Method Article
An Effective Surgical Strategy for Anteromedial Osteoarthritis of the Knee with Simultaneous Popliteal Cysts Drainage
In This Article
Summary
Popliteal cysts are frequently found during the pre-operative examination of patients with osteoarthritis being prepared for the unicompartmental knee arthroplasty. These symptomatic cysts usually require treatment. To do this, a unicompartmental knee arthroplasty was performed with internal drainage of the popliteal cyst under the same anesthetic.
Abstract
Unicompartmental knee arthroplasty (UKA) is an established treatment option for anteromedial osteoarthritis, and popliteal cysts are a common finding in the knee among patients with chronic osteoarthritis pain. The two are so closely related that popliteal cysts are commonly discovered during the unicompartmental knee arthroplasty preoperative examination. However, only a few reports exist on the management and outcome of popliteal cysts in the patients receiving UKA for knee osteoarthritis (OA) and popliteal cysts. As such, it is crucial to evaluate different treatment strategies and their management of popliteal cysts. In this paper, we evaluate a surgical strategy for patients with knee anteromedial osteoarthritis and symptomatic popliteal cysts. These patients were treated with UKA and internal drainage of the popliteal cyst. The results shown here, spanning 1-year post-operation follow-up, demonstrated that UKA and internal drainage is an effective surgical protocol for treating anteromedial osteoarthritis with symptomatic popliteal cysts.
Introduction
A popliteal cyst is a mass located in the popliteal area, filled with fluid, which is prevalent in locations of intra-articular lesions of the knee1. Multiple reports suggest a strong correlation between popliteal cysts and knee osteoarthritis (OA)2,3. As a result, ~20%-42% of patients with knee OA also experience popliteal cysts1,3,4,5,6,7,8. Most of the cysts are rarely symptomatic and do not generally require therapy, while the symptomatic cysts warrant surgical resection9.
Unicompartmental knee arthroplasty (UKA) is widely used in the treatment of anteromedial knee OA10,11. Popliteal cysts are commonly discovered during the UKA preoperative examination. However, only a few reports exist on the management and outcome of popliteal cysts in patients that received UKA for knee OA and popliteal cysts. This article describes a protocol on how to treat popliteal cysts together with UKA.
Protocol
The present study was approved by the ethics committee of Second Hospital of Shanxi Medical University and all the patients provided written informed consent.
1. Inclusion and exclusion criteria for patients
- Use the following inclusion criteria.
- Select patients diagnosed with anteromedial osteoarthritis of the knee where conservative treatment failed. Diagnose anteromedial osteoarthritis of the knee by anteroposterior x-ray, based on a narrowed medial compartment of the knee but a normal lateral compartment.
- Verify the presence of an intact anterior cruciate ligament using clinical and intraoperative assessments. Identify the anterior cruciate ligament through preoperative magnetic resonance imaging (MRI) and a negative sign in the anterior drawer test; then, verify its integrity intraoperatively by probing with the hook instrument. An intact anterior cruciate ligament is a prerequisite for the patients undergoing UKA.
- Select patients having a <10° flexion contracture. Flexion contracture means that the knee is unable to fully extend to 0°, either actively or passively.
- Select patient with a >90° range of motion (ROM) of the knee. It is also a prerequisite for the patients undergoing UKA.
- Select patients diagnosed with popliteal cysts after ultrasonography and MRI examinations.
- With the ultrasound, identify a popliteal cyst as a well-defined and unilocular collection of anechoic or hypoechoic fluid between the tendons of the medial head of the gastrocnemius and semimembranosus.
- With the MRI, identify a popliteal cyst as a delineated mass with low signal intensity on the T1-weighted image, high signal intensity on the proton density-weighted fat saturation image, and a fluid-filled neck of the cyst communicating with the joint on the axial images.
- Classify popliteal cysts based on the Rauschning and Lindgren (R-L) knee grade, which is used to evaluate the severity of popliteal cysts12. Based on the R-L knee grade, classify the cysts as grade 0, grade I, grade II, and grade III. Select pre-operative grade II, and grade III cysts, which are symptomatic, for treatment.
- Use the following inclusion criteria.
- Exclude patients with a history of prior knee joint surgery.
- Exclude patients diagnosed as having asymptomatic popliteal cysts.
- Exclude patients who dropped out of follow-up or patient with incomplete follow-up data.
2. Surgical techniques
NOTE: The same group of surgeons conducted all the operations included in the study. Moreover, ensure that all the participants underwent the standard Oxford UKA surgical procedure with spinal anesthesia10. In case of a symptomatic popliteal cyst, Oxford UKA was performed, along with internal drainage of the popliteal cyst before implantation of the Oxford phase III medial unicondylar knee prosthesis. Perform the internal draining of the popliteal cyst as described below.
- Sedate the patient with spinal anesthesia as per the standard operating procedure. Ensure complete loss of sensation below the patient's waist to confirm proper anesthetization.
- Use an oscillating saw blade to excise the plateau. Lever the plateau up with a broad osteotome and remove it. Identify a wide space between the tibia and the femur following which the internal exit of the cyst can be visualized (Figure 1).
- Open the internal exit of the cyst to 5-8 mm with a knife. This will help in widening and clearing the communication between the joint and the cyst and restore the bidirectional fluid flow.
- Squeeze the popliteal cyst by hand outside the skin until all the viscous cyst fluid flows into the joint cavity through the exit of the cyst. Draw out the remaining cyst fluid by applying 30 kPa of negative pressure.
- Mill the femoral condyle using the number of spigots required by the ligament balancing technique and a spherical cutter. Cement the prosthesis sequentially from the tibial side to the femoral side when the trial implantation test is satisfactory. Complete the reconstruction by snapping the chosen bearing into place and the procedure is ended.
3. Postoperative rehabilitation
- Ask the patients to perform straight-leg raises and isometric exercises on the first day after surgery. To improve the knee function, ask the patients to perform full weight-bearing exercises, including standing and walking slowly with the assistance of a walker, 2 days after operation.
- For postoperative analgesia, ensure that all the patients receive postoperative administration of 40 mg of parecoxib intravenously every 8 h. To prevent blood clots, give patients anticoagulant therapy with a 10 mg dose of rivaroxaban daily at day 1 to 2 weeks post operation.
4. Efficacy evaluation
- Obtain a visual analog scale (VAS) score for all the patients13. Use the VAS score to indicate the degree of pain by asking the patient to make a mark on the horizontal line according to their feeling: 2-4 points represent mild pain, 5-7 points represent moderate pain, and 8-9 points represent severe pain.
- Obtain a hospital for special surgery (HSS) score for all the patients14. The HSS score mainly includes six aspects of pain, function, joint mobility, muscle strength, knee flexion deformity, and knee stability. Classify the score as follows: >85 as excellent, 70-84 as good, 60-69 as fair, and <59 as poor.
- Obtain a Western Ontario and McMaster Universities Arthritis Index (WOMAC) score for all the patients15. The WOMAC score assesses the knee through three domains: pain, stiffness, and joint function. Scores range from 0 to 96 for the total WOMAC, where 0 represents the best health status and 96 the worst possible status. The higher the score, the poorer the function.
- Assign a Rauschning and Lindgren (R-L) knee grade12 to evaluate the severity of the popliteal cysts. Based on the R-L knee grade, classify the cysts as grade 0, grade I, grade II, and grade III as described below.
- Grade a cyst as 0 for no swelling or pain, no limitation of range of motion, no instability or weakness, and no limitation in work or sports participation.
- Grade a cyst as I for slight swelling and discomfort after strenuous exercise, some giving-way or weakness, muscular atrophy of <1 cm, negligible limitation of range of motion (<10°), no hard labor, and no strenuous sports such as athletics or a ball game.
- Grade a cyst as II for moderate swelling, pain following moderate exertion, slight or moderate instability, locking, and muscular atrophy of 1-2 cm, limitation of range of motion between 10° and 20°, no physical work, limited participation in sports.
- Grade a cyst as III for considerable and tense swelling, severe pain interfering with activities of daily living, pain at rest, disabling instability, contractures, and muscular atrophy of >2 cm, limitation of range of motion >20°, stopped working due to knee derangement, no participation in sports.
Results
Clinical evaluation
Each patient was followed up for at least 1 year after the operation. At 1 year postoperatively, the postoperative VAS score significantly decreased from 7.0 ± 0.9 to 0.6 ± 0.7 (P < 0.05); the HSS score improved from 48.3 ± 8.5 preoperatively to 87.8 ± 4.6 (P < 0.05); and the WOMAC score decreased from 56.0 ± 9.6 preoperatively to 11.6 ± 5.0 (P < 0.05). The symptoms of popliteal cysts were instantly relieved for all the eight patients after recovery from anesthesia. Six patients (75%) had a R-L grade of 0, and two patients (25%) had a grade of l; popliteal cysts disappeared in 7 patients (87.5%) and decreased in 1 patient (12.5%) at 1 year postoperatively (Table 1).
Typical case analysis
Case 1
A 75-year-old male was presented to the hospital with medial-sided left knee pain. The major complaints were knee pain, swelling and pain in the popliteal fossa after soft exercise, and the inability to participate in normal recreational activities. The images of the tests done on the knee are shown below (Figure 2). The diagnosis of anteromedial osteoarthritis of the knee showed the presence of a symptomatic popliteal cyst (R-L grade ll) and was confirmed by studying the patient history and performing clinical examination, X-ray, and MRI. When the osteotomy of the femur and tibia were completed, the connecting opening to the cyst was located and enlarged with a knife (Figure 2C). Then, the Oxford phase III medial unicondylar knee prosthesis was implanted (Figure 2D).
Case 2
An 82-year-old man who complained of pain in the medial aspect of the knee, along with swelling and pain in the rest of the popliteal fossa was admitted to the hospital. Preoperative X-rays, MRI, and ultrasound confirmed that the patient had medial osteoarthritis of the knee combined with a symptomatic popliteal cyst (R-L grade lll). After careful preoperative assessment, it was clear that UKA alone would not adequately relieve the symptoms. Finally, under the same anesthetic, Oxford unicompartmental knee arthroplasty and internal drainage of the popliteal cyst were performed. The symptoms of popliteal cysts were instantly relieved after recovery from anesthesia. A good functional outcome was presented after 1 year of follow up (Figure 3).
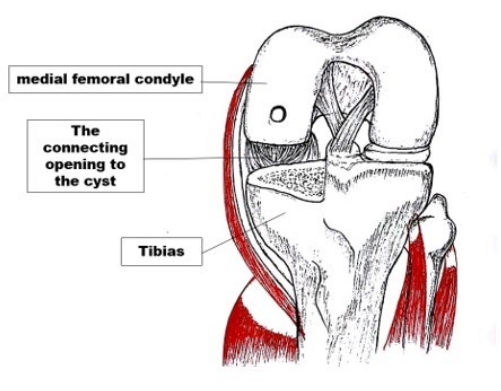
Figure 1: Finding the intra-articular opening of the cyst. The connecting opening can be identified when the osteotomy of the tibia was completed. The opening is so conspicuous that it can be seen with the naked eye. Please click here to view a larger version of this figure.

Figure 2: Photo of Case 1. (A) The anterior-posterior radiograph showed medial compartment degenerative joint disease. (B) The axial view in the MRI showed a popliteal cyst preoperatively (red arrow). (C) The location of the connecting opening to the cyst can be identified under direct vision after the completion of the osteotomy of the femur and tibia in the UKA (black arrow). (D) The postoperative anterior-posterior radiograph showed proper implant placement. Please click here to view a larger version of this figure.
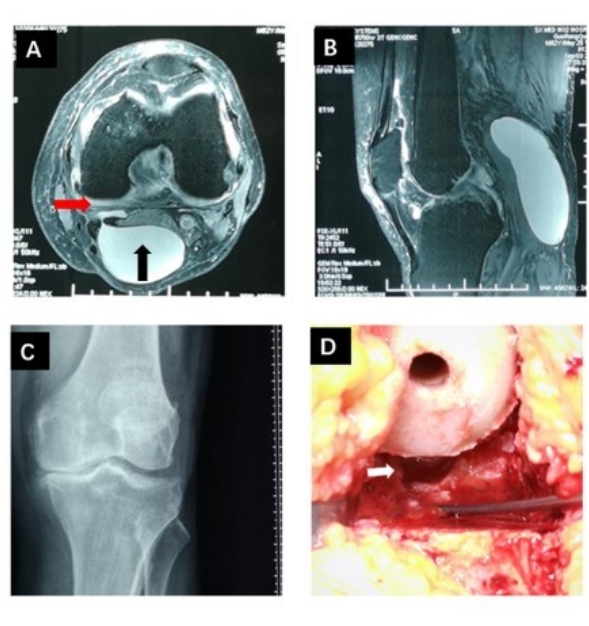
Figure 3: Photo of case 2. (A,B) The axial and sagittal MRI showed a giant popliteal cyst preoperatively (black arrow) and the connecting opening to the cyst can be seen (red arrow). (C) The AP radiograph showing the degenerative joint disease in the medial compartment. (D) The location of the connecting opening to the cyst can be dilated with the use of a knife (white arrow). Please click here to view a larger version of this figure.
| Before Surgery | 1-year follow-up | P | |
| VAS | 7±0.9 | 0.6±0.7 | <0.0001 |
| HSS | 48.3.0±8.5 | 87.8±4.6 | <0.0001 |
| WOMAC | 56.0±9.6 | 11.6±5.0 | <0.0001 |
| Rauschning-Lindgren grade | <0.0001 | ||
| Grade 0 | 0 | 6 | |
| Grade I | 0 | 2 | |
| Grade II | 6 | 0 | |
| Grade III | 2 | 0 |
Table 1: Scores before and after surgery. The table shows a significant improvement in the post-operative scores as compared to the pre-operative scores.
Discussion
A popliteal cyst, otherwise known as a Baker's cyst, is the knee joint disorder that is prevalent among the middle-aged and older population16,17. The incidence of popliteal cysts, in combination with symptomatic knee joint disease, is between 9.2% to 38%, depending on the location and the analysis18,19,20. Approximately 20%-42% of the patients with knee OA also have popliteal cysts1,3,4,5,6,7,8. In the field of sports medicine, most academics have denoted grade ll and lll as indicators for surgery while grade 0 and l are denoted as popliteal cysts that can be managed with observation and reassurance. Hommel et al.21 demonstrated that the prevalence of popliteal cysts, detected using ultrasound, was 9.2% among 1,508 patients with end-stage OA undergoing total knee arthroplasty (TKA) treatment. Unlike in this study, the popliteal cyst in the Hommel et. al. study was not treated. As a result, 85.3% of the patients who underwent TKA still had popliteal cysts whereas 35.6% of the patients experienced pain or other symptoms associated with the cysts at the 1-year follow-up. Despite the lack of accurate statistics, we have also seen some patients in the clinic with symptomatic popliteal cysts after UKA. Therefore, the surgical technique we report can be useful to avoid symptomatic popliteal cysts after UKA.
Historically, open excision of the popliteal cyst is the most common treatment method. However, in patients requiring end-stage OA knee replacement operation (TKA or UKA), the popliteal cyst is not normally addressed. This is because an open excision of the cyst requires placing the patients in a prone position to perform a posterior approach. Unfortunately, this strategy may exacerbate wound complications, calf swelling, and deep vein thrombosis22. In the Lindegren et al.23 study, the high popliteal cyst recurrence rate resulted from persistent intra-articular lesions and related recurrent effusion. Yet another strategy to correct unidirectional valve diseases is to expand the cyst opening under arthroscopy. This strategy was shown to have a 95% success rate5,24,25. Thus, the cyst opening/enlargement surgery can be considered an effective strategy to remove the popliteal cysts24,26,27,28,29. As previously reported, it is crucial to remove the one-way valve of the cyst cavity and the gastrocnemius tunica musculoskeletal bursa in order to promote a two-way circulation of the joint fluid30. Although the aforementioned techniques were only described arthroscopically, we combined Oxford UKA with internal drainage of the popliteal cyst, in the approach described here.
We performed the internal drainage of the popliteal cyst before the Oxford UKA prosthesis implantation. The cyst opening that connects to the joint was identified under direct vision right below the crease of the posterior knee upon osteotomy of the femur and tibia. This opening was then expanded with a knife to provide a two-way joint fluid flow without arthroscopy. The study reported a high success rate where popliteal cysts disappeared in seven patients (87.5%) and decreased in one patient (12.5%) at 1-year postoperatively and all the symptomatic popliteal cysts were instantly relieved post operation. There is a possibility that the cleaning of the posterior soft tissue during the operation may inadvertently eliminate the one-way valve mechanism that forms the fossa cyst,but this cannot be controlled, and excessive clearance of the posterior soft tissues may bring about potential complications. There were no complications in the eight cases presented above, but less experienced surgeons should pay more attention because the cyst is close to the popliteal vessels and nerves.
The limitations of this study are as follows. The study has a small sample size and a short follow-up period in the case of all the patients. In future studies, a larger sample size and a longer follow-up period must be included for assessing the effectiveness of the surgeries. There is no postoperative MRI to compare with the preoperative MRI. Additionally, the current study lacks a control group where patients with unicompartmental knee OA, in combination with symptomatic popliteal cysts, were treated with UKA alone.
Disclosures
The authors have nothing to disclose.
Acknowledgements
This research was supported by a grant from the Fund Program for the Scientific Activities of Selected Returned Overseas Professionals in Shanxi Province (grant number: 20210008).
Materials
| Name | Company | Catalog Number | Comments |
| Excel | Microsoft | digital table software | |
| Magnetic resonance inspection (MRI) | General Electric Company | Imaging examination of popliteal cyst before and after surgery. | |
| Oxford® Partial Knee surgery system | ZIMMER BIOMET | NONE | For the catalog numbers refer to Oxford Partial Knee Microplasty Instrumentation (femoral component, tibial component, meniscus bearing) |
| ultrasound | General Electric Company | we used ultrasound to observe changes in the postoperative cysts |
References
- Liao, S. -. T., Chiou, C. -. S., Chang, C. -. C. Pathology associated to the Baker's cysts: a musculoskeletal ultrasound study. Clinical Rheumatology. 29 (9), 1043-1047 (2010).
- Jiang, J., Ni, L. Arthroscopic internal drainage and cystectomy of popliteal cyst in knee osteoarthritis. Journal of Orthopaedic Surgery and Research. 12 (1), 1-6 (2017).
- Razek, A. A. K. A., El-Basyouni, S. R. Ultrasound of knee osteoarthritis: interobserver agreement and correlation with Western Ontario and McMaster Universities Osteoarthritis. Clinical Rheumatology. 35 (4), 997-1001 (2016).
- Rupp, S., Seil, R., Jochum, P., Kohn, D. Popliteal cysts in adults. Prevalence, associated intraarticular lesions, and results after arthroscopic treatment. American Journal of Sports Medicine. 30 (30), 112-115 (2002).
- Gu, H., Bi, Q., Chen, J. Arthroscopic treatment of popliteal cyst using a figure-of-four position and double posteromedial portals. International Orthopaedics. 43 (6), 1503-1508 (2019).
- Johnson, L. L., Van Dyk, G. E., Johnson, C. A., Bays, B. M., Gully, S. M. The popliteal bursa (Baker\"s cyst): An arthroscopic perspective and the epidemiology. Arthroscopy: The Journal of Arthroscopic & Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 13 (1), 66-72 (1997).
- Bui-Mansfield, L. T., Youngberg, R. Baker's cyst. Magnetic Resonance Imaging (MRI). 5, 18 (2009).
- Fam, A., Wilson, S., Holmberg, S. Ultrasound evaluation of popliteal cysts on osteoarthritis of the knee. The Journal of Rheumatology. 9 (3), 428-434 (1982).
- Zhang, M., et al. Arthroscopic internal drainage with cyst wall resection and arthroscopic internal drainage with cyst wall preservation to treat unicameral popliteal cysts: A retrospective case-control study. Orthopaedic Surgery. 13 (4), 1159-1169 (2021).
- Murray, D. W., Parkinson, R. W. Usage of unicompartmental knee arthroplasty. Bone & Joint Journal. 100 (4), 432 (2018).
- Wal Hamilton, T., et al. Evidence-based indications for mobile-bearing unicompartmental knee arthroplasty in a consecutive cohort of thousand knees. The Journal of Arthroplasty. 32 (6), 1779-1785 (2017).
- Rauschning, W., Lindgren, P. G. Popliteal cysts (Baker's cysts) in adults. I. Clinical and roentgenological results of operative excision. Acta Orthopaedica Scandinavica. 50 (5), 583-591 (1979).
- Crichton, N. Information point: Visual analogue scale (VAS). Journal of Clinical Nursing. 10 (5), 706 (2001).
- Bach, C. M., et al. Scoring systems in total knee arthroplasty. Clinical Orthopaedics and Related Research. 399 (1976-2007), 184-196 (2002).
- Ackerman, I. Western ontario and mcMaster universities osteoarthritis index (WOMAC). Australian Journal of Physiotherapy. 55 (3), 213 (2009).
- Baker, W. On the formation of synovial cysts in the leg in connection with disease of the knee joint. Clinical Orthopaedics and Related Research. (299), 2-10 (1877).
- Herman, A. M., Marzo, J. M. Popliteal cysts: a current review. Orthopedics. 37 (8), 678-684 (2014).
- Johnson, L. L., Van Dyk, G. E., Johnson, C. A., Bays, B. M., Gully, S. M. The popliteal bursa (Baker's cyst): an arthroscopic perspective and the epidemiology. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 13 (1), 66-72 (1997).
- Sansone, V., De Ponti, A., Paluello, G. M., Del Maschio, A. Popliteal cysts and associated disorders of the knee. International Orthopaedics. 19 (5), 275-279 (1995).
- Sansone, V., de Ponti, A., Paluello, G. M., del Maschio, A. Popliteal cysts and associated disorders of the knee. Critical review with MR imaging. International Orthopaedics. 19 (5), 275-279 (1995).
- Hommel, H., Becker, R., Fennema, P., Kopf, S. The fate of Baker's cysts at mid-term follow-up after total knee arthroplasty. The Bone & Joint Journal. 102 (1), 132-136 (2020).
- Rauschning, W., Lindgren, P. G. Popliteal cysts (Baker's cysts) in adults: I. Clinical and roentgenological results of operative excision. Acta Orthopaedica Scandinavica. 50 (5), 583-591 (1979).
- Lindgren, P. G., Willen, R. Gastrocnemio-Semimembranosus bursa and its relation to the knee joint: I. Anatomy and histology. Acta Radiologica: Diagnosis. 18 (5), 497-512 (1977).
- Ohishi, T., et al. Treatment of popliteal cysts via arthroscopic enlargement of unidirectional valvular slits. Modern Rheumatology. 25 (5), 772-778 (2015).
- Takahashi, M., Nagano, A. Arthroscopic treatment of popliteal cyst and visualization of its cavity through the posterior portal of the knee. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 21 (5), 638 (2005).
- Sansone, V., De Ponti, A. Arthroscopic treatment of popliteal cyst and associated intra-articular knee disorders in adults. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 15 (4), 368-372 (1999).
- Ahn, J. H., Lee, S. H., Yoo, J. C., Chang, M. J., Park, Y. S. Arthroscopic treatment of popliteal cysts: clinical and magnetic resonance imaging results. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 26 (10), 1340-1347 (2010).
- Jin, H. C. Clinical results of direct arthroscopic excision of popliteal cyst using a posteromedial portal. Knee Surgery & Related Research. 24 (4), 235-240 (2012).
- Ujjval, D., Harshvardhan, J., Chetan, R., Loya, N. Arthroscopic treatment of popliteal cyst and visualization of its cavity through the posterior portal of the knee. National Journal of Integrated Research in Medicine. 1 (1), 25-29 (2010).
- Herman, A. M., Marzo, J. M. Popliteal cysts: a current review. Orthopedics. 37 (8), 678 (2014).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionThis article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved