Method Article
Surgically Induced Cardiac Volume Overload by Aortic Regurgitation in Mouse
* These authors contributed equally
In This Article
Summary
This protocol presents a practical guide on the surgery for creation of aortic regurgitation (AR) in the mouse. Assessment of the AR mouse by echocardiography and invasive hemodynamic measurement recapitulates its clinically relevant characteristics of volume overload-induced eccentric hypertrophy, suggesting its promising application in the study of cardiac hypertrophy.
Abstract
Aortic regurgitation (AR) is a common valvular heart disease that exerts volume overload on the heart and represents a global public health problem. Although mice are widely applied to shed light on the mechanisms of cardiovascular disease, mouse models of AR, especially those induced by surgery, are still paucity. Here, a mouse model of AR was described in detail which is surgically induced by disruption of the aortic valves under high-resolution echocardiography. In accordance with regurgitated blood flow, AR mouse hearts present a distinctive and clinically relevant volume overload phenotype, which is characterized by eccentric hypertrophy and cardiac dysfunction, as evidenced by echocardiographic and invasive hemodynamic evaluation. Our proposal, in a reliable and reproducible manner, provides a practical guide on the establishment and assessment of a mouse model of AR for future studies on molecular mechanisms and therapeutic targets of volume overload cardiomyopathy.
Introduction
In the presence of increased volume overload (preload) or pressure overload (afterload), the heart undergoes enlargement, a condition termed hypertrophy. Although cardiac hypertrophy is a compensatory response to maintain perfusion of peripheral organs before cardiac failure, it is also an independent risk factor for major cardiovascular events1,2. Volume overload is one of the important manifestations of increased mechanical stress. Volume overload occurs during cardiac diastole and induces eccentric cardiac hypertrophy, which is not only commonly seen in valvular diseases, such as aortic regurgitation and mitral regurgitation, but also in end-stage hypertensive heart disease, myocardial infarction, dilated cardiomyopathy, and excessive exercise. In addition, in clinical practice, some drugs that can better reduce the myocardial hypertrophy induced by pressure overload have unsatisfactory effects in the treatment of myocardial hypertrophy induced by volume overload1. It is therefore of great significance to discover the mechanism and intervention methods of eccentric cardiac remodeling caused by volume overload. However, such research on volume overload has been significantly hampered for a long time, which can be, in large part, attributed to the lack of small animal models that can be easily operated, efficiently quantified, and stably replicated3.
As for small animal species, mice have become the mainstream model animal for cardiovascular disease research due to their short life cycle, convenient operation, clear genome, and ease of genetic modification4. In terms of model categories, compared to genetic modification models and drug-treated models, surgical models have obvious unique advantages. The surgical model can avoid excessive and laborious mouse breeding and gene identification that are necessary for the genetic modification model and can also avoid the non-specific effects on extracardiac tissues and organs that are difficult to control in drug-treated models. The mouse model of aortocaval shunt has been documented to induce cardiac volume overload in previous literature5. However, aortocaval shunt accounts for a small fraction of cardiac eccentric hypertrophy in the clinic and causes biventricular overload5, making it of little translational significance to be used in left ventricular eccentrical hypertrophy study. Nevertheless, valvular heart disease represents a major public health problem worldwide; it is estimated that around 15% of the population >75 years of age has significant valvular disorder6. Although aortic regurgitation (AR) occupies a portion of valvular heart disease, it distinctively causes eccentric left ventricular (LV) hypertrophy due to an increase in volume overload by regurgitant blood flow7,8. Considering the right common carotid artery (RCCA) provides a route to reach the location of aortic valves, it is conceptually intriguing to disrupt aortic valves via the RCCA to cause regurgitant blood flow in mice. Inspired by the techniques of creating oscillating aortic flow9, a mouse model of aortic regurgitation (AR) was recently established in our lab to surgically induce volume overload7. This AR mouse demonstrates obvious LV eccentric hypertrophy, which is a clinically transformative approach and demonstrates a great translational potential for studying the overloaded heart phenotype and its underlying mechanism. Here, a detailed step-by-step procedure was described to perform AR surgery in mice, recapitulated by high frequency echocardiography and invasive hemodynamics to ensure the success of the surgery (Figure 1).
Protocol
This protocol has received ethical approval from the Animal Care and Use Committee of Zhongshan Hospital, Fudan University, and follows the recommendations of Guide for the Care and Use of Laboratory Animals (No. 85-23, revised 2011; National Institutes of Health, Bethesda, MD, USA).
NOTE: Animal experiments were performed on male C57BL/6J mice >10 weeks of age. The surgeon in this protocol should be skillful in the manipulation of murine echocardiography, before he/she performs the AR operation in the mouse. However, at most research institutions, small rodent echocardiography is operated by a core facility, so the surgeon can closely collaborate with core experts, if not an experienced surgeon in echocardiography. Experience of invasive hemodynamic measure in mouse is a plus.
1. Preparation for ultrasound imaging (mandatory) and invasive hemodynamic measurement (optional)
- Start up the ultrasound machine connected to a 30 MHz probe. Set the temperature-controlled ultrasound animal platform in the position for the aortic arch view, in which the right side of the mouse is tilted up.
NOTE: It is recommended that the cranial end of the ultrasound animal platform is placed toward the surgeon. However, whether the cranial end or the caudal end is toward the surgeon should be dependent upon on which one the surgeon feels more comfortable with. - Connect a micromanometer (pressure catheter) to the data acquisition device and analog/digital converter. Immerse the micromanometer's calibration cuvette in saline for saline calibration.
NOTE: If the condition permits, a pressure-volume catheter can be used as well. We use a pressure catheter because the pressure data acquisition device in the lab collects pressure-only data and does not have the capacity to collect volume-related data, although the echocardiographic results in the current study can also delineate LV volumes.
2. Anesthesia of mice, preparation of surgical devices, and isolation of the RCCA
NOTE: Surgical tools must be sterilized and autoclaved before use. All steps are recommended to be performed under aseptic conditions. It is also recommended that hair removal is performed 1 day ahead to save time during the imaging procedure, minimize potential undesired stress responses in the mice, and to keep the chest and extremities clean and dry.
- Anesthetize the mouse in the induction chamber, which is connected to a vaporizer set to 4% isoflurane mixed with 0.8 L/min of oxygen. When the mouse falls asleep or the tail pinch reflex disappears, remove the animal from the induction chamber.
- Place the animal in the supine position on a copper plate, which is warmed by a heating pad. Connect its nose to a nosecone, to which 1.5% isoflurane mixed with 0.8 L/min of oxygen is delivered for maintaining a steady level of anesthesia.
NOTE: A copper plate is recommended as it is convenient to clean and is rust proof, though it can be replaced by another type of metal plate. - Place ophthalmic ointment on the eyes to prevent dryness under anesthesia and tape the extremities onto the copper plate. Remove hair from the neck and chest using depilatory cream and clean the depilated area with 75% ethanol.
- Prepare the necessary surgical tools, including various forceps and scissors (Figure 2A; see Table of Materials).
- Make a longitudinal median incision, around 1 cm, in the neck with curved thumb forceps and straight scissors, between the lower jaw and sternum.
- Bluntly dissect the left and right part of the thyroid gland using two pairs of forceps. With the curved fine thumb forceps, separate the stemohyoideus muscle and fat tissue in the right paratracheal region to expose the RCCA for as long as possible. Avoid injury of the vagal nerve at all times, as this can cause hypotension, bradycardia, and death (Figure 2B).
3. Catheterization through the RCCA and ascending aorta under ultrasound guidance
- Pass two 6-0 silk threads, around 5 cm each, under the vessel. Ligate the distal RCCA with a tight knot using one thread and fix the two ends of the tight knot next to the head of the animal to maintain light tension on the RCCA. This action will facilitate the catheterization in the coming steps.
- Place a loose knot on the proximal RCCA using the second thread. This fills the sealed region of the RCCA with blood, making it easy to incise.
- Use small pinch scissors to cut a wedge-shaped opening, 1-2 mm proximal to the tight knot, to open the RCCA. Make sure the size of the incision is neither too small to insert a catheter, nor too large for it to snap during insertion.
NOTE: Incision under a microscope is highly recommended. Puncturing a small hole in the vessel with a 26 G needle is an alternative method. - Prepare a plastic catheter containing a metal wire (Figure 2C). Stretch the incision with long-handed curved tying forceps, insert the plastic catheter containing the metal wire into the RCCA, and move forward to the loose knot.
- Relieve the loose knot to advance the catheter and wire around 2 cm. Transfer the copper plate containing the animal onto the ultrasound animal platform, apply ultrasound gel to the mouse neck and chest, and then carefully forward the catheter and wire through the RCCA and ascending aorta under ultrasound guidance.
4. Puncture of the aortic valves under ultrasound guidance
- Collect basal ultrasound data in color Doppler mode and pulse wave Doppler mode before the plastic catheter and metal wire reach the aortic orifice.
- With the ultrasound simultaneously and clearly showing the ascending aorta, the LV outflow tract, the catheter, and the wire, when the catheter and wire reach the aortic orifice, protrude the tip of the wire from the catheter, and puncture the aortic valves (Figure 1).
NOTE: When the aortic valve is perforated, the surgeon should be able to sense this break. - Slightly retreat the catheter and wire from the aortic orifice and collect post-perforation ultrasound data in color Doppler mode and pulse wave Doppler mode after puncture of the aortic valves. The regurgitant flow is red in color during cardiac diastole in color Doppler mode and can be quantitively confirmed in pulse wave Doppler mode.
- Consider a peak diastolic velocity of aortic flow (PSVa) between 300-500 mm/s as satisfactory. If the regurgitant degree of blood flow is unsatisfactory, repeat step 4.2.
- Optional: Apply a micromanometer before and instantly after perforation of the aortic valves to further confirm the existence of regurgitant flow. To check, both the aortic end-diastolic pressure (AEDP) is depressed, and the aortic pulse pressure is enhanced by around 20 mmHg.
NOTE: A detailed description of how to use a micromanometer catheter to perform invasive LV hemodynamic measurement has been elegantly presented elsewhere10,11.
5. Withdrawal of the plastic catheter and metal wire, and perioperative care
- Remove the ultrasound gel and dry the mouse with sterile gauze or tissue after confirmation of successful perforation of the aortic valves, then carefully withdraw the plastic catheter with the central metal wire, before ligation of the RCCA.
- Close the skin using a 5-0 silk suture in a continuous suture pattern and apply povidone-iodine solution to the suture site. Administer the mouse with meloxicam (0.13 mg) subcutaneously for analgesia and place the mouse in a pre-warmed cage under a warming light until fully awake for recovery.
6. Sham surgery
- Perform sections 1-3 as described. For the sham-operated mouse, perform similar procedures as in section 4 without disruption of the aortic valves.
- Perform section 5 as described, although AR should not be present in any of the sham-operated mice.
7. Assessment of aortic valve perforation, cardiac morphology, and function using echocardiography and invasive hemodynamic measurement
- After 4 weeks of AR, use echocardiographic B-mode, color Doppler mode, and pulse wave Doppler mode to assess blood flow of the aortic arch in the aortic arch view, and measure PDVa, according to step 4.1 and elsewhere1,12.
- Use echocardiographic B-mode and M-mode to assess LV dimension and contractility in the parasternal long axis view, with the LV end-diastolic (LVEDD) and end-systolic (LVESD) dimensions, LV posterior wall end-diastolic (LVPWTd) and end-systolic (LVPWTs) thickness, LV ejection fraction (LVEF), and fractional shortening (LVFS) derived.
NOTE: A detailed description of how to use the ultrasound machine and manipulation of ultrasound views has been elegantly described previously12. - After the echocardiographic imaging, perform invasive hemodynamic measurement, in a manner similar to step 4.3 and elsewhere10. Record the maximal contraction and relaxation velocity (+dp/dt and −dp/dt). Insert the micromanometer into the left common carotid artery (LCCA, not RCCA), since the RCCA was permanently ligated during the AR surgery.
- After the invasive hemodynamic measurement, euthanize the mouse via cervical dislocation. Open the chest, flush the heart with 10% formalin, followed by 0.9% sodium chloride solution, excise the heart by cutting off the aorta, and section transversely at the level of the inferior margin of the left auricle. Acquire images using light microscopy.
Results
To guarantee successful AR, we validated regurgitant blood flow using color Doppler and pulse wave Doppler echocardiography. In mice with AR, the color Doppler spectrum of the aortic arch showed regurgitant flow (red) immediately post-operation, which was absent in sham mice (no flow in diastole; Figure 3A). Consistently, the pulse wave Doppler demonstrated robustly elevated regurgitant flow in AR mice (Figure 3B,C). With a further confirmation using invasive hemodynamic measurement, it was evident that AEDP was noticeably lower and pulse pressure (PP) was resultantly promoted in AR mice relative to that of sham animals (Figure 3D-F). The mortality in the peri-operative period, within 2 h after surgery, is around 15%, and the mortality in the post-operative period of 4 weeks is around 20% (peri-operative mortality was excluded; Figure 4A). Macroscopic photographs of the LV outflow tract indicate perforated aortic valves in AR mice and intact valves in sham mice (Figure 4B). These results indicate that the murine AR model was successfully established.
The efficacy of AR and its resulting remodeling was further validated by echocardiography and hemodynamic measurement 4 weeks after surgery. AR induced prominent enlargement of the LV cavity was evidenced by the strikingly increased LVEDD and LVESD, along with slightly elevated LVPWTd (Figure 4A-C). On the contrary, AR caused a reduction in LVEF and LVFS (Figure 4A-C). In agreement with the results derived from echocardiography, invasive hemodynamic measurement also demonstrated impaired cardiac function, as evidenced by a remarkable reduction in +dp/dt and -dp/dt (Figure 4D,E). Therefore, the AR hearts underwent LV eccentric hypertrophy and dysfunction over 4 weeks post-surgery.
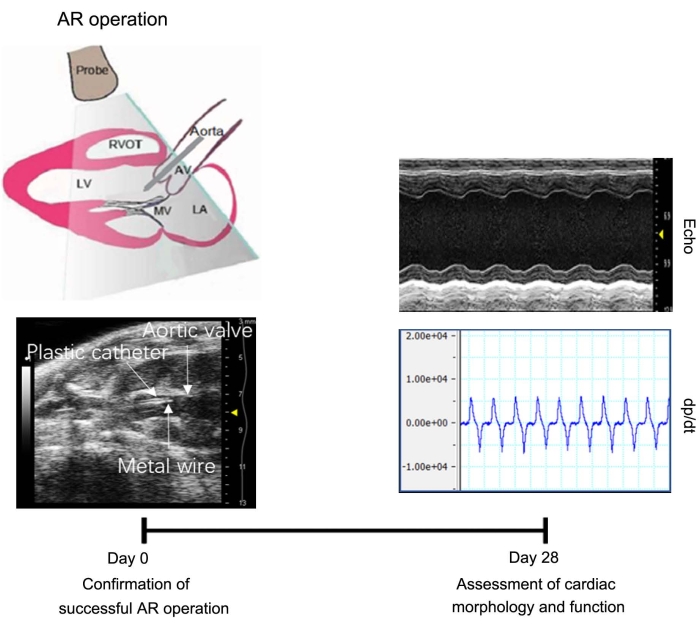
Figure 1: Schematic timeline of the experimental design. AR is created by puncture of the aortic valves and confirmed by echocardiography and invasive hemodynamic measurement. After 4 weeks of operation, cardiac morphology and function are evaluated by echocardiography and invasive hemodynamic measurement. Abbreviations: AR = aortic regurgitation, AV = aortic valve, LA = left atrium, LV = left ventricle, MV = mitral valve, RVOT = right ventricular outflow tract. Please click here to view a larger version of this figure.

Figure 2: Manipulation of the RCCA. (A) Surgical tools. Scale unit in cm. (B) Separation of the RCCA from the vagal nerve. (C) Plastic catheter and metal wire used to insert into the subsequent RCCA opening. Scale bar = 1 cm. Abbreviations: RCCA = right common carotid artery. Please click here to view a larger version of this figure.
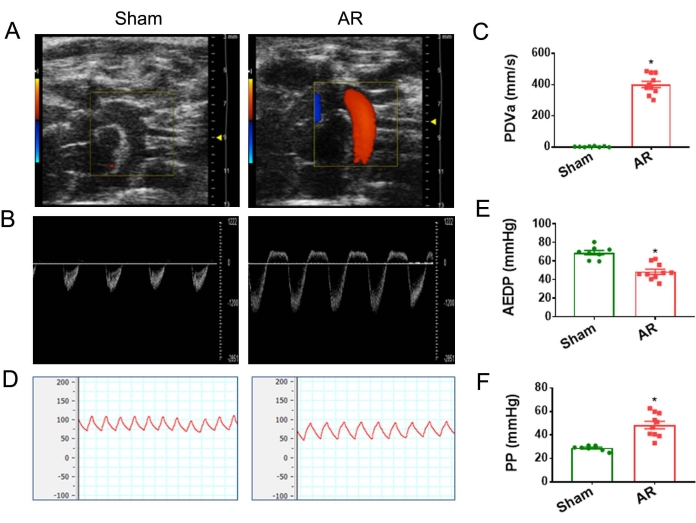
Figure 3. Confirmation of successful AR operation in mice. (A) Immediately after perforation of the aortic valves, color Doppler images of aortic arch flow show regurgitant flow (red) during cardiac diastole in AR mice, which is absent in sham mice. (B) Pulsed wave Doppler recordings of aortic arch flow demonstrate strikingly elevated regurgitant flow in AR mice. (C) Quantitative analysis of PDVa. (D) Invasive hemodynamic recordings demonstrate lower AEDP in AR mice. (E) Quantitative analysis of AEDP. (F) Quantitative analysis of PP. Abbreviations: AEDP = aortic end-diastolic pressure, PDVa = peak diastolic velocity of aortic flow, PP = pulse pressure. * P < 0.05 versus sham. Data are presented as mean ± SEM. Student's t-test is used to determine statistical significance. Please click here to view a larger version of this figure.
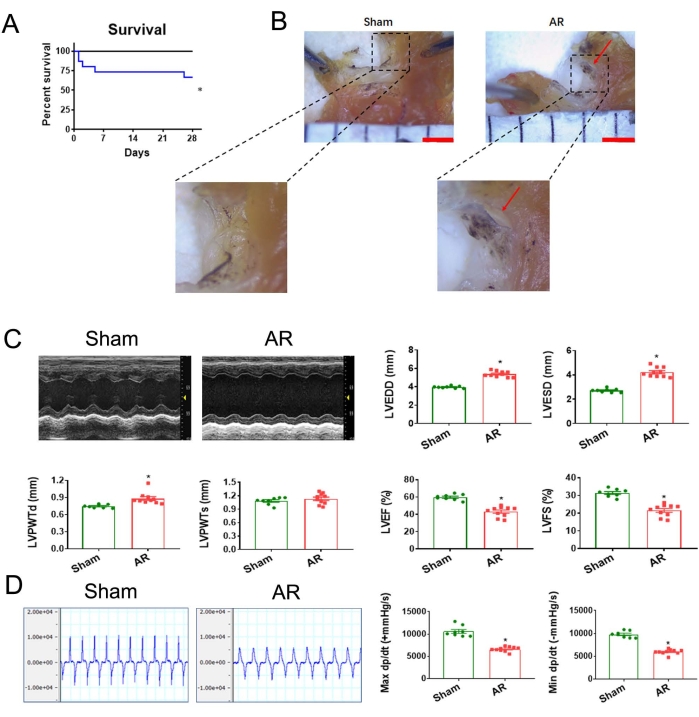
Figure 4: Assessment of survival curve, valve perforation, cardiac morphology, and function 4 weeks after AR. (A) Survival curves in AR model. Kaplan-Meier survival analysis was performed in mice subjected to AR or the corresponding sham operation for 4 weeks. (B) Gross appearance of aortic valve lesions. Scale bar = 1 mm. The red arrow shows perforation. (C) Representative M-mode echocardiographic images of sham and AR hearts. Quantitative analysis of LV end-diastolic (LVEDD) and end-systolic (LVESD) dimensions, LV posterior wall end-diastolic (LVPWTd) and end-systolic (LVPWTs) thickness, LV ejection fraction (LVEF), and fractional shortening (LVFS). (D) Representative images of maximal contraction and relaxation velocity (+dp/dt and −dp/dt) derived from invasive hemodynamic measurement. Quantitative analysis of +dp/dt and −dp/dt. Abbreviations: AR = aortic regurgitation. * P < 0.05 versus sham. Data are presented as mean ± SEM. Student's t-test is used to determine statistical significance. Please click here to view a larger version of this figure.
Discussion
The surgical induction of AR in the mouse is a technically challenging, new technique but has significant translational relevance. To master the technique, a surgeon should at least be familiar in advance with murine cervical and cardiac anatomy, mouse handling, and echocardiography. Skillful operation in invasive hemodynamic measurement is a plus. For successful AR operation, special care should be taken on several critical steps.
Cutting open the RCCA is the most crucial step. The hole on the RCCA should not be too small to accommodate the plastic catheter, nor too large to easily break off the RCCA during insertion of the plastic catheter. To satisfactorily cut the RCCA, the small pinch scissors should be slightly opened before cutting the RCCA. Undertaking this step under a microscope is strongly recommended.
Avoid perforation of the RCCA and ascending aorta. It is easy to perforate the vascular wall when the plastic catheter containing a metal wire is introduced via the RCCA and forwarded to the aortic orifice. Perforation of the RCCA and ascending aorta would lead to overt bleeding, and in most cases the animal would die within 1 week post-operation. To address this concern, make sure the headend of the wire does not exceed the opening mouth of the catheter. Further, the catheter containing the wire should be advanced very gently within the vessel. The surgeon should pause advancing when resistance occurs, withdraw a little, and then gently advance again.
One should also avoid perforation of the aortic root and ventricular wall during puncture of aortic valves. It is easy to perforate the aortic root and ventricular wall (septum and posterior wall) when the plastic catheter containing the metal wire is used to puncture the aortic valves. Once perforation occurs, heavy bleeding and hematoma ensues, and in most cases the animal dies within 1 h. To puncture the valves without aortic and ventricular wall perforation, make sure the lumen of the aortic root and the basal left ventricle is clearly and simultaneously visualized, the headend of the wire exceeds the opening mouth of the catheter a little (not too much), and the catheter containing the wire is advanced alongside the long axis of the aorta to puncture the roof aortic valves.
The high-frequency echocardiography used in this protocol provides a real-time and noninvasive tool to assess ongoing cardiovascular structural and functional changes in living animals. Echocardiography is especially helpful for timely visualization of the movement of the plastic catheter and metal wire, as well as for assessment of the degree of regurgitation. Considering the Doppler angle between the sound beam and blood flow direction is positively associated with experimental bias11, we choose the aortic arch for the evaluation of blood flow, as if the sampling volume is placed in this location, the Doppler angle can be easily maintained within 15°. In that setting, if the speed of regurgitant flow is slow, the surgeon could repeat the procedure so that the aortic valves more severely disrupted. Therefore, echocardiography is indispensable for successful establishment of the AR murine model. In this protocol, the blood flow of aortic arch, rather than the site of aortic valves nor ascending aorta, was evaluated by Doppler echocardiography. Additionally, the invasive hemodynamic measurement provides supporting information for its lower AEDP and promoted PP, suggesting that blood flow regurgitates during cardiac diastole.
Volume overload is common in the end-stage of nearly all heart diseases7,13. With the help of echocardiography, the AR mouse model proposed in this protocol can precisely indicate the severity of regurgitation in a real-time manner, thus providing a suitable tool for volume overload study. In this mouse model, the most prominent change is that the left ventricular diameter is significantly increased, indicative of eccentric hypertrophy induced by cardiac volume overload. This AR model is superior over the aortocaval shunt model, as the incidence of aortocaval shunt is low in clinic, and aortocaval shunt could lead to double ventricular volume overload5. This AR surgical model is also more advanced than similar AR models used in previous studies about surgically induced AR and volume overload cardiac hypertrophy14,15. In those reports, a 1.4 French pressure catheter was inserted into the RCCA of the mouse and advanced to damage the aortic valve cusp without echocardiography. However, the pressure catheter is too big relative to the aortic valves, which can easily cause severe regurgitation, leading to high mortality and low success rates. Moreover, without echocardiographic guidance, it's easy to penetrate the RCCA or aorta and cause hemorrhage, in contrast to the safety provided under echocardiographic guidance used in this study. Even so, a drawback of this AR surgical model is that it mimics acute volume overload via valve disruption, while AR in humans mostly is a chronic process which develops after a long period. Thus, it has to be noted, that the results of this AR surgical model may not be simply extrapolated to human parameters and the discrepancy needs to be considered during analysis. Regardless, it is expected that this AR mouse model is of great translational significance to investigate the mechanism and intervention of eccentric cardiac remodeling caused by volume overload. This AR model also provides a favorable opportunity for studies differentiating structural, functional, and signal characteristics of volume overload from that of pressure overload.
Disclosures
The authors have no conflicts of interest to disclose.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81941002, 82170389, 82170255, 81730009, 81670228, and 81500191), Laboratory Animal Science Foundation of Science and Technology Commission of Shanghai Municipality (201409004300 and 21140904400), Health Science and Technology Project of Shanghai Pudong New Area Health Commission (PW2019A-13), and "Rising Sun" Excellent Young Medical Talents Program of Shanghai East Hospital (2019xrrcjh03).
Materials
| Name | Company | Catalog Number | Comments |
| Copper plate | JD.com Inc. | Customized | 20 X 15 cm or bigger is prefeered |
| Curved Tying forceps | 66 Vision Tech | 53324A | to stretch and isolate muscle, tissue, and vessel |
| Heating pad | JD.com Inc. | Changzhi 55 | warm the copper plate and mouse by the way |
| Long-handed Curved Tying Forceps | MECHENIC | TS-15 | to stretch vessel |
| Metal Wire (stainless steel) | JD.com Inc. | 0.18 mm in diametter | work with a plastic catheter to puncture aortic valves |
| Needle Holder | Shanghai Jinzhong | 131110 | suture of skin |
| Plastic Catheter | Anilab software & instruments | PE-0402 | work with a metal wire to puncture aortic valves |
| Pressure Catheter | Millar Instruments | SPR 835 | 1.4F in size |
| Pressure Data Acquisition Device and Analog/Digital Converter | AD Instruments | Labchart 5 | connected with pressure catherter |
| Scissor | Suzhou Shiqiang | Stronger 13Cr | to cut skin |
| Smallpinch Scissors | Shanghai Jinzhong | YBE030 | to cut vessel |
| Stereomicroscope | Olympus Corporation | SMZ845 | for incision and intubation of vessel |
| Straight Tying forceps | 66 Vision Tech | 53320A | to stretch and isolate muscle, tissue, and vessel |
| Thumbforceps | Suzhou Shiqiang | 5307B | to clamp and stretch skin and muscle |
| Ultrasound Gel | PARKER | Aquasonic-100 | to transfer ultrasound signal |
| Ultrasound Imaging System | VisualSonics | 2100 | includes B-mode, M-model, color Doppler and pulse wave Dopper |
| Vaporizer | RWD Life Science | R540 | for anesthesia |
References
- You, J., et al. Differential cardiac hypertrophy and signaling pathways in pressure versus volume overload. American Journal of Physiology. Heart and Circulatory Physiology. 314 (3), 552-562 (2018).
- Wu, J., et al. Variations in energy metabolism precede alterations in cardiac structure and function in hypertrophic preconditioning. Frontiers in Cardiovascular Medicine. 7, 602100 (2020).
- Houser, S. R., et al. Animal models of heart failure: a scientific statement from the American Heart Association. Circulation Research. 111 (1), 131-150 (2012).
- Pilz, P. M., et al. Large and small animal models of heart failure with reduced ejection fraction. Circulation Research. 130 (12), 1888-1905 (2022).
- Bartelds, B., et al. Differential responses of the right ventricle to abnormal loading conditions in mice: pressure vs. volume load. European Journal of Heart Failure. 13 (12), 1275-1282 (2011).
- Badheka, A. O., et al. Trends of hospitalizations in the United States from 2000 to 2012 of patients >60 Years with aortic valve disease. The American Journal of Cardiology. 116 (1), 132-141 (2015).
- Wu, J., et al. Left ventricular response in the transition from hypertrophy to failure recapitulates distinct roles of Akt, β-arrestin-2, and CaMKII in mice with aortic regurgitation. Annals of Translational Medicine. 8 (5), 219 (2020).
- Qi, Y. F. Aortic regurgitation and heart valve disease in mice. Journal of Thoracic Disease. 7 (10), 1676-1677 (2015).
- Zhou, Y. Q., Zhu, S. N., Foster, F. S., Cybulsky, M. I., Henkelman, R. M. Aortic regurgitation dramatically alters the distribution of atherosclerotic lesions and enhances atherogenesis in mice. Arteriosclerosis, Thrombosis, and Vascular Biology. 30 (6), 1181-1188 (2010).
- Michel, L., et al. Real-time pressure-volume analysis of acute myocardial infarction in mice. Journal of Visualized Experiments. (137), e57621 (2018).
- Wu, J., et al. Early estimation of left ventricular systolic pressure and prediction of successful aortic constriction in a mouse model of pressure overload by ultrasound biomicroscopy. Ultrasound in Medicine & Biology. 38 (6), 1030-1039 (2012).
- Li, L., et al. Assessment of cardiac morphological and functional changes in mouse model of transverse aortic constriction by echocardiographic imaging. Journal of Visualized Experiments. (112), e54101 (2016).
- Toischer, K., et al. Cardiomyocyte proliferation prevents failure in pressure overload but not volume overload. Journal of Clinical Investigation. 127 (12), 4285-4296 (2017).
- Patten, R. D., Aronovitz, M. J., Bridgman, P., Pandian, N. G. Use of pulse wave and color flow Doppler echocardiography in mouse models of human disease. Journal of the American Society of Echocardiography. 15 (7), 708-714 (2002).
- Nakanishi, M., et al. Genetic disruption of angiotensin II type 1a receptor improves long-term survival of mice with chronic severe aortic regurgitation. Circulation Journal. 71 (8), 1310-1316 (2007).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved