fusion surgery (OLIF51). Spine Surgery and Related Research. 5 (1), 1-9 (2021).
- Hah, R., Kang, H. P. Lateral and oblique lumbar interbody fusion-current concepts and a review of recent literature. Current Reviews in Musculoskeletal Medicine. 12 (3), 305-310 (2019).
- Woods, K. R. M., Billys, J. B., Hynes, R. A. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. The Spine Journal. 17 (4), 545-553 (2017).
- Ohtori, S., et al. Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine Journal. 9 (4), 565-572 (2015).
- Wang, Z., et al. Biomechanical evaluation of stand-alone oblique lateral lumbar interbody fusion under 3 different bone mineral density conditions: a finite element analysis. World Neurosurgery. 155, e285-e293 (2021).
- Fang, G., et al. Biomechanical comparison of stand-alone and bilateral pedicle screw fixation for oblique lumbar interbody fusion surgery-a finite element analysis. World Neurosurgery. 141, e204-e212 (2020).
- Ko, M. J., Park, S. W., Kim, Y. B. Effect of cage in radiological differences between direct and oblique lateral interbody fusion techniques. Journal of Korean Neurosurgical Society. 62 (4), 432-441 (2019).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved